Measles Outbreak in Bundibugyo District, Western Uganda, February–June 2023
Authors: Dominic Kizza1*, Yasiini Nuwamanya1, Susan Waako1, Benon Kwesiga1,2, Richard Migisha1,2, Daniel Kadobera1,2, Alex Ario Riolexus1,2; Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda; 2Uganda National Institute of Public Health, Kampala, Uganda; Correspondence*: Tel: +256782264576, Email: dkizza@uniph.go.ug
Summary
Background: Measles is the most common cause of vaccine preventable disease outbreaks in Uganda. On April 28, 2023, the Ministry of Health was notified of a measles outbreak in Bundibugyo District, Western Uganda. We investigated to determine the scope of the outbreak, assess risk factors for transmission, evaluate vaccine effectiveness (VE), and recommend control measures.
Methods: A suspected measles case was onset of fever and maculopapular rash, plus ≥1 of: cough, runny nose, or conjunctivitis in a Bundibugyo District resident from February 1 to June 8, 2023. A confirmed case was a suspected case with positive measles-specific IgM. We reviewed medical records and conducted active case-finding in communities to identify case-patients. We conducted a matched case-control study (by age and village of residence) to identify risk factors for transmission. We estimated vaccine coverage using the percentage of vaccinated persons among eligible controls. We identified risk factors using conditional logistic regression, and calculated VE as VE= 1-ORMH, where ORMH is the Mantel-Haenszel odds ratios associated with having received ≥1 dose of measles vaccine.
Results: We identified 234 case-patients; 14 (6%) were confirmed and 4 (2%) died. Children aged 7-11 months were the most affected (attack rate [AR]=134/10,000), followed by 0-6 months (AR=44/10,000). Tokwe (AR=18/10,000) and Bundibugyo (AR=19/10,000) were the most affected sub-counties. Being unvaccinated for measles (aOR=6.1, 95%CI: 2.5–15) and visiting a health facility with symptomatic case-patients 7-21 days before rash onset (aOR=3.7, 95%CI: 1.0–13) increased odds of infection. Overall, measles vaccination coverage was 86% (95%CI 79-92); VE was 87% (95%CI: 69–94%).
Conclusion: The measles outbreak was facilitated by suboptimal vaccine coverage. A mass measles vaccination campaign targeting children <5 years in affected sub-counties, and proper triaging and isolation of patients with signs and symptoms of measles could help prevent future outbreaks in this area.
Background
Measles virus causes systemic illness (1, 2). Transmission of measles is dependent on person to person spread through respiration droplets or direct contact (2).Measles is highly contagious disease which was responsible for high infant mortality before the advent of an effective vaccine in 1963 (3). Furthermore measles virus infection diminishes preexisting antibodies that offer protection from other pathogens (4).
Despite the availability of an effective and safe vaccine for almost half a century, measles is re-emerging in several developed countries because of the insufficient vaccination coverage among specific sub-populations, the emerging anti-vaccination movement, and the increasing movement of humans across borders. (5). The same applies to developing countries. Most strategies for reducing global measles morbidity and mortality and eliminating measles are based on the ability to enhance immune response to the measles virus(6).
In 2023, Uganda launched a nationwide measles-rubella vaccination campaign, targeting 18.1 million children aged 9 months to 15 years, with the aim of achieving at least 95% coverage in each district. The campaign was conducted in two phases, from 12–16 September and from 19–23 September, using a fixed-post and outreach strategy (7). The campaign also included vitamin A supplementation and deworming for children under five years of age. Despite the measures, Uganda has been experiencing measles outbreaks.
On April 28, 2023, Ministry of Health (MoH) received a notification of a measles outbreak in Bundibugyo District, Uganda. This was after four out of five samples tested positive for measles specific IgM antibodies at the Uganda Virus Research Institute (UVRI). A total of 78 case-patients had been line listed at that time. We determined the scope of the outbreak, assessed risk factors for transmission, assessed vaccine effectiveness and vaccine coverage, and recommended evidence-based control measures.
Methods
Outbreak area
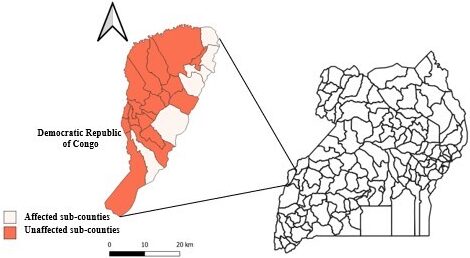
This outbreak occurred in Bundibugyo District, Western Uganda between March and June 2023. The district is bordered by Ntoroko District to the north, Kabarole District to the east and southeast and the Democratic Republic of Congo to the west.
The outbreak affected 18 sub counties and town councils of Bundibugyo District namely: Tokwe, Bundibugyo town council, Nyahuka town council, Buganikire town council, Busaru, Bubandi, Kisubba, Mirambi, Bubukwanga, Butama-Mitunda town council, Kirumya, Ntotoro, Bundingoma, Busunga town council, Bukonzo, Nduguto, Ntandi town council and Sindila. The district has a population of approximately 277,900 people.
The district has 27 sub-counties and town councils and covers an area of 848.2 km2 with an average population density of approximately 328/km2.
Case definition and finding
We defined a suspected case as onset of fever and maculopapular rash, with at least one of the following: cough, runny nose (Coryza) or conjunctivitis (red eyes) in a resident of Bundibugyo District from 1st February, 2023 to 08th June 2023. A confirmed case was defined as a suspected case that has been confirmed positive for IgM measles-specific antibody test(2).
We reviewed patient records to identify measles case-patients that visited health facilities in Bundibugyo District since February, 2023. We updated the line-list by reviewing patients’ clinical records and registers.
Additional case-patients were identified through active case search at both health facilities and communities, with the help of the Health Assistants (HAs) and Village Health Teams (VHTs). We trained 15 HAs from the 18 affected sub-counties on the case definition, and these subsequently cascaded the training to their respective VHTs. The VHTs then conducted house to house community active case-search, and notified the HA who then verified whether the person met the case definition. For those that met the case definition, a standard Case Investigation Form (CIF) would then be administered by the HA.
Descriptive epidemiology
We described the case-patients by calculating attack rates by person and place, using the Uganda Bureau of Statistics 2021 population projection of children in Bundibugyo District sub counties as the denominator (8). We further described the case-patients by time of rash onset using an epidemic curve.
Hypothesis generation interviews
We conducted fifty-six (56) hypothesis-generating interviews using a standardized measles case investigation form. We interviewed parents/guardians of case-patients about potential risk factors for measles transmission occurring within 3 weeks before onset of signs and symptoms. These included visiting a health facility, attending social gatherings, school or places of worship, receiving a visitor and travelling outside Bundibugyo district. We asked parents/guardians about the case-patients’ immunization status before symptom onset. Vaccination status was verified through review of health cards and where the card was missing, a recall approach was employed. Additional risk factors we assessed included playing away from home and visiting water collection points.
Laboratory Investigations
We collected whole blood, oral and pharyngeal swabs from suspected case-patients for measles IgM antibody testing and molecular testing to ascertain the strain.
Environmental investigations
We conducted an environmental assessment at the different border crossings between DRC and Bundibugyo district, as well the isolation facilities at the two major measles treatment units i.e. Bundibugyo Hospital and Nyahuka HCIV. This was with the aim of evaluating any potential factors that may have led to the outbreak
Case control study
We conducted a matched case control study in the 18 affected sub-counties and town councils to evaluate exposures that emerged during hypothesis generation. We defined a control as any person residing in Bundibugyo District with no history of fever or rash from 1st Feb 2023 to 8th June 2023.
We matched cases to controls by age, the following groups: 0<9 months, 9-24 months, 25-59 months, 5-14 years and >14 years to align with the national routine and mass immunization schedules for measles and by village of residence to ensure both case and control had comparable exposures. The controls were randomly selected from the neighborhood and from only households that didn’t report any measles case from February 2023 to 8th June 2023. We defined effective exposure period to be the time window during 7-21 days prior to case patient’s onset of rash. Vaccination history was assessed by vaccination card availability and recall of the parent with demonstration of knowledge on site of vaccination. We collected data using Epi Data and exported it to MS Excel for cleaning. We conducted data analysis using Epi Info 7.1.5. We conducted a conditional logistic regression to analyze matched case control data.
We estimated vaccine effectiveness for measles vaccine using the formula VE= (1-ORProtective) where ORProtective were the protective odds from the case control study. We excluded subjects with ages between 1 to 9 months based on Uganda’s measles immunization schedule.
Measles vaccine effectiveness
We identified risk factors using conditional logistic regression, and calculated VE as VE= 1-ORMH, where ORMH is the Mantel-Haenszel odds ratios associated with having received ≥1 dose of measles vaccine.
Measles vaccine coverage
We estimated vaccine coverage using the percentage of vaccinated persons among eligible controls.
Ethical considerations
This outbreak investigation was in response to a public health emergency and was therefore determined to be non-research. The Ministry of Health (MoH) gave permission to investigate this outbreak. The investigation was also approved by US CDC and conducted in accordance to the applicable US federal laws.
We sought permission to conduct the investigation from District health authorities of Bundibugyo District. We also sought verbal informed consent from the respondents who were survivors, and next of kin of the deceased. We ensured privacy during all interviews and case-patients information was kept confidential throughout the investigation period and beyond.
Results
Descriptive epidemiology
Overall, 234 measles cases were identified (220 suspected and 14 confirmed cases), with a case-fatality rate of 2%. The age range of the identified cases was 2 months–60 years with age group 7–11 months being the most affected (AR 134/10,000 persons), followed by 0–6 months (AR 44/10,000 persons). Males and females were similarly affected (Attack rate [AR]: 9/10,000) vs. 8/10,000) (Table 1). Tokwe (AR 19/10,000 persons) and Bundibugyo TC (AR 18/10,000 persons) were the most affected sub counties (Table 1).
Table 1: Measles attack rate by sex and age group of case-patients and sub counties, Bundibugyo District, Western Uganda, March-June, 2023
| Variable | Frequency | Population | AR/10,000 |
| Age | |||
| 0-6 Months | 29 | 6,586 | 44 |
| 7-11 Months | 72 | 5,363 | 134 |
| 12-59 Months | 105 | 45,020 | 23 |
| 5-14 Years | 21 | 91,985 | 2 |
| 15 Years and above | 7 | 128,946 | 1 |
| Sex | |||
| Male | 116 | 136,300 | 9 |
| Female | 118 | 141,600 | 8 |
| Sub-county | |||
| Tokwe | 23 | 11,886 | 19 |
| Bundibugyo TC | 43 | 23,711 | 18 |
| Nyahuka | 34 | 20,883 | 16 |
| Buganikere TC | 9 | 6,344 | 14 |
| Busaru | 24 | 18,568 | 13 |
| Bubandi | 9 | 9,425 | 10 |
| Kisubba | 19 | 21,112 | 9 |
| Mirambi | 9 | 10,115 | 9 |
| Bubukwanga | 12 | 14,184 | 9 |
| Butuma-Mitunda TC | 5 | 7,019 | 7 |
| Kirumya | 8 | 13,971 | 6 |
| Ntotoro | 5 | 13,130 | 4 |
| Bundigoma | 2 | 5,733 | 4 |
| Busunga tc | 4 | 11,915 | 3 |
| Bukonzo | 2 | 8,382 | 2 |
| Ndugoto | 1 | 7,257 | 1 |
| Ntandi TC | 1 | 9,478 | 1 |
| Sindila | 1 | 9,705 | 1 |
| Mabere | 2 | 5,857 | 3 |
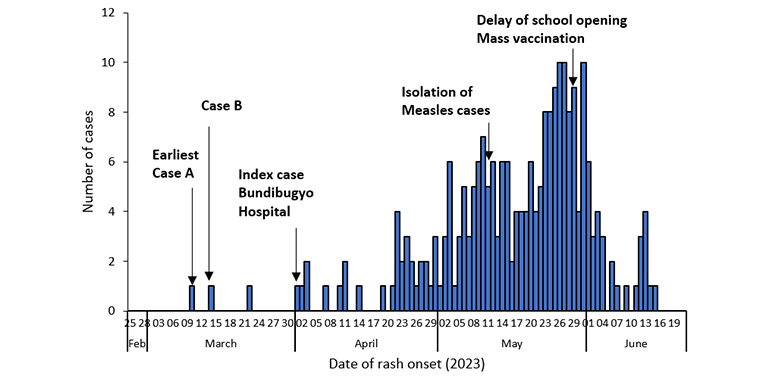
The epidemic curve revealed a propagated measles outbreak, with the primary case having rash onset on March 10th, 2023. The primary case-person had arrived from DRC on February 27th, 2023, and developed fever on March 4th,2023 followed by a generalized maculopapular rash on March 10th, 2023. This implies that he was infectious from about March 6th, 2023 since measles case-patients are known to be infectious 4 days before and after the onset of rash. The first secondary case was a 2-year-old son to the primary case and had onset of rash on 14th March 2023. The index case was identified on 1st April 2023, at Bundibugyo hospital. More cases appeared after 31st March 2023 and there have been no reported cases since 15th June 2023 (Figure 2).
Laboratory investigation
The measles strain responsible for the outbreak was the B3 measles virus following molecular gene sequencing.
Environmental assessment
We found that there was generally unregulated movement of persons to and from either side of the border, and no screening of incoming persons from DRC. We got reports from members of the border community about a similar illness that had been in DRC since February 2023.
We also found out that there was mixing up of measles case-patients and other patients on the pediatric ward of Bundibugyo hospital in the early weeks of outbreak. The isolation facility was established after about 2 weeks from when the first confirmed case visited the facility. The nursing staff on the ward informed us that they started seeing suspicious cases as early as March 2023 but their reports were ignored by the medical officers. There was also lack of functional triage at all health facilities, even after the outbreak was confirmed.
Hypothesis-generating interview findings
The hypothesis generation findings suggested that the potential risk factors for measles transmission were: attending school, not being vaccinated, visiting a water collection point, attending a health facility and attending any place of worship before falling sick before falling sick within 3 weeks before falling sick (Table 2).
Table 2: Hypothesis generation interview findings
| Risk factors | Percentage (%) |
| Attending school within 3 weeks before falling sick | 89 |
| Not vaccinated against measles | 71 |
| Visiting a water collection point | 57 |
| Attending a health facility | 55 |
| Attending a place of worship | 54 |
| Playing away from home | 45 |
| Attending a social gathering | 29 |
| Travel outside Bundibugyo district | 18 |
| Receiving a visitor | 14 |
Case-control study findings
Being unvaccinated against measles increased the odds of measles infection 6 times (aOR 6.13 (2.5, 15.0)) (Table 3). In addition, meeting a symptomatic person during a health facility visit was associated with a 3-fold increase in the odds of measles infection, compared to those who never visited a health facility (aOR 3.7(1.01, 13)
Table 3: Multivariate analysis of risk factors for Measles transmission in Bundibugyo District, February-June 2023
Measles vaccine effectiveness
We estimated vaccine effectiveness at 87% (CI 69,94) among respondents above 9 months of age (Table 4).
Table 4: Measles vaccine effectiveness by age, Bundibugyo District, May-June 2023
| Age | Vaccination status | Frequency (%) | ORMH (95% CI) | Vaccine effectiveness | |
| Cases
(n=62) |
Controls
(n=117) |
||||
| Overall
(9 months-60 years) |
Vaccinated | 27(44) | 101(86) | 0.13(0.14,0.31) | 87(69,94) |
| Not vaccinated | 35(56) | 16(14) | Ref | ||
Measles vaccination coverage
Approximately eighty-six percent (101/117) of the controls above the age of 9 months had received at least one dose of measles vaccine. Thus, the estimated vaccine coverage was 86%.
Discussion
Our investigation revealed that being unvaccinated against measles, and meeting someone with a rash during a health facility visit increased the odds of measles infection during the measles outbreak in Bundibugyo District. Molecular laboratory findings showed that the outbreak was due to the measles B3 strain. The most affected sub-counties were Bundibugyo town council and Tokwe sub-county.
The vaccination coverage of 86% was way below the recommended minimum target of 95%, required for herd immunity (9). This lack of herd immunity facilitated the outbreak and spread of the measles, following its introduction by the earliest identified case who had recently returned from an affected village in DRC.
The estimated coverage also grossly contrasts the administrative district coverage, and is much lower than the reported coverage of 114% (10), suggesting data quality gaps.
Poor triage at health facilities, particularly Bundibugyo hospital facilitated the transmission and amplified the measles outbreak. During the first three weeks of the outbreak, measles case-patients admitted to the pediatric ward were mixed with other patients, who would days later, be readmitted with measles infection.
The most affected sub-county of Tokwe and Bundibugyo town council are closely linked to DRC by the physical border and trade activities respectively. The porous border entry points with unregulated entry and exit of persons along with lack of routine screening of persons likely introduced the measles virus into a population. The primary case-patient returned to Uganda from DRC via one of the s border points at Butogho village, Kisubba subcounty and proceeded to Nyahuka subcounty.
Study limitations
Recall bias from parents who had lost their vaccination cards and children whose caretakers who did not have clear vaccination and exposure information which might have led to over estimation or under estimation of vaccination status. We relied on knowledge of site of vaccination at 9 months to establish vaccination status. Most cases were identified through active case search at health facilities and this could have introduced selection bias. We used proportion of vaccinated controls in the affected sub counties to estimate vaccine coverage which may not have been representative of the coverage in the entire district.
Conclusion
The outbreak was facilitated by the low measles vaccination coverage and suboptimal vaccine effectiveness in the affected sub counties. We recommended mass vaccination campaign and scale up of routine immunization activities while observing good cold chain practices. We further recommended the following measures to mitigate the risk of future outbreaks in Bundibugyo District: routine measles vaccination through sustained daily static clinics and outreaches, proper triaging of all patients at care-entry points in all departments by health facility managers, improvement on health education on immunization, and ensuring that at least one isolation room is established and maintained at all high-volume health facilities to prevent mix-up of patients with contagious diseases.
Public Health Actions
Following the investigation, we conducted a mass measles immunization campaign targeting all children aged 6-59 months regardless of prior immunization for measles at health facilities of all affected sub counties. The District task force supported mass measles vaccination by delaying school opening for one week. The District Health Officer redistributed key drugs and supplies for measles case management to support the established isolation units. We intensified case-finding through active search at health facilities and communities and emphasized set up of triage and temporary holding areas at all outpatient departments
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
We acknowledge the support of Bundibugyo District Local Government and community members in this study. We also appreciate the Uganda Public Health Fellowship Program and the Ministry of Health, Public Health Emergency Operations Centre for the technical support offered during this study. We also thank the US-CDC for the funding.
Copyright and licensing
All materials in the Uganda Public Health Quarterly Epidemiological Bulletin are in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Griffin DE, Ward BJ, Esolen LM. Pathogenesis Of Measles Virus Infection: An Hypothesis For Altered Immune Responses. The Journal of Infectious Diseases. 1994;170(Supplement_1):S24-S31.
- Bester JC. Measles and Measles Vaccination: A Review. JAMA Pediatrics. 2016;170(12):1209-15.
- Naniche D. Human immunology of measles virus infection. Measles: Pathogenesis and Control. 2009:151-71.
- Mina MJ, Kula T, Leng Y, Li M, de Vries RD, Knip M, et al. Measles virus infection diminishes preexisting antibodies that offer protection from other pathogens. Science. 2019;366(6465):599-606.
- Rota JS, Hickman CJ, Sowers SB, Rota PA, Mercader S, Bellini WJ. Two Case Studies of Modified Measles in Vaccinated Physicians Exposed to Primary Measles Cases: High Risk of Infection But Low Risk of Transmission. The Journal of Infectious Diseases. 2011;204(suppl_1):S559-S63.
- Moss WJ, Polack FP. Immune responses to measles and measles vaccine: challenges for measles control. Viral immunology. 2001;14(4):297-309.
- WHO. Statement from Uganda’s Minister of Health on the National Measles-Rubella and Polio Immunisation Campaign 2019 2019 [Available from: https://www.afro.who.int/news/statement-ugandas-minister-health-national-measles-rubella-and-polio-immunisation-campaign.
- Statistics UE. Uganda Bureau of Statistics. Energy. 2022;95(13.6):14.5.
- Immunization WHODo. Immunization in practice: a practical guide for health staff: World Health Organization; 2015.
- Health Mo. 2023 [updated 15-6-2023. Available from: https://hmis.health.go.ug/dhis-web-data-visualizer/index.html#/.


Comments are closed.