Food Poisoning Outbreak caused by Bacillus Cereus at a Secondary School in Mukono District, Uganda, July 2023
Authors: Benigna G. Namara1*, Innocent Semanda1, Anthony Kiyimba1, Dorothy Aanyu1, Arnold Taremwa1, John Mary Lutwama1, Valeria Eugenia Nawajje1, Benon Kwesiga1, Alex Riolexus Ario1; Institution affiliations, 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda; Correspondence*: Tel: +256782882261, Email: benignamara@uniph.go.ug
Summary
Introduction: Bacillus cereus is a foodborne bacterial pathogen that causes abdominal pain and diarrhoea; incubation is typically 4-16 hours. On July 20, 2023, the Ministry of Health was notified of a suspected food poisoning outbreak at a secondary school in Mukono District, Uganda, following an alert about students with sudden-onset abdominal pain and diarrhoea. We investigated the incident and recommended control measures.
Methods: We defined a case as ‘sudden onset of abdominal pain, diarrhoea or vomiting in a student or staff member at the school’ from July 19–20, 2023. We found cases by reviewing school and health facility records and created a line-list. We subjected cases to a questionnaire and conducted descriptive epidemiology and environmental assessments. We tested our hypothesis in a cohort of all boarding students.
Findings: Among 267 cases (all students), 13% were commuters and 87% were boarders. The most common symptoms included abdominal pain (100%), diarrhoea (92%), and vomiting (16%). The epidemic curve indicated a point-source outbreak with onsets occurring 6-36 hours after eating school lunch or dinner. Posho and beans from the same bags were cooked and consumed on preceding days with no illness reported, suggesting that the food was contaminated during preparation on that day. Nearly all 299 cohort members ate the food for lunch and/or dinner on July 19. Zero (0%) of the 4 students who ate neither meal and 229 (78%) of 295 students who ate the school lunch and/or dinner and became ill (RR=0.13; 95% CI 0.01-1.8). Attack rates were 90% for those who ate only lunch, 77% only dinner and 78% who ate both. Bacillus cereus was isolated from leftover samples of the cooked food.
Conclusion: This was a point-source outbreak caused by Bacillus cereus in food cooked at school; mechanism of contamination was unknown. Proper food handling, preparation, and storage were emphasized to prevent repeat occurrences.
Background
Food poisoning is a common public health problem that can cause serious illness or even death. According to the World Health Organization, food poisoning affects an estimated 600 million people and kills 420,000 people every year (1).
Food poisoning can be caused by various biological, chemical, or physical agents that contaminate food during production, processing, distribution, or preparation. Some of the common symptoms of food poisoning include nausea, vomiting, diarrhea, abdominal cramps, fever, and headache(2).
In Africa, several outbreaks of food poisoning have been documented and it is estimated that 92 million people suffer from food poisoning after consuming contaminated foods resulting in 137 000 deaths each year.(3,4) The most common food poisoning causes are bacteria such as Salmonella, Escherichia coli, Staphylococcus aureus and Bacillus cereus(5). These bacteria can be found in foods such as meat, eggs, dairy products, and vegetables.
In Uganda, food poisoning is a major public health concern that affects many people every year. In 2019, deaths due to food poisoning by alkaloids and outbreaks of food poisoning by chemical agents were reported in Uganda (6,7) . Some of the risk factors for food poisoning in Uganda include poor hygiene practices, inadequate cooking methods, improper storage conditions, and lack of awareness among consumers(8).
On Thursday, July 20th, 2023, the Ministry of Health was notified of a suspected food poisoning outbreak at a secondary school in Mukono district, Uganda. The alert followed several students from the school complaining of a sudden onset of abdominal pain and diarrhoea. The school comprises of day and boarding sections with approximately 300 students in the boarding section many of whom developed symptoms suggestive of food poisoning and were evacuated to the nearby health facilities for treatment. We investigated to determine the scope, cause, risk factors for the outbreak and provide recommendations for remedial action.
Methods
Outbreak location
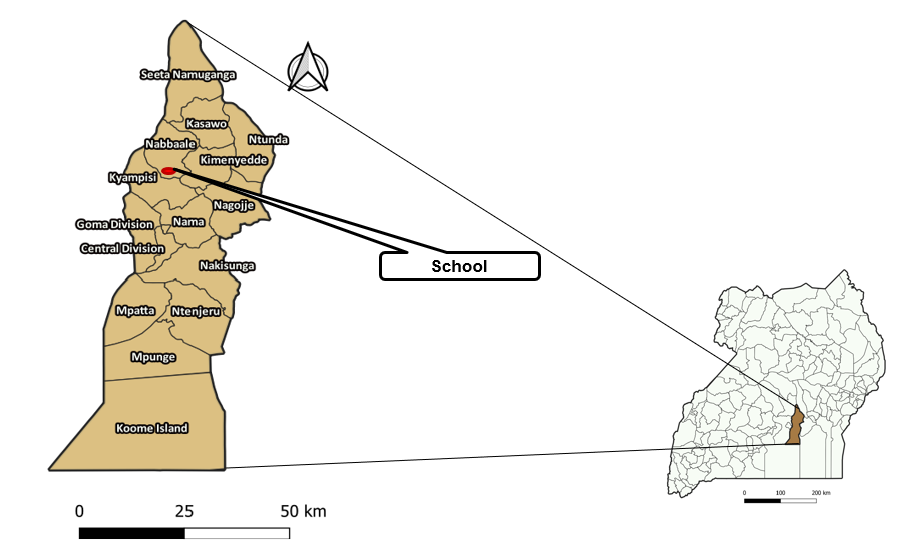
The investigation took place at the secondary school in Mukono District where the outbreak took place (Figure 1). The school is comprised of both boarding and day sections with a population of approximately 300 boarding students and 900 day scholars(commuters) respectively.
Case definition and finding
We defined a suspected case as sudden onset of abdominal pain, diarrhoea or vomiting in a student or staff member at the school’ from July 19–20, 2023.
We found cases using records of sick children from both the school and the health facilities to which the students were evacuated and generated a line-list. A case investigation form was administered to case-patients on the line-list. The case investigation form included questions about demographic and clinical characteristics of the cases including age, sex, class, scholar type, date and time of symptom onset and gastrointestinal symptoms.
Descriptive analysis
We described case-patients by time using an epidemiologic curve and by person using attack rates by class, dormitory, and sex.
Laboratory Investigations
Samples both clinical (10 stool and 52 blood) and non-clinical (cooked beans and posho from the kitchen; flour, water, cooking oil, tomatoes from the food stores; and collard greens from the garden) were collected for laboratory testing. Clinical samples including stool and blood were taken from students while non-clinical samples were taken from the food stores, kitchen, and the vegetable garden.
Environmental assessment
We did this using both direct observation and interviews with the food handlers. We explored the food supply, storage facilities, preparation and the water source. We directly observed the process of food preparation, storage, and distribution at the school in order to identify possible sources of contamination. We inspected the reservoirs from which the students get their water in order to determine possible sources of contamination. We interviewed the food handlers about how, when, and from where they obtain the food, how it is prepared, how it is served, and stored also to assess for any possible risks for contamination.
Hypothesis generation
Using a structured questionnaire, we interviewed 93 case-persons to generate a hypothesis. We asked questions about possible exposures such as food, snacks, and drink the cases had been exposed to on the day of the outbreak and quantified the exposure to each of these.
Retrospective cohort study
To test the hypotheses, a cohort consisting of all boarding school students was constructed. This was because the day scholars had been temporarily sent home pending investigation into the outbreak. A structured electronic questionnaire was administered to all members of the cohort in order to assess exposure and outcomes of interest which were symptoms of food poisoning constituting the case definition. Risk ratios were calculated.
Ethical considerations
We conducted this study in response to a public health emergency and as such was determined to be non-research. The MoH authorized this study and the office of the Center for Global Health, US Center for Disease Control and Prevention determined that this activity was not human subject research and with its primary intent being for public health practice or disease control. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy. §
- See e.g., 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
We obtained permission to conduct the investigation from the Mukono District health authorities and the school administration in whose custody all the students were. We obtained verbal consent from all the respondents aged ≥18 years. For those aged <18 years, we obtained consent from the school administration and assent from the respondents. Participants were assured that their participation was voluntary and that there would be no negative consequences for declining to participate in the investigation. Data collected did not contain any individual personal identifiers and information was stored in password-protected computers, which were inaccessible by anyone outside the investigation team.
Results
Descriptive epidemiology
Of the 267 cases listed, 233(87%) were boarders and the rest were commuters. The most common symptom reported was abdominal pain among all (100%) of the cases followed by diarrhoea among 247 (92%) while vomiting was rare, among only 43(16%) of the cases
Females were more affected (Attack rate=85%) than males (Attack rate=64%).
The attack rates varied by class: with S4 having the highest (84%), S5(83%), S2(80%), S3(80%), S1(74%), and S6(53%). The attack rates also varied by dormitory with the three girls’ dormitories having attack rates of 76%, 63%, and 56% while the two boys’ dormitories had attack rates of 62% and 42%.
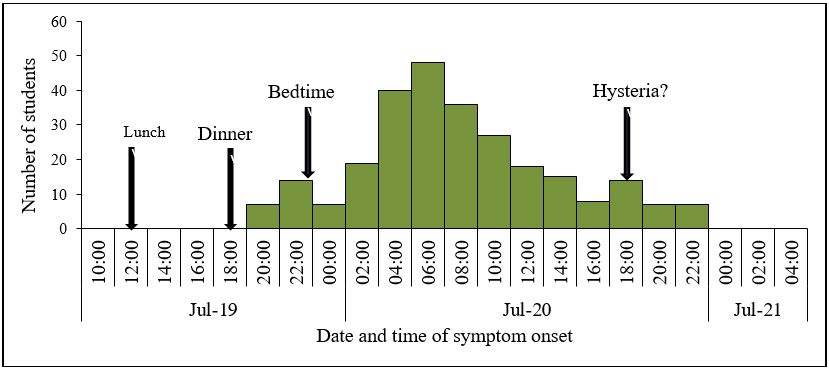
There was a rapid rise in the number of cases to a peak within twelve hours, and then a gradual fall over eighteen hours (Figure 2).
Environmental assessment findings
Food supply: The school stocks food every two weeks from one supplier who also supplies the neighbouring school and community. Existing stock had been consumed for several days prior to the outbreak with no illness events occurring. Food cooked on the day of the outbreak was from same sacks as that cooked on previous days still with no illness events occurring on those days.
Food storage: The food store was a small dark room with no ceiling, no windows, and no ventilation system. The sacks of posho are kept on pallets on the floor while the sacks of beans sit directly on a cemented floor. The kitchen is more open with adequate ventilation but with mud floors and bare mud bricks comprising the walls. Trace-back for the flour was deemed unnecessary given that the same batch of flour had been used in the previous days with no incident. The fact that there were no similar incidents reported in the neighbouring school and surrounding community which use flour from the same supplier further negated the usefulness of a trace-back.
Food preparation: Posho and beans were cooked daily in one go and eaten at both lunch and dinner. Food preparation starts at 2.00am in the morning of each day with the preparation of posho. When the posho is ready, the beans are boiled by the same cooks until 5.00am. At 8.00am, the raw vegetables are added depending on what is available. The food is then left on low heat throughout the day until lunch time when the first portion is served. What remains is then left on low heat until dinner time when they are consumed. According to the cooks, the food eaten on the day of symptom onset was prepared in the same way that food is normally prepared. There was no deviation from the norm.
Water source: Water is pumped from a protected deep well located about 1 kilometer away from the school. During pumping, it passes through a water purification system from which it is then distributed. The same water is used daily by three populations i.e. the secondary school, a neighbouring primary school and the community. There were no reports of related illness in the latter two.
Laboratory findings
Among the samples taken for lab testing: all stool samples were negative for parasites and bacteria. All blood samples were negative for pesticides, metals and aflatoxins. The tap water and vegetables tested negative for bacterial growth. Samples of left over posho and beans tested positive for Bacillus cereus.
Hypothesis generation
We explored possible risk factors including all food and drink consumed by the cases on that day (Table 2).
Table 2: Proportion of cases exposed to possible risk factor during the food poisoning outbreak at a secondary school in Mukono District, July 2023
| Exposure characteristic | Percentage exposed |
| Ate school food (posho &beans) -at least one meal on 19th July 2023 | 97% |
| Drank school water | 100% |
| Took tea at either lunch or dinner | 42% |
| Ate Snacks from canteen (cassava, donuts, etc) | 11% |
| Added flavoring(‘appetizer’) to their food | 8% |
Based on the table, the exposures of interest were food (posho & beans) eaten and water drunk. However, based on the environmental assessment, water was ruled out as the exposure since there were no reports of illness from the other consumers of the same water. We therefore hypothesized that food (posho and beans) consumed by the students on the 19th of July 2023 was responsible for the outbreak.
Retrospective cohort study
We constructed a cohort consisting of 299 boarding students. Among the cohort, 295(99%) had had at least one meal of posho and beans and of these, 229(78%) got sick. Among the 4(1%) that did not eat any meal, none got sick. We calculated the risk based on the exposure to food and stratified by number of meals eaten in order to assess for a dose response. The risk ratios did not vary significantly across strata likely due to the small numbers in some of the groups (Table 3).
Table 3: Level of risk among those who ate meals of posho and beans compared to those who did not prior to the food poisoning outbreak at a secondary school in Mukono District, July 2023
| Exposure | Sick Not sick | Total RR 95%CI |
| Did not eat 0 4 4 0.13 0.01-1.8
Ate lunch only 4 1 5 1.03 0.67-1.6 Ate dinner only 51 15 66 0.99 0.86-1.2 Ate lunch+dinner 174 50 224 Ref Total 229 70 299 |
||
Discussion
This was a point-source outbreak of food poisoning by Bacillus cereus, the source of which was undetermined. The outbreak presented as a diarrhoeal illness and there were no deaths. The food cooked on the day of the outbreak was from the same bags as that cooked on previous days where no illness events were reported, suggesting that contamination of the food occurred during preparation. Having at least one meal of posho and beans, either lunch or dinner, was the risk factor for developing illness.
Bacillus cereus is a gram-positive aerobic spore forming rod well known for causing food poisoning. It causes two syndrome types, the emetic and the diarrhoeal which present predominantly with vomiting or diarrhoea respectively and can occur independently(9,10). The emetic syndrome has a shorter incubation period(0 to 6 hours) while the diarrhoeal syndrome has a longer average incubation period of 8-16 hours(11,12). Based on our epi-curve, the timeline matched the diarrhoeal syndrome incubation period and given that diarrhoea was the main symptom, it makes sense that this was Bacillus cereus food poisoning with the diarrhoeal syndrome. Within 30 hours, there were no new cases or symptoms in keeping with reports that this illness is self-limiting and usually resolves within 48 hours (10).
This bacteria has been identified as a major cause of food poisoning in various parts of the world including East Africa presenting as either the emetic syndrome or diarrhoeal or both(9,13–16).In one outbreak in Australia, whole genome sequencing was done and only genes encoding the diarrhoeal toxin were found(17) while in another, 90% had diarrhoea while only 10% had vomiting(18) Although rarely fatal, some outbreaks of Bacillus cereus have registered fatalities from food poisoning caused by this organism, although most fatal outbreaks are usually from the emetic type of food poisoning which normally has more severe consequences(19,20)There were no fatalities in this outbreak which was the diarrhoeal type, in keeping with what is documented about the severity of the different syndromes. In another outbreak, a 7-year-old girl died 13 hours after having a meal contaminated with these bacteria and subsequently developing the emetic syndrome. Four of her siblings developed illness with the emetic syndrome but recovered.(19)
These bacteria often exist as spores in the environment which are able to contaminate raw foods, vegetables and even cooked food during preparation as we suspect is what happened in this outbreak. Under favorable conditions such as warm food, inadequate refrigeration of cooked food , these spores germinate to produce viable bacteria which grow and produce the toxins responsible for most cases of Bacillus cereus food poisoning(14). Given the nature of food preparation at the school whereby food is cooked in the early hours of the morning and then left on low heat throughout the day, it is possible that the bacteria were given ideal conditions to grow.
Although this pathogen is more commonly found in cases of food poisoning with cooked rice or rice products(12,17,21), it has also been documented severally in other types of food such as cooked beans and green salads(22,23). However, food poisoning outbreaks with foods other than rice as the source of Bacillus cereus have not been widely documented. Studies have documented the growth of Bacillus cereus biofilms on green leafy vegetables (22,24), which is why it is plausible that the collard greens which were added to the cooked beans might have been the source of contamination. However, the sample of collard greens taken from what was left over in the same garden as those cooked on that day reportedly tested negative for bacteria. Flour, especially maize flour is known to be an unfavorable growth medium for bacterial organisms due to its low-water activity, although contamination of wheat flour by Bacillus cereus spores has been documented(25,26). This points out the interesting finding of Bacillus cereus in one out of the four samples of flour.
The symptoms, timelines of symptom onset, duration of illness, environmental findings as well as the laboratory findings are all consistent with Bacillus cereus food poisoning making it plausible as the cause of this outbreak.
For the cases who did not eat any of the suspect food but reported symptoms, we suspect that this may have been a result of mass hysteria influenced by fellow students falling ill, worsened by the anxiety of the community and the presence of the media and police at the school. Mass hysteria is a well-documented occurrence in schools especially affecting girls, and can even mimic food poisoning(27–30).
Study limitations
There were more boarders than commuters among the cases listed possibly due to the fact that the school had been closed temporarily and day scholars suspended to allow for the investigation to take place. Some scholars however were still at the school at the time of the investigation and were identified as cases. The school has approximately 900 day scholars compared to approximately 300 boarders and these share the same meals at lunch. It is possible that there were more cases among the day scholars but these were managed at home.
Given the likely apprehension brought about by the involvement of political, media, and security personnel in the response to this outbreak, it is possible that the key informant recounts of events pertinent to the incident including the food preparation specifics were less than accurate. The team was therefore unable to determine the source of contamination of the food on that day.
Conclusion
Our investigation determined that there was an outbreak of Bacillus cereus food poisoning among students at the school on the 19th of July, 2023. This was probably as a result of contamination during handling and preparation of the food for that day but the source of contamination was not determine.
Recommendations and public health actions
Strict hygiene practices should be observed during handling and preparation of food. Vegetables must we washed thoroughly before cooking to remove any films of bacteria or toxins that may have formed on the leaves. Food must be kept hot or reheated adequately before serving in order to prevent germination of spores into viable organisms, or to destroy any viable organisms that may have grown while in storage at warm temperatures. The cooks were educated about food poisoning and best practices to prevent its occurrence.
Conflict of Interest
The authors declare that they had no conflict of interest.
Authors contribution
BGN: participated in the conception, design, analysis, interpretation of the investigation findings and wrote the draft bulletin.IS, AK, DA, AT, JML, VEN and BK reviewed the report. BK and ARA reviewed the bulletin to ensure intellectual content and scientific integrity.
Acknowledgments
The authors would like to thank the Mukono District health office and the management of the school for their support during this investigation.
Copyrights and licensing
All materials in the Uganda Public Health Bulletin is in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- WHO’s first ever global estimates of foodborne diseases find children under 5 account for almost one third of deaths [Internet]. [cited 2024 Jan 29]. Available from: https://www.who.int/news/item/03-12-2015-who-s-first-ever-global-estimates-of-foodborne-diseases-find-children-under-5-account-for-almost-one-third-of-deaths
- CDC. Centers for Disease Control and Prevention. 2023 [cited 2024 Jan 29]. Food Poisoning Symptoms. Available from: https://www.cdc.gov/foodsafety/symptoms.html
- World Health Organization: World Health Statistics… – Google Scholar [Internet]. [cited 2024 Mar 5]. Available from: https://scholar.google.com/scholar_lookup?title=World+health+statistics+2015&publication_year=2015&
- Idehen CN, Jiya MJ, Balogu VT. Food Poisoning in Africa: A Silent Epidemic in Recent Era of Global Food Traffic. DRJAFS. 2023 Feb 1;11(2):25–30.
- Malangu N. Risk Factors and Outcomes of Food Poisoning in Africa. In: Significance, Prevention and Control of Food Related Diseases [Internet]. IntechOpen; 2016 [cited 2024 Jan 29]. Available from: https://www.intechopen.com/chapters/49838
- Mutebi RR, Ario AR, Nabatanzi M, Kyamwine IB, Wibabara Y, Muwereza P, et al. Large outbreak of Jimsonweed (Datura stramonium) poisoning due to consumption of contaminated humanitarian relief food: Uganda, March–April 2019. BMC Public Health. 2022 Mar 30;22(1):623.
- Haughey SA, Chevallier OP, McVey C, Elliott CT. Laboratory investigations into the cause of multiple serious and fatal food poisoning incidents in Uganda during 2019. Food Control. 2021 Mar 1;121:107648.
- UPDATE ON FOOD POISONING INVESTIGATIONS IN KARAMOJA REGION [Internet]. Ministry of Health | Government of Uganda. [cited 2024 Jan 28]. Available from: https://www.health.go.ug/document/update-on-food-poisoning-investigations-in-karamoja-region/
- Granum PE, Lund T. Bacillus cereus and its food poisoning toxins. FEMS Microbiology Letters. 1997 Dec 1;157(2):223–8.
- Bacillus cereus [Internet]. [cited 2024 Mar 5]. Available from: http://www.bccdc.ca/health-info/diseases-conditions/bacillus-cereus
- Canada PHA of. Pathogen Safety Data Sheets: Infectious Substances – Bacillus cereus [Internet]. 2012 [cited 2024 Mar 5]. Available from: https://www.canada.ca/en/public-health/services/laboratory-biosafety-biosecurity/pathogen-safety-data-sheets-risk-assessment/bacillus-cereus.html
- Martinelli D, Fortunato F, Tafuri S, Cozza V, Chironna M, Germinario C, et al. Lessons learnt from a birthday party: a Bacillus cereus outbreak, Bari, Italy, January 2012. Ann Ist Super Sanità. 2013 Dec;49:391–4.
- Thery M, Cousin VL, Tissieres P, Enault M, Morin L. Multi-organ failure caused by lasagnas: A case report of Bacillus cereus food poisoning. Front Pediatr. 2022 Sep 14;10:978250.
- Midura T, Gerber M, Wood R, Leonard AR. Outbreak of food poisoning caused by Bacillus cereus. Public Health Rep (1896). 1970 Jan;85(1):45–8.
- Tewari A, Abdullah S. Bacillus cereus food poisoning: international and Indian perspective. J Food Sci Technol. 2015 May;52(5):2500–11.
- Lentz SAM, Rivas PM, Cardoso MR de I, Morales D de L, Centenaro FC, Martins AF. Bacillus cereus as the main casual agent of foodborne outbreaks in Southern Brazil: data from 11 years. Cad Saúde Pública. 2018 Mar 29;34:e00057417.
- Thirkell CE, Sloan-Gardner TS, Kacmarek MC, Polkinghorne B. An outbreak of Bacillus cereus toxin-mediated emetic and diarrhoeal syndromes at a restaurant in Canberra, Australia 2018. Commun Dis Intell (2018). 2019 Sep 16;43.
- Al-Abri SS, Al-Jardani AK, Al-Hosni MS, Kurup PJ, Al-Busaidi S, Beeching NJ. A hospital acquired outbreak of Bacillus cereus gastroenteritis, Oman. J Infect Public Health. 2011 Sep;4(4):180–6.
- Dierick K, Coillie EV, Swiecicka I, Meyfroidt G, Devlieger H, Meulemans A, et al. Fatal Family Outbreak of Bacillus cereus-Associated Food Poisoning. Journal of Clinical Microbiology. 2005 Aug;43(8):4277.
- Elise N, Cissé M, Souleymane B, Sindic M. A Review on Bacillus Cereus in Africa’s Locally Produced Foods. European Scientific Journal ESJ. 2019 Mar 31;15.
- Li T, Zou Q, Chen C, Li Q, Luo S, Li Z, et al. A foodborne outbreak linked to Bacillus cereus at two middle schools in a rural area of Chongqing, China, 2021. PLOS ONE [Internet]. 2023 [cited 2024 Mar 5];18(10). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10586640/
- Antequera-Gómez ML, Díaz-Martínez L, Guadix JA, Sánchez-Tévar AM, Sopeña-Torres S, Hierrezuelo J, et al. Sporulation is dispensable for the vegetable-associated life cycle of the human pathogen Bacillus cereus. Microb Biotechnol. 2021 Jul;14(4):1550–65.
- BLAKEY LJ, PRIEST FG. The Occurrence of Bacillus cereus in some Dried Foods Including Pulses and Cereals. Journal of Applied Bacteriology. 1980 Apr 1;48(2):297–302.
- Majed R, Faille C, Kallassy M, Gohar M. Bacillus cereus Biofilms-Same, Only Different. Front Microbiol. 2016;7:1054.
- Microbiology of Grains and Flours July 2021.pdf [Internet]. [cited 2024 Jan 29]. Available from: https://fri.wisc.edu/files/Briefs_File/Microbiology%20of%20Grains%20and%20Flours%20July%202021.pdf
- Kindle P, Etter D, Stephan R, Johler S. Population structure and toxin gene profiles of Bacillus cereus sensu lato isolated from flour products. FEMS Microbiology Letters. 2019 Oct 1;366(20):fnz240.
- Pfeiffer PH. MASS HYSTERIA MASQUERADING AS FOOD POISONING. J Maine Med Assoc. 1964 Feb;55:27.
- Ebrahim GJ. Mass Hysteria in School Children: Notes on Three Outbreaks in East Africa. Clin Pediatr (Phila). 1968 Jul 1;7(7):437–8.
- “The Wandering Womb”: Mass Hysteria in School Girls, 1968 [Internet]. [cited 2024 Jan 28]. Available from: https://journals.sagepub.com/doi/abs/10.1177/000992286800700701
30. Small GW, Borus JF. Outbreak of illness in a school chorus. Toxic poisoning or mass hysteria? N Engl J Med. 1983 Mar 17;308(11):632–5.

