Cholera outbreak associated with drinking contaminated river water in Kayunga District, Uganda, June–August 2023
Authors: Adams Kamukama1*, Edith Namulondo1, Yasini Nuwamanya 1, Leah Naluwagga Baliruno1, Irene Kyamwine1, Hildah Tendo Nansikombi1,3, Lilian Bulage1, Benon Kwesiga1, Alex Riolexus Ario1; Institutional affiliation: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda; *Correspondence: Tel: +256779314504, Email: akamukama@uniph.go.ug
Summary
Background: Cholera is endemic in Uganda with cases reported annually. On July 19, 2023, the Uganda Ministry of Health declared a cholera outbreak in Kayunga District following death of four family members within eight days and confirmation of Vibrio cholerae by culture. We investigated the outbreak to determine the magnitude, factors associated with cholera infection, and recommend control and prevention measures.
Methods: We defined a suspected case as onset of acute watery diarrhea during June 24–August 29, 2023 in a resident of Kayunga District aged ≥2 years. A confirmed case was a suspected case with Vibrio cholerae cultured from stool. We described cases and conducted an environmental assessment and an un-matched case-control study in Lusenke Village which was the epicenter of the outbreak. We analyzed data using logistic regression to identify factors associated with cholera infection.
Conclusion: This outbreak was likely a propagated outbreak initiated at a funeral of a suspected case whose source of infection was unknown and amplified through contamination of river water used and drank by village members. The outbreak ended within one week after prohibiting use of River Nile water and activities that contaminate river water among other control measures.
Background
Cholera is an acute diarrheal disease caused by the bacterium Vibrio cholerae. It presents with sudden onset of profuse watery diarrhea with or without abdominal discomfort, vomiting or dehydration. The disease affects both children and adults and can kill within hours if untreated. The case fatality rate in untreated cases may be as high as 30–50%; however, if well treated with rapid and sufficient rehydration, the case fatality rate can be reduced to as low as below 1% (1).
Vibrio cholerae occurs and persists in various aquatic systems such as lakes and rivers, and is transmitted via ingestion of contaminated water or food (2). The incubation period is between hours and 5 days (3). Inadequate clean water and poor sanitary conditions have been identified as the driving forces for the cholera epidemic (4,5).
The annual cholera burden is estimated to be between 1.3-4.0 million cases and 21,000-143,000 deaths globally with about 30% of the cases and 80% of the deaths occurring in Africa (6–8). Africa saw the highest burden of cholera outbreaks on record in 2021, with 19 countries reporting over 137,000 cases and 4,062 deaths (9). In Uganda, cholera outbreaks have continued to occur since 1971 when the disease was first reported (10). From 1997, cholera cases have been reported annually in Uganda, including a major epidemic that occurred in 1998, with nearly 50,000 reported cases (11,12). Border districts along the Democratic Republic of Congo, South Sudan, and Kenya borders are at high risk because of cross boarder transmission (13). In addition, areas lying along water bodies are prone to cholera outbreaks especially during rainy seasons when the water bodies get contaminated with fecal matter due to runoffs and flooding (14). Over 50% of the cholera cases in Uganda occur in the fishing villages (15). Majority of these communities live under high levels of poverty, poor hygiene conditions, and have poor access to safe water (15).
From 2015 ̶ 2021, 63 cholera outbreaks were reported in Uganda, affecting 43 districts, Kayunga District inclusive. In 2018 ̶ 2019, Kayunga District was reported as one of the cholera endemic districts in Uganda (13,16). On July 19, 2023, the Uganda Ministry of Health (MoH) declared a cholera outbreak in Kayunga District following death of four family members within eight days. Vibrio cholerae was cultured from two stool samples collected from the last two people who died. We investigated the outbreak to determine the magnitude, factors associated with cholera infection, and recommend control and prevention measures.
Methods
Outbreak area
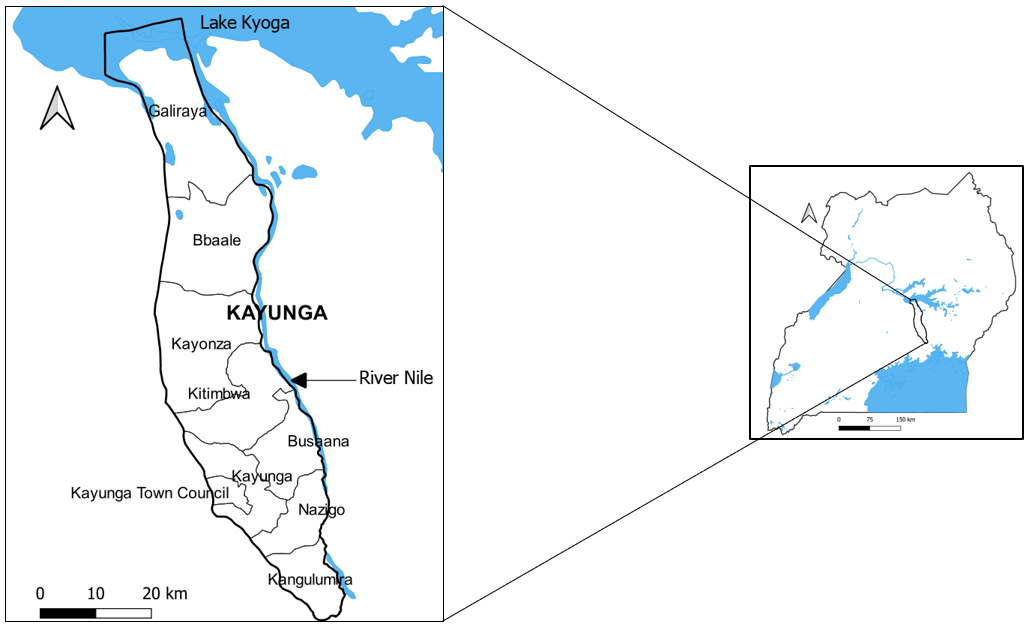
The outbreak occurred in Kayunga District, located in the North-central Region of Uganda (Figure 1). The district neighbors Lake Kyoga in the North and River Nile in the East, where there are fishing activities (17). Kayunga District has a population of approximately 427,100 people living in nine sub-counties (17,18). Sixty four percent of the population has access to safe drinking water (piped water, water from protected springs, and water from deep boreholes) and the district latrine coverage is 73% (19).
Case definition and finding
We defined a suspected case as onset of acute watery diarrhea during June 24–August 29, 2023 in a resident of Kayunga District aged ≥2 years. A confirmed case was a suspected case in which V. cholerae was isolated in stool by culture (20,21).
We interviewed health workers and reviewed records at Kayunga Regional Referral Hospital, Busaana heath center III, Namusaala heath center II, and five purposively-selected private health facilities to identify confirmed and suspected cases. The selected private health facilities were those in the epicenter subcounty or those with high volume of patients. In the community, we interviewed leaders and village health team (VHT) members and already identified case-patients, their caretakers and family members to direct us to other persons who had experienced diarrhea, vomiting or abdominal pain in the community. We then line listed the case-patients
Descriptive epidemiology
We calculated attack rates by place (district, subcounty, and village), age (grouped age into categories of 2-4, 5-14, 15-29, 30-59 and ≥60 years) and sex using the 2023 population estimates of persons aged two and above years obtained from Kayunga district biostatistician and Uganda Bureau of Statistics (UBOS).
Environmental assessment
We assessed the disposal of human excreta in communities and inspected the sources of water for drinking and domestic use in the most affected villages. We inspected for any possible sources of water contamination.
Laboratory investigations
We collected 107 stool samples from all suspected case-patients and rectal swabs from those who died from acute watery diarrhea. The samples were tested for V. cholerae by culture at Kayunga Regional Referral Hospital and Central Public Health Laboratory in Kampala. We collected water samples for bacteriological culture for V. cholerae: four samples from River Nile, two from boreholes, and two from solar pumped taps.
Eight water samples (four from River Nile, two from boreholes, two from solar pumped taps) were collected aseptically. Water samples from River Nile were collected along the shores where the community regularly fetched water. The samples were transported under cold chain conditions to the laboratory for testing.
Hypothesis generation
We interviewed the first 40 case-patients (identified by active case search), their family members, caretakers, community leaders and village health team (VHT) members. The interviews included questions about foods consumed, drinking water, history of recent travel, and funeral practices.
Case-control study
Because of logistical limitations, we conducted a case-control study using 25 cases (14 confirmed and 11 suspected) and 99 controls from Lusenke Village which was the most affected village in the most affected subcounty of Busaana (Figures 2&3). All case-patients identified in Lusenke Village by the time of the study were included in the case-control study. We defined a control as a resident of Lusenke Village, aged ≥2 years with no history of acute watery diarrhea during June 24–August 29, 2023. We listed all households that did not have any case in the village as control households. We systematically sampled control-households. One control-person was randomly selected from each sampled control-household using lottery method. We administered a standard questionnaire to both case and control-persons to obtain information on their demographics (age, sex), clinical characteristics (date of onset, signs and symptoms, seeking health care) and exposures (water sources, history of travel, attending funerals and preparation of drinking water). We analyzed data using logistic regression to generate odds ratios and 95% confidence intervals (CI) for factors associated with cholera infection. We stopped at bivariate analysis since most of the variables had counts less than five. However, we further conducted common reference group analysis for factors that were significant at bivariate level to assess the differences in the odds of infection based on combinations of the factors associated with cholera infection.
Ethics approval and consent to participate
This outbreak investigation was in response to a public health emergency and was instituted by the Uganda Ministry of Health. This investigation was also reviewed by the US CDC and was conducted consistent with applicable federal law and the US CDC policy. §§See e.g., 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
We got permission to enter the district and do the investigation from the Kayunga District health authorities. We obtained verbal informed consent and assent from the adult and minor respondents accordingly. We ensured confidentiality by conducting interviews in privacy ensuring that no one could follow proceedings of the interview. Unique identifiers were used and raw data were kept in a password protected computer and shared only among the investigation team.
Results
Descriptive epidemiology
There were 78 case-patients in Kayunga District (AR=20/100,000); 44 confirmed (V.cholerae 01 Ogawa) and 34 suspected. Ten case-patients died; case fatality rate (CFR)=13%. The median age was 24 years (IQR:15-37 years). Males were more affected (AR =24/100,000) compared to females (AR = 16/100,000). Persons aged ≥15 years were most affected (Table 1).
Table 1: Attack rates of case-patients by sex and age during a cholera outbreak in Kayunga District, Uganda, June–August, 2023.
| Characteristic | Frequency (n=78) | Population | AR /100,000 |
| Sex | |||
| Male | 46 | 194,407 | 24 |
| Female | 32 | 194,681 | 16 |
| Age (years) | |||
| 2-4 | 5 | 50,825 | 10 |
| 5-14 | 14 | 141,370 | 10 |
| 15-29 | 34 | 102,077 | 33 |
| 30-59 | 20 | 77,305 | 26 |
| ≥60 | 5 | 17,511 | 29 |
Of the nine sub-counties in Kayunga District, five were affected. Three of the affected sub-counties lie along the River Nile; Busaana Sub-county was the most affected (AR=109/100,000) (Figure 2).
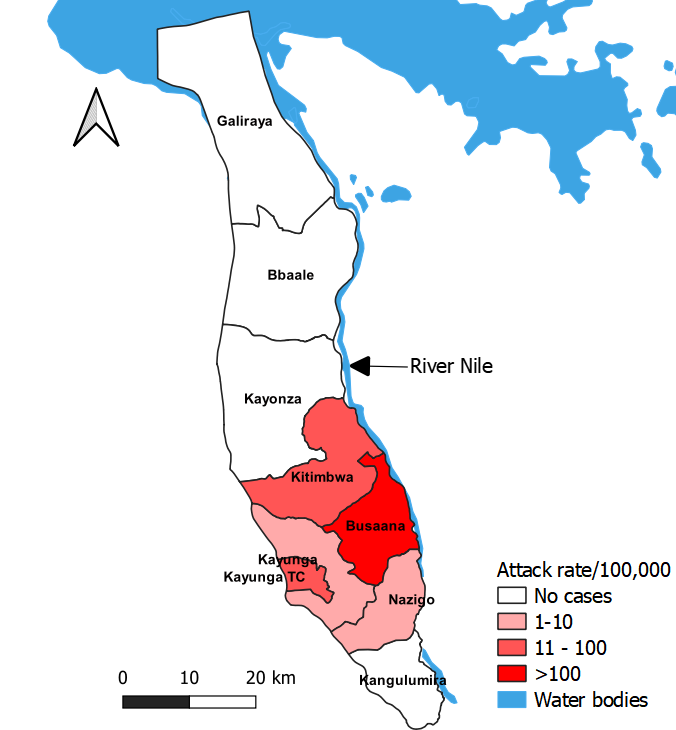
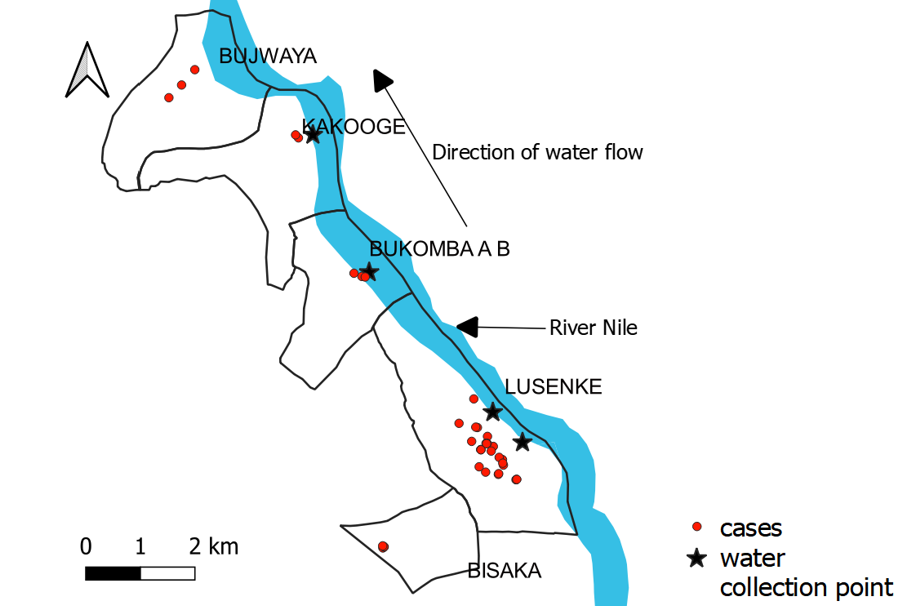
In Busaana Sub-county, Lusenke Village (lies upstream along River Nile) was the most affected (AR=4.0%). It registered cases before the downstream villages of Bukomba, Kakooge and Bujwaya. In these villages, cases were clustered around water collection points along the River Nile (Figure 3).
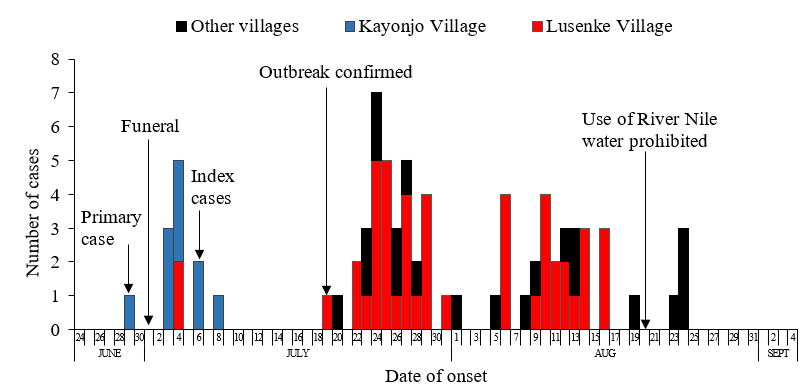
The “primary” case-patient presented with acute watery diarrhea on June 29, 2023 and the diarrhea was described as colorless (not rice-water) by caretakers. She was admitted in hospital six hours later and treated with intravenous rehydration. She died on June 30, 2023 about 10 hours following admission. The cause of death was described as respiratory failure in hospital. Her body was washed according to her culture and religious beliefs before being buried on July 1, 2023 in Kayonjo Village. Two days after the funeral, the deceased’s two brothers and a neighbor who had all attended the funeral developed acute watery diarrhea. They were admitted and treated in hospital and they both recovered. Three days after the funeral, another brother and a cousin to the “primary” case-patient who had also attended the funeral developed acute watery diarrhea. The brother died and the cousin recovered. Five days after the first funeral, the “primary” case’s father and another cousin who had also attended the funeral developed acute watery diarrhea and both died on July 7, 2023 at home. Following these two deaths, cholera was suspected; two rectal swabs were picked on July 7 from the deceased. Twelve days later, V. cholerae 01 Ogawa was confirmed by culture.
On July 19, cases started occurring in distant villages mainly Lusenke Village. During active case search, we found that two case-patients in Lusenke Village (a mother and her child) had their dates of onset on July 4, 2023, but we did not find them to have any link with Kayonjo Village (Figure 4). The mother and the child reported to have defecated along River Nile shore when they developed acute watery diarrhea. They also reported to have washed their clothes soiled with fecal matter along River shores before crossing to the neighboring district by boat to seek treatment. None of the case-patients in Lusenke Village admitted to have attended the funerals in Kayonjo Village, and neither of the cases in Kayonjo Village was reported/ reported to have travelled or come in contact with anyone in Lusenke Village.
Hypothesis generation findings
Sixty-eight percent of the case-patients had used water from River Nile and 23% had attended a funeral within 5 days prior to onset of symptoms. We hypothesized that, using contaminated water from River Nile while or attending a funeral was associated with cholera transmission.
Environmental findings
Lusenke Village is a low-lying village and had experienced episodes of flooding during the June–August 2023. According to VHT reports, latrine coverage in Lusenke Village was 38%. We found feces along the river banks in Lusenke Village; some case-patients and caretakers reported defecating in the river while fishing. We also found villagers washing clothes along the river banks where they also fetch water. Some of the case-patients and their care takers reported to have washed clothes soiled with fecal matter at the river banks.
Laboratory findings
No V. cholerae or coliforms were isolated from the water samples tested.
Case-control study findings
Eighty-eight percent (22/25) of case-patients compared to 53% (52/98) of controls used water from River Nile for domestic purposes (COR=6.5, CI 1.8-23). In addition, 36% (9/25) of case-patients compared to 9% (9/99) of controls drank water from River Nile (COR=5.6, 95%CI 1.9-16). All case-patients who drank River Nile water also used it for domestic purposes (Table 2). All persons who drunk or used water from River Nile did not boil or treat it.
Table 2: Risk factors associated with cholera transmission in Lusenke Village during the cholera outbreak in Kayunga District, Uganda, June–August, 2023
| Exposure | Cases (n) | (%) | Controls (n) | (%) | COR | 95%CI |
| Used River Nile water for domestic purpose | ||||||
| No | 3 | (12) | 46 | (47) | Ref | |
| Yes | 22 | (88) | 52 | (53) | 6.5 | 1.8-23 |
| Drank water from River Nile | ||||||
| No | 16 | (64) | 90 | (91) | Ref | |
| Yes | 9 | (36) | 9 | (9) | 5.6 | 1.9-16 |
| Used borehole water for domestic purposes | ||||||
| No | 17 | (68) | 48 | (48) | Ref | |
| Yes | 8 | (32) | 51 | (52) | 0.4 | 0.2-1.1 |
| Drank borehole water | ||||||
| No | 4 | (16) | 16 | (16) | Ref | |
| Yes | 21 | (84) | 83 | (84) | 1.0 | 0.3-3.3 |
| Attended a funeral | ||||||
| No | 12 | (48) | 53 | (46) | Ref | |
| Yes | 13 | (52) | 46 | (54) | 0.9 | 0.4-2.3 |
| Ate something at the funeral | ||||||
| No | 6 | (46) | 27 | (51) | Ref | |
| Yes | 7 | (54) | 26 | (49) | 1.2 | 0.4-4.1 |
| Drank anything at the funeral | ||||||
| No | 7 | (54) | 36 | (68) | Ref | |
| Yes | 6 | (46) | 17 | (32) | 1.8 | 0.5-6.2 |
| Touched the dead body | ||||||
| No | 9 | (69) | 44 | (85) | Ref | |
| Yes | 4 | (31) | 8 | (15) | 2.4 | 0.6-9.9 |
Upon using common reference group analysis, 36% (9/25) of case-persons and 8% (8/99) of controls drank and used River Nile water for domestic purposes (AOR=17, CI 3.8-77) compared to those who never drank or used River Nile water (Table 3).
Table 3: Adjusted odds ratios for domestic use or drinking of water from River Nile in Lusenke Village during the cholera outbreak in Kayunga District, Uganda, June–August, 2023
| Drank water from River Nile | Domestic use of water from River Nile | Cases (n) | (%) | Controls (n) | (%) | AOR | 95% CI |
| No | No | 3 | (12) | 46 | (46) | Ref | |
| Yes | No | 0 | (0) | 1 | (1) | NA | NA |
| No | Yes | 13 | (52) | 44 | (44) | 4.5 | 1.2-17 |
| Yes | Yes | 9 | (36) | 8 | (8) | 17 | 3.8-78 |
Discussion
The cholera outbreak in Kayunga District started in June and lasted two months. It was a propagated outbreak, caused by V. cholerae serotype 01 Ogawa, the major causative agent of previous cholera outbreaks in Uganda (22). The outbreak was initiated at a funeral of a suspected case whose source of infection was unknown, and amplified through contamination of river water used and drank by community members. Cases first occurred in the upstream villages before sequentially occurring in the downstream villages following the direction of flow of River Nile water. Lusenke Village which was most affected had low latrine coverage (38%) compared to the district average latrine coverage (about 70%) (17). In addition, there was defecation along River Nile banks.
The outbreak started in Kayonjo Village (an inland village) following a funeral of the “primary” case-patient. Relatives and neighbors developed symptoms of cholera days later. We were unable to ascertain how the primary case got cholera and how it spread among the relatives and neighbors. However, funerals have previously been found to be points of clusters of cholera transmission especially where individuals who wash the corpse also participate in food preparation without thoroughly washing hands (23–25). This might have been the source of infection among the funeral attendees.
From Kayonjo Village, the outbreak spread to other villages along the River Nile including: Lusenke, Bukomba, Kakooge and Bujwaya villages with some spillovers to other inland villages. The village being low-lying, makes it prone to flooding and river water contamination during heavy rains. Heavy rains, flooding and proximity to lakes and rivers have been identified by as the risk factors for cholera outbreaks in Uganda and Africa (13,14). These findings suggest that contaminated river water could have propagated the outbreak from Lusenke Village to downstream villages. Cases had 17 times odds of drinking and using unboiled/untreated river water for domestic purposes compared to controls. These findings further corroborate reports that V. cholerae is known to persist and thrive in river water for almost two years and can later enter the human body through consumption of contaminated water (2,26,27) (14). Prohibiting practices like washing and swimming in the river, enforcing latrine construction and discouraging people from drinking unboiled/ untreated river water could have largely contributed to the end of this outbreak.
The high CFR (13%) registered in this outbreak compared to the average of 2-4% reported from other outbreaks in Uganda (28) could be explained by poor health seeking behavior among case-patients as evidenced by the case-patients who died at home. With timely rehydration, the cholera CFR can be less than 1% (29). In addition, there was delay in suspicion and detection of cholera. Initial case-patients were reported to have presented with normal color diarrhea contrary to the usually expected whitish (rice-water) diarrhea. This could have led to the clinicians not suspecting cholera quickly. The outbreak was not suspected until four cases-patients had died. Further, it took 12 days to receive the stool culture results and confirm the outbreak. This delay in suspicion and confirmation could have led to delay in instituting timely and appropriate treatment and control measures.
Study limitations
We were not able to identify how the “primary” case acquired the infection to prevent similar future outbreaks and specifically how the infection reached Lusenke Village from Kayonjo Village which is far apart. However, it is likely that the outbreak might have been spread through population movement, open defecation, and flooding.
Conclusion
This outbreak started as a point source following a funeral in Kayonjo Village. It later spread to other villages where it was propagated and amplified by domestic use and drinking contaminated River Nile water. The water was likely contaminated by introduction of feces into the river by practices like open defecation and washing soiled clothes along the river. The outbreak lasted for two months and ended within one week following temporary prohibition of use of River Nile water and activities that contaminate river water. To prevent future similar outbreaks, community sensitization against drinking and domestically using untreated/ unboiled river water and enforcement of latrine construction should be sustained by the Kayunga District health department.
Public health actions
We instituted control measures for the outbreak, including: community and health worker sensitization, setting up a cholera treatment unit near the epicenter, distribution of hand washing facilities, water chlorinating tablets, and prophylactic antibiotics to affected communities.
Acknowledgements
We appreciate the support of the Kayunga District health team, Kayunga Regional Referral Hospital administration and personnel, and community members who participated in this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Authors’ contributions
AK, EN, YN, LNB, BK designed the study, contributed to data collection and analysis. AK led the writing of the bulletin. EN, YN, LNB, BK, IK, HTN, LB, and ARA participated in manuscript writing and review to ensure scientific integrity and intellectual content. All authors contributed to the final draft of the bulletin.
Copyright and licensing
All materials in Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form
References
- Cholera | Cholera Outbreak Response Field Manual [Internet]. [cited 2023 Nov 5]. Available from: https://choleraoutbreak.org/book-page/cholera
- Almagro-Moreno S, Taylor RK. Cholera: Environmental Reservoirs and Impact on Disease Transmission. Microbiol Spectr. 2013 Dec;1(2): OH-0003-2012.
- Azman AS, Rudolph KE, Cummings DAT, Lessler J. The incubation period of cholera: a systematic review. J Infect. 2013 May;66(5):432–8.
- Paye NG, Miller RHB, Zhou C, Weamie SJY, Davies TA. Systematic Study and Meta-Analysis of Risk Factors Associated with Cholera Outbreaks in Africa: A Review. Advances in Infectious Diseases. 2021 Apr 2;11(2):240–60.
- Cholera [Internet]. [cited 2023 Oct 4]. Available from: https://www.who.int/news-room/fact-sheets/detail/cholera
- Cholera – Global situation [Internet]. [cited 2023 Oct 4]. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON426
- WHO reports exponential rise in cholera cases in Africa | UN News [Internet]. 2023 [cited 2023 Oct 4]. Available from: https://news.un.org/en/story/2023/02/1133337
- Zheng Q, Luquero FJ, Ciglenecki I, Wamala JF, Abubakar A, Welo P, et al. Cholera outbreaks in sub-Saharan Africa during 2010-2019: a descriptive analysis. Int J Infect Dis. 2022 Sep; 122:215–21.
- WHO and Partners revamp war against cholera in Africa – World | ReliefWeb [Internet]. 2022 [cited 2024 Jan 24]. Available from: https://reliefweb.int/report/world/who-and-partners-revamp-war-against-cholera-africa
- Bwire G, Malimbo M, Makumbi I, Kagirita A, Wamala JF, Kalyebi P, et al. Cholera surveillance in Uganda: an analysis of notifications for the years 2007-2011. J Infect Dis. 2013 Nov 1;208 Suppl 1: S78-85.
- WHO_CDS_CSR_ISR_2000.1.pdf [Internet]. [cited 2024 Jan 24]. Available from: https://iris.who.int/bitstream/handle/10665/66485/WHO_CDS_CSR_ISR_2000.1.pdf?sequence=1
- Bwire G, Malimbo M, Maskery B, Kim YE, Mogasale V, Levin A. The Burden of Cholera in Uganda. PLOS Neglected Tropical Diseases. 2013 Dec 5;7(12): e2545.
- Bwire G, Ali M, Sack DA, Nakinsige A, Naigaga M, Debes AK, et al. Identifying cholera “hotspots” in Uganda: An analysis of cholera surveillance data from 2011 to 2016. PLOS Neglected Tropical Diseases. 2017 Dec 28;11(12): e0006118.
- WHO | Regional Office for Africa [Internet]. 2023 [cited 2024 Jan 19]. Floods raise cholera risk even as cases decline in Africa. Available from: https://www.afro.who.int/countries/madagascar/news/floods-raise-cholera-risk-even-cases-decline-africa
- Bwire G, Munier A, Ouedraogo I, Heyerdahl L, Komakech H, Kagirita A, et al. Epidemiology of cholera outbreaks and socio-economic characteristics of the communities in the fishing villages of Uganda: 2011-2015. PLOS Neglected Tropical Diseases. 2017 Mar 13;11(3): e0005407.
- Bwire G, Sack DA, Lunkuse SM, Ongole F, Ngwa MC, Namanya DB, et al. Development of a Scorecard to Monitor Progress towards National Cholera Elimination: Its Application in Uganda. Am J Trop Med Hyg. 2023 May 3;108(5):954–62.
- Kayunga District Profile | KAYUNGA DISTRICT [Internet]. [cited 2023 Oct 24]. Available from: https://kayunga.go.ug/about-us/district-profile
- Explore Statistics – Uganda Bureau of Statistics [Internet]. [cited 2024 Feb 6]. Available from: https://www.ubos.org/explore-statistics/20/
- Water | KAYUNGA DISTRICT [Internet]. [cited 2024 Jan 24]. Available from: https://kayunga.go.ug/services/water
- IDSR.pdf.
- Cholera Outbreak Toolbox [Internet]. [cited 2023 Oct 24]. Available from: https://www.who.int/emergencies/outbreak-toolkit/disease-outbreak-toolboxes/cholera-outbreak-toolbox
- Legros D, McCormick M, Mugero C, Skinnider M, Bek’Obita DD, Okware SI. Epidemiology of cholera outbreak in Kampala, Uganda. East Afr Med J. 2000 Jul;77(7):347–9.
- Ngwa MC, Young A, Liang S, Blackburn J, Mouhaman A, Morris JG. Cultural influences behind cholera transmission in the Far North Region, Republic of Cameroon: a field experience and implications for operational level planning of interventions. Pan Afr Med J. 2017; 28:311.
- McAteer JB, Danda S, Nhende T, Manamike P, Parayiwa T, Tarupihwa A, et al. Notes from the Field: Outbreak of Vibrio cholerae Associated with Attending a Funeral — Chegutu District, Zimbabwe, 2018. MMWR Morb Mortal Wkly Rep. 2018 May 18;67(19):560–1.
- Sack RB, Siddique AK. Corpses and the spread of cholera. The Lancet. 1998 Nov 14;352(9140):1570.
- Opare J, Ohuabunwo C, Afari E, Wurapa F, Sackey S, Der J, et al. Outbreak of Cholera in the East Akim Municipality of Ghana Following Unhygienic Practices by Small-Scale Gold Miners, November 2010. Ghana Med J. 2012 Sep;46(3):116–23.
- Jubair M, Atanasova KR, Rahman M, Klose KE, Yasmin M, Yilmaz Ö, et al. Vibrio cholerae Persisted in Microcosm for 700 Days Inhibits Motility but Promotes Biofilm Formation in Nutrient-Poor Lake Water Microcosms. PLOS ONE. 2014 Mar 25;9(3): e92883.
- Uganda Cholera case fatality ratio, 1923-2023 [Internet]. [cited 2024 Jan 29]. Available from: https://knoema.com/atlas/Uganda/topics/Health/Communicable-Diseases/Cholera-case-fatality-ratio?mode=amp
- Cholera Outbreak Response field manual | Cholera Outbreak Response Field Manual [Internet]. [cited 2024 Jan 29]. Available from: https://choleraoutbreak.org/

