Cholera outbreak associated with drinking contaminated lake shore water, Namayingo District, Uganda, July–August 2023
Authors: John Rek1*, Daniel Orit1, Susan Waako1, Benon Kwesiga1, Richard Migisha1, Lillian Bulage1, Alex Riolexus Ario1; Institutional affiliation: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda; Correspondence*: Tel: +256782387857, Email: jrek@uniph.go.ug
Summary
Background: On July 24, 2023 Uganda’s Ministry of Health confirmed a cholera outbreak on Sigulu Island, Namayingo District. We investigated to determine its magnitude, identify possible exposures and recommend evidence-based control interventions.
Methods: We defined a suspected case as acute onset of watery diarrhea in a resident of Sigulu and Bukana Sub-counties in Namayingo District from July 1–August 15, 2023, and a confirmed case as a suspected case with positive Vibrio cholerae serotype 01 and 0139 stool culture. Cases were identified by active case search and records review at the health centers. We conducted descriptive epidemiology, environmental assessment at the lakeshore water collection points, and generated hypotheses. We additionally collected water samples from lakeshore water collection points and Jericans used for household water storage for cholera testing. We conducted an unmatched individual case-control study to compare exposures among case-patients and asymptomatic controls residing in Sigulu and Bukana sub-counties.
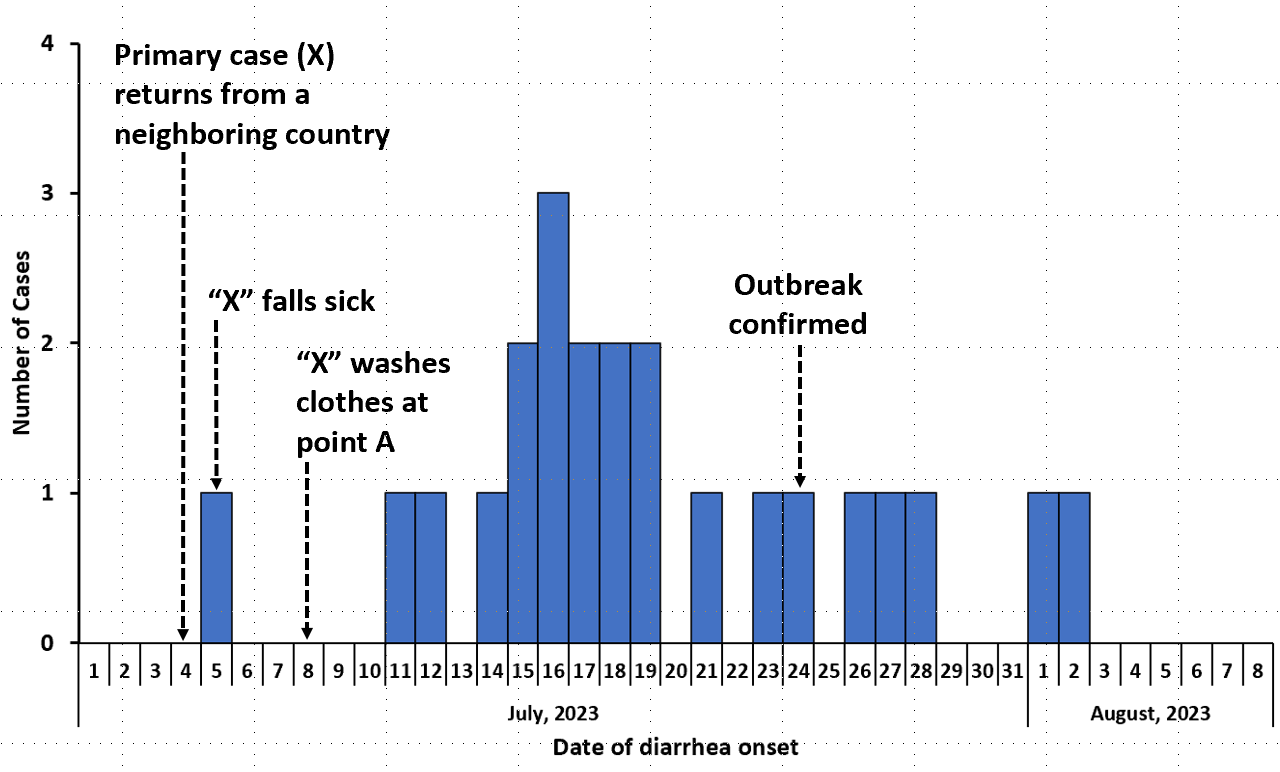
Results: We identified 24 cases of which 4 were confirmed to have V.cholerae serotype 01 and 0139 ogawa. Fifteen (62%) cases were female and the median age of cases was 27 years (range:2-68 years). Nine (37%) received the oral cholera vaccine (OCV) in 2020/2021. The epi curve showed a propagated outbreak after the contamination of a communal water collection point on July 8, 2023 by the primary case who had recently traveled back from a neighboring country with a cholera outbreak. Eighteen (75%) were resident of Secho village in Sigulu sub county. All case-patients drunk lakewater but no water samples tested positive for Vibrio cholerae. Compared to other water collection points, drinking water from water point A in Secho, Sigulu sub-county increased odds of getting cholera (aOR=4.3, 95% CI: 1.3–15). Treatment of drinking water by any means (aOR=0.085, 95% CI: 0.097–0.74) and receiving OCV (aOR=0.16, 95% CI: 0.051–0.56) were both protective. We observed residents directly drawing lakeshore water for laundry, bathing, and drinking.
Conclusion: This cholera outbreak in an island community was associated with the introduction of Vibrio cholerae by a traveller, followed by community consumption of untreated lakeshore water. We recommended mass distribution of water treatment tablets, repeated OCV, and community mass sensitization about risks associated with drinking untreated lake water.
Introduction
Cholera is characterized by profuse rice water diarrhea and is caused by the bacterium Vibro cholerae. It is transmitted through the consumption of Vibrio cholerae fecally contaminated food and water (1). It has an incubation period of hours to 5 days, with most infected persons being asymptomatic carriers capable of transmitting infection (2). Most of the global burden of cholera is seen in developing countries and areas with poor sanitation (ref). Globally, there are about 1.3 to 4 million cases and 22,000 to 143,000 deaths annually (3). Clusters of cholera are common due to either person to person spread or through spread from contamination of the environment by a case (4). Strategies for prevention of cholera include; vaccination in hotspots, and improving water, sanitation and hygiene. The global targets are a reduction of deaths by 90% and elimination of transmission in 20 countries by 2030 (5).
Uganda is one of the cholera endemic countries targeted for cholera elimination by the global task force for cholera. Between 2015 and 2021, Uganda had reported 63 outbreaks from 61 districts with a total of 8,498 cases(6). There are several hotspots in the country including border and refugee hosting districts and, lakeshore communities. Urban slums are also at high risk of cholera(7,8). While progress has been made in the fight against Cholera, over 15 districts remain endemic for Cholera in Uganda including Namayingo (6,9). Between 2018 and 2021, the country rolled out the Oral Cholera Vaccination (OCV) campaign in several districts, including Namayingo in a bid to eliminate Cholera from these districts. The vaccine is given in 2 doses, 14 days apart to people aged ≥2 years and provides protection upto 80% for 3 years (10). Despite this, the country still grapples with cholera outbreaks from time to time (6).
On July 24, 2023, the Ministry of Health was notified of a confirmed outbreak of Cholera in Sigulu Island. This followed an alert on July 15, 2023 of four residents from Secho village, Sigulu Island in Namayingo District presenting with acute profuse watery diarrhea and vomiting. Stool samples from 4 of the suspected cases were sent to the Central Public Health Laboratory (CPHL) for testing and three of the four were confirmed culture positive for Vibro cholerae 01 ogawa. We investigated the outbreak to determine its magnitude, identify possible associated exposures and recommend evidence-based control and prevention interventions.
Methods
Outbreak area
The outbreak occurred in Namayingo District, Busoga Region, in South Eastern Uganda. The district has nine subcounties and 193 villages with an estimated population of 247,400 people (11). Three of the district sub counties (Bukana, Sigulu and Lolwe) are Island sub counties, with an estimated population of 42,900 people. Safe water coverage in the district is 62% (12), and latrine coverage is 20% (13).
Case definition and finding
We defined a suspected case as any resident of Sigulu and Bukana Subcounties in Namayingo District aged ≥2 years with acute onset of watery diarrhea between July 1 – August 15 2023. A confirmed case was a suspected case with Vibrio cholerae O1 or O139 confirmed by stool culture. Cases were identified through records review at the health centres and active case search in the community.
Descriptive epidemiology
We conducted descriptive analysis of the cases identified during July 1 to August 15, 2023 by age, sex, clinical presentation, place of residence, possible exposures, and vaccination status. We calculated attack rates by age, sex, and place of residence using population estimates from Namayingo district biostatistician and Uganda Bureau of statistics, of persons aged ≥2 years. An epicurve was used to describe the distribution of cases by dates of symptom (diarrheal) onset.
Laboratory investigations
We collected both stool (ten samples) and water (six samples) and shipped to the Central Public Health Laboratories in triple packaging bags for testing.
Environmental assessment
We inspected six water collection sources identified by the case-patients in the villages of Secho, Bukana, Buhere, Buhone, and Bulagaye to observe for open defecation, water collection practices, and activities at the water collection sites like washing clothes and bathing.
Hypothesis generation
We used a case investigation form to collect information on potential exposures including sources of household water, water treatment practices, consumption of commercial foods and drinks, food preparation, contact with an individual with profuse watery diarrhea, and travel form an area with known cholera. We also assessed vaccination status of case-patients by looking at vaccination cards and for those with no cards, a vivid recall of the vaccination exercise, dose schedule, and vaccine administration. One was considered fully vaccinated if they had received 2 doses of the OCV.
Case control study
We conducted a 1:4 individual unmatched case control study in Sigulu and Bukana sub counties where the case-patients resided. Control persons were residents of the same village as the case patients but never had an episode of acute watery diarrhea from July 1, 2023 to the time of the investigation. They were selected randomly using the case patient household as the starting point and spinning a bottle to obtain direction of the next household. This was continued until all the 4 controls were selected.
Ethical considerations
The Ministry of Health (MoH) gave permission to investigate this outbreak. We additionally sought permission and support to conduct the investigation from district health authorities of Namayingo District. In addition, the office of the Center for Global Health, US Center for Disease Control and Prevention determined that this activity was not human subject research and with its primary intent being for public health practice or disease control. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy. § § See e.g., 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
We sought verbal informed consent from the respondents who were either sick at the time or survivors of cholera. All respondents were informed that their participation was voluntary and their refusal would not attract any negative consequences. To ensure confidentiality, personal identifying information collected was only accessed by the investigators.
Results
Descriptive epidemiology
We identified 24 cases of which four were confirmed cases of Vibro cholerae, serotype 01 and 0139 ogawa. There was no death reported. The median age of the case-patients was 27 years (range: 1-68) and those above 15 years (79% (19) Attack rate (AR) 7/1000) were most affected. Both sexes were affected. However,females (63% (15), AR: 12/100,000) were more affected than males. Cases were clustered around water collection points, and the most affected were residents of Secho village in Sigulu sub county (79% (19), attack rate: 13/1000 (Figure). The epi curve showed a propagated outbreak following the washing of fecally soiled clothes by the primary case on July 8, 2023 (Figure 2). The majority of case patients 92% (22) drank untreated lake water and 38% (9) received the OCV
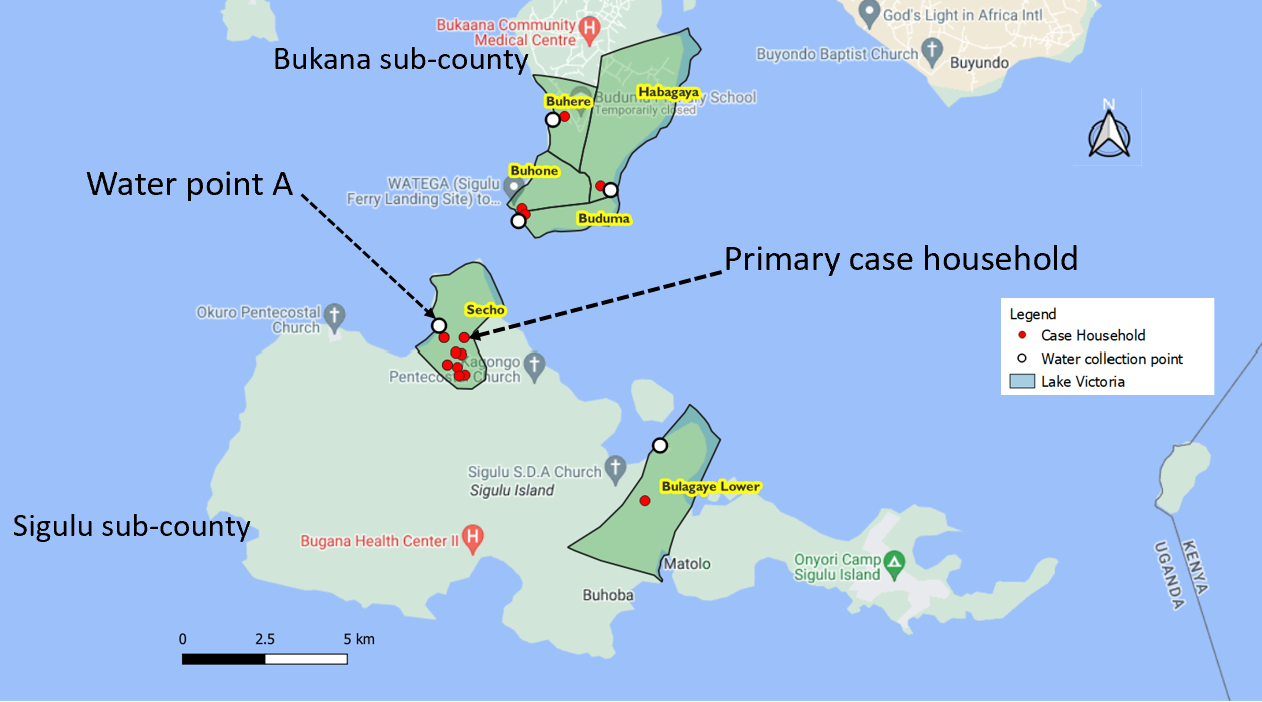
Cases started to rise after the primary case washed her fecally soiled clothes at the water collection point A, on July 8. After confirmation and institution of control measures from July 25, cases declined and eventually stopped.
Environmental assessment findings
We found that residents drew lake water for all domestic use, but also bath and washed clothes at the lake shore water collection points. Residents were also seen drinking water directly drawn from the lake. The available boreholes had salty unpalatable hard water.
Exposures associated with cholera in Sigulu and Bukana subcounties, Namayingo District, Uganda, July 1 – August 15, 2023
From the case-control study, compared to other water collection points, drinking water from water point A in Secho, Sigulu sub-county increased odds of getting cholera (aOR=4.3, 95% CI: 1.3–15). The odds of getting cholera were reduced by treatment of drinking water by any means (aOR=0.085, 95% CI: 0.097–0.74) and receiving OCV (aOR=0.16, 95% CI: 0.051–0.56).
Discussion
This was a cholera outbreak following possible importation of Vibrio cholerae into Secho Village, Sigulu Island in Namayingo District. Six villages in 2 sub-counties were affected. We also show evidence that drinking untreated lake water was a risk factor, while the cholera vaccine remained protective after 2 years of administration.
Namayingo District borders Kenya to the east and is a cholera epidemic prone district. In the past, the district has had several cholera outbreaks, mainly affecting the island subcounties. There have also been cases of the outbreak spreading to the mainland for example in 2018, where 90% of mainland cases were reported to have originated from the Islands(14). Being a border district, cross border movements between Uganda and Kenya provide an efficient channel for spread of epidemic diseases like cholera(15) . During this outbreak, it is reported that Busia Kenya had a protracted cholera outbreak. The primary case travelled back to Sigulu after possible exposure at a hospital in Busia Kenya where she shared a ward with suspected cholera patients between June 27 and July 4 2023.
All age groups were affected. However, adults ≥15 years and females were more affected in this outbreak. Cholera is a water borne disease, and all age groups and gender can be affected by the infection, though some age groups and genders may be more affected than the others. Outbreaks in other settings have indeed shown different age groups being affected by cholera, for example in the cholera outbreak in the democratic republic of Congo, December 2022(16), Bagdad, Iraq in 2015(17) and Kampala, Uganda in 2018(18). Females especially those above 15 years play a more central role in water collection, food preparation and washing of clothes, either as wives or older siblings in the household (19,20). They therefore have more exposure to the water sources than male counterparts. In this investigation, we found that indeed females above 15 years were more affected.
The index case was suspected on July 16, ten days after the primary case developed symptoms of cholera. The 7-1-7 protocol requires that an infectious disease outbreak is detected within 7 days, notified within a day and response measures mounted within 7 days after notification. This outbreak was detected10 days after the primary case developed symptoms. An outbreak of cholera is detected when two or more suspected cholera cases are reported from the same unit within a week of each other or if there is a death in a person 2 years and older due to acute watery diarrhea with no other known cause(21). This presented a missed opportunity to curb the outbreak. If the primary case had been detected, she would not have washed clothes at the lakeshore water collection point as usual, thus stopping spread of the outbreak.
Drinking of untreated water from unsafe water collection points is a major risk for cholera. The lakeshore communities affected by this outbreak drink untreated water from the lakeshores. Like in many other outbreaks in lake shore communities, this has been found to be a risk factor for outbreaks (22–25). Fresh water access at Sigulu and Bukana Sub counties are 59% and 30% respectively (12). However, the borehole water was heavily salty and unpalatable, and the piped lake water was only available in Bukana subcounty at a fee of 0.08 USD per 20 liter Jerican. This cost is prohibitive to the community members who find it expensive. Provision of safe drinking water is a major preventive strategy for the control of cholera, in addition to improved hygiene and sanitation(26,27).
The oral cholera vaccine was deployed in Namayingo in October 2020 as a strategy to control outbreaks especially in the outbreak prone lakeshore communities of the district (6). This investigation confirms that several residents received the vaccine and either had a vaccination card or could recall the vaccination process. The vaccine is given in 2 doses, 14 days apart and targeting individuals over 2 years and It provides protection upto 80% for 3 years (10) . We found that the vaccine given in the 2020/2021 campaign was 84% protective of cholera in the individuals who received it 2 years post vaccination. This is consistent with other studies in Zambia and Malawi that report vaccine protection upto 80% when 2 doses are administered(28,29).
Study limitations
This investigation had some limitations including. First, some patients with cholera experience mild or nonspecific symptoms or asymptomatic and may not have been picked up during case-finding. This likely led to an under estimation of the magnitude of the outbreak. Secondly, although drinking untreated and contaminated lake water was found to be significantly associated with cholera, Vibro cholerae was not isolated from any of the water samples tested. This is likely because of late collection of samples, which was over three weeks since contamination with soiled clothes by the primary case. Additionally, being an open lake shore collection point, any residual reservoirs could have been washed away by lake shore waves or the concentration of biofilms harboring vibro cholerae was low(30).
Conclusion
This outbreak was associated with drinking contaminated and untreated lake shore water. However, receiving the OCV was protective against cholera. We recommended emergency distribution of water treatment tablets, sensitisation of the community about cholera and treatment of all drinking water and deployment of periodic OCV to the high-risk island residents. The public health actions implemented included, distribution of water treatment tablets, mass sensitisation of the communities in the affected sub counties about cholera and refresher training of health workers about cholera and its management.
Conflict of Interest
The authors declare that they had no conflict of interest.
Authors contribution
JR, SW, DO, BK, and LB designed the study and contributed to data collection and analysis. JR led the writing of the bulletin. SW, DO, RM, BK, LB, and ARA participated in bulletin writing and review to ensure scientific integrity and intellectual content. All authors contributed to the final draft of the bulletin.
Acknowledgments
The authors would like to thank the Namayingo District Health Office, Bugana and Bumalenge Health Center staff, VHTs, and community members for their support during this investigation.
Copyrights and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- WHO 2022. Cholera Fact sheet [Internet]. Available from: https://www.who.int/news-room/fact-sheets/detail/cholera
- Azman AS, Rudolph KE, Cummings DAT, Lessler J. The incubation period of cholera: A systematic review. J Infect. 2013 May;66(5):432–8.
- World Health Organization. Global Task Force on Cholera Control: Ending Cholera. A global road map to 2030 [Internet]. Available from: https://www.gtfcc.org/wp-content/uploads/2019/10/gtfcc-ending-cholera-a-global-roadmap-to-2030.pdf
- Deen J, Mengel MA, Clemens JD. Epidemiology of cholera. Vaccine. 2020 Feb 29;38:A31–40.
- Kanungo S, Azman AS, Ramamurthy T, Deen J, Dutta S. Cholera. The Lancet. 2022 Apr;399(10333):1429–40.
- Bwire G, Sack DA, Lunkuse SM, Ongole F, Ngwa MC, Namanya DB, et al. Development of a Scorecard to Monitor Progress toward National Cholera Elimination: Its Application in Uganda. The American Journal of Tropical Medicine and Hygiene. 2023 May 3;108(5):954–62.
- Bwire G, Ali M, Sack DA, Nakinsige A, Naigaga M, Debes AK, et al. Identifying cholera “hotspots” in Uganda: An analysis of cholera surveillance data from 2011 to 2016. PLoS Negl Trop Dis. 2017 Dec;11(12):e0006118.
- Bwire G, Orach CG, Aceng FL, Arianitwe SE, Matseketse D, Tumusherure E, et al. Refugee Settlements and Cholera Risks in Uganda, 2016–2019. Am J Trop Med Hyg. 2021 Apr;104(4):1225–31.
- Atuhairwe J. Spreading like a wild fire: a tale of three cholera outbreaks, Namayingo District, Uganda, March 2016. Pan Afr Med J. 2018 Jan;
- Bi Q, Ferreras E, Pezzoli L, Legros D, Ivers LC, Date K, et al. Protection against cholera from killed whole-cell oral cholera vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2017 Oct;17(10):1080–8.
- Uganda Bureau of Statistics. Statistical Abstract, 2022 [Internet]. 2022. Available from: https://www.ubos.org
- Uganda Water Supply Atlas [Internet]. [cited 2024 Jan 17]. Available from: http://wsdb.mwe.go.ug/index.php/reports/district/104
- Bwire G, Kisakye A, Amulen E, Bwanika JB, Badebye J, Aanyu C, et al. Cholera and COVID-19 pandemic prevention in multiple hotspot districts of Uganda: vaccine coverage, adverse events following immunization and WASH conditions survey. BMC Infectious Diseases. 2023 Jul 21;23(1):487.
- The Independent. Few people turn up for cholera vaccination in Namayingo [Internet]. The Independent Uganda: 2020. Available from: https://www.independent.co.ug/fewer-people-turn-up-for-cholera-vaccination-in-namayingo/
- Bwire G, Mwesawina M, Baluku Y, Kanyanda SSE, Orach CG. Cross-Border Cholera Outbreaks in Sub-Saharan Africa, the Mystery behind the Silent Illness: What Needs to Be Done? PLoS One. 2016 Jun 3;11(6):e0156674.
- World Health Organization. Disease Outbreak News; Cholera – Democratic Republic of Congo [Internet]. 2023. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON441
- Jameel SK, Shafek MA, Abdulmohsen AM, Mohamed NS, Naji SR, Mohammed TT. The Isolation of Vibrio cholera and Other Enteric Bacteria with Molecular Characterization of Vibrio cholera during the Outbreak of Baghdad/Iraq in 2015. Advances in Microbiology. 2016 Aug 2;6(9):699–715.
- Eurien D, Mirembe BB, Musewa A, Kisaakye E, Kwesiga B, Ogole F, et al. Cholera outbreak caused by drinking unprotected well water contaminated with faeces from an open storm water drainage: Kampala City, Uganda, January 2019. BMC Infect Dis. 2021 Dec;21(1):1–9.
- UNICEF. Brief notes on gender and cholera [Internet]. 2010 [cited 2024 Jan 16]. Available from: https://gbvguidelines.org/wp/wp-content/uploads/2020/03/29_Haiti_UNICEF_Briefing_Note_Gender_Cholera.pdf
- Rancourt N. Oxfam Policy & Practice. 2013. Gender and Vulnerability to Cholera in Sierra Leone: Gender analysis of the 2012 cholera outbreak and an assessment of Oxfam’s response. Available from: https://policy-practice.oxfam.org/resources/gender-and-vulnerability-to-cholera-in-sierra-leone-gender-analysis-of-the-2012-293965/
- Cholera Outbreak Toolbox [Internet]. . Available from: https://www.who.int/emergencies/outbreak-toolkit/disease-outbreak-toolboxes/cholera-outbreak-toolbox
- Challa JM, Getachew T, Debella A, Merid M, Atnafe G, Eyeberu A, et al. Inadequate Hand Washing, Lack of Clean Drinking Water and Latrines as Major Determinants of Cholera Outbreak in Somali Region, Ethiopia in 2019. Frontiers in Public Health [Internet]. 2022 [cited 2024 Jan 16];10. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2022.845057
- Oguttu DW, Okullo A, Bwire G, Nsubuga P, Ario AR. Cholera outbreak caused by drinking lake water contaminated with human faeces in Kaiso Village, Hoima District, Western Uganda, October 2015. Infectious Diseases of Poverty. 2017 Oct 10;6(1):146.
- Pande G, Kwesiga B, Bwire G, Kalyebi P, Riolexus A, Matovu JKB, et al. Cholera outbreak caused by drinking contaminated water from a lakeshore water-collection site, Kasese District, south-western Uganda, June-July 2015. PLoS One. 2018;13(6):e0198431.
- Birmingham ME, Lee LA, Ndayimirije N, Nkurikiye S, Hersh BS, Wells JG, et al. Epidemic cholera in Burundi: patterns of transmission in the Great Rift Valley Lake region. The Lancet. 1997 Apr 5;349(9057):981–5.
- Buliva E, Elnossery S, Okwarah P, Tayyab M, Brennan R, Abubakar A. Cholera prevention, control strategies, challenges and World Health Organization initiatives in the Eastern Mediterranean Region: A narrative review. Heliyon. 2023 May 1;9(5):e15598.
- Wolfe M, Kaur M, Yates T, Woodin M, Lantagne D. A Systematic Review and Meta-Analysis of the Association between Water, Sanitation, and Hygiene Exposures and Cholera in Case–Control Studies. The American Journal of Tropical Medicine and Hygiene. 2018 Jul 2;99(2):534–45.
- Grandesso F, Kasambara W, Page AL, Debes AK, M’bang’ombe M, Palomares A, et al. Effectiveness of oral cholera vaccine in preventing cholera among fishermen in Lake Chilwa, Malawi: A case-control study. Vaccine. 2019 Jun 19;37(28):3668–76.
- Sialubanje C, Kapina M, Chewe O, Matapo BB, Ngomah AM, Gianetti B, et al. Effectiveness of two doses of Euvichol-plus oral cholera vaccine in response to the 2017/2018 outbreak: a matched case–control study in Lusaka, Zambia. BMJ Open. 2022 Nov;12(11):e066945.
- Conner JG, Teschler JK, Jones CJ, Yildiz FH. Staying alive: Vibrio cholerae’s cycle of environmental survival, transmission, and dissemination. Microbiol Spectr. 2016 Apr;4(2):10.1128/microbiolspec.VMBF-0015–2015.

