COVID-19 vaccine uptake and coverage, Uganda, 2021-2022
Authors: Patrick King1*, Mercy Wendy Wanyana1, Richard Migisha1, Daniel Kadobera1, Benon Kwesiga1, Biribawa Claire2, Michael Baganizi2, and Alfred Driwale2; Institution affiliation: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda, 2Uganda National Expanded Program on Immunization, Ministry of Health, Kampala, Uganda; *Correspondence: Email: kingp@uniph.go.ug, Tel: +256775432193
Summary
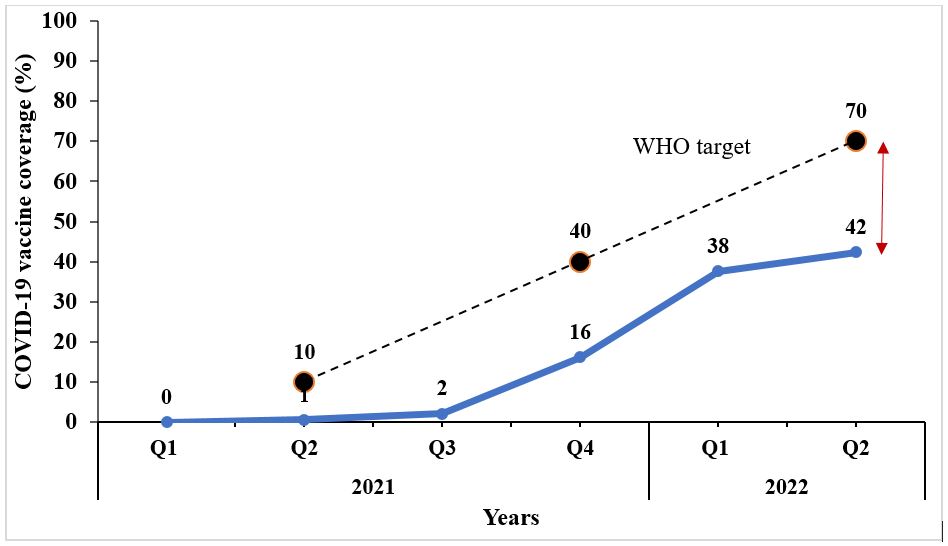
Background: Vaccination against COVID-19 reduces COVID-19-associated mortality, severe disease, and hospitalization, and the potential for the severity of future COVID-19 waves. Uganda began COVID-19 vaccination in March 2021 and has used a variety of vaccines, including AstraZeneca, Johnson & Johnson, Moderna, Pfizer, Sinopharm, and Sinovac. The World Health Organization (WHO) Global strategy on COVID-19 vaccination targeted national coverage of 10% by September 2021, 40% by December 2021, and 70% by June 2022. We assessed COVID-19 vaccination uptake and coverage in Uganda during March 2021 through June 2022 to evaluate progress towards targets and identify gaps for evidence-based recommendations.
Methods: We conducted descriptive analysis of COVID19 vaccination data from the national COVID-19 vaccination database, March 2021-June 2022. Vaccine uptake was defined as the proportion of the population vaccinated with ≥1 COVID-19 vaccine dose. Coverage was the proportion of persons who had received the full number of doses (‘schedule’) of the relevant vaccine. For single-dose vaccines, uptake equaled coverage. We calculated uptake and coverage at national, regional, and district levels and also disaggregated by sex and age groups. We used chi-square test to assess differences between categories.
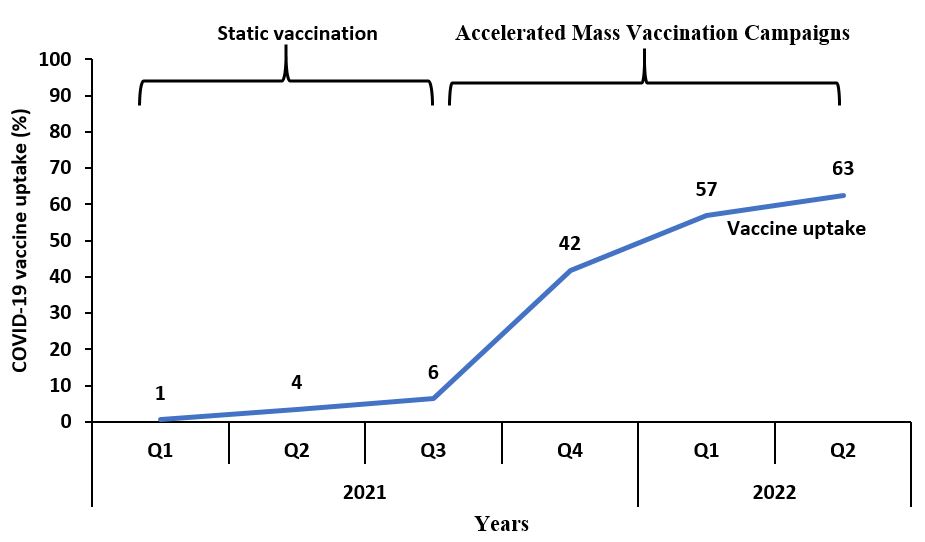
Results: In total, 17,369,476 individuals received ≥1 COVID-19 vaccine dose, and 11,833,911 individuals had received the full schedule by June 2022. National uptake (6% in September (Q3) 2021, 42% in December (Q4) 2021, and 63% by June (Q2) 2022) and coverage (2% in Q3 2021, 16% in Q4, 2021, and 42% in Q2 2022) were below WHO targets. Western Region (33.2%) had significantly higher coverage than Eastern (31.4%), Central (22.4%), and Northern regions (21.6%) (p<0.0001). Females (10.6%) had higher coverage than males (8.6%) (p<0.0001). Persons >50 years of age had higher coverage (24.9%) than persons aged 40-49 (21.8%), 30-39 (19.0%), 18-29 (4.7%), and 12-17 (2.9%) years (p<0.0001).
Conclusion: COVID-19 vaccine coverage and uptake were below WHO targets in Uganda by June 2022. The Uganda National Expanded Program for Immunization should carry out targeted vaccination campaigns to improve vaccine uptake and coverage, particularly for groups and areas with the lowest coverage. Programs to continuously monitor the extent of vaccine hesitancy could help increase vaccine demand among the population.
Background
COVID-19 has had massive health and economic impacts globally(1). By June 2022, COVID-19 had contributed to 6 million deaths and more than 38 million infections globally as reported on the World health organization (WHO) dashboard(2). COVID-19 vaccine showed that they could prevent more deaths(3). Consequently, various countries developed several vaccines, with 11 vaccines licensed for emergency use by the WHO. Following this, WHO through the Strategy to Achieve Global COVID-19 Vaccination set a target for each country to vaccinate 70% total population coverage by mid-2022 in order to end the COVID-19 pandemic (4).
Initially, Uganda particularly received its first batch of COVID-19 vaccine in March 2021 through the COVID-19 Vaccines Global Access (COVAX) facility which is a group of organizations that included Coalition for Epidemic Preparedness Innovations (CEPI), Gavi, WHO, and United Nations International Children’s Fund(5). The COVAX facility aimed to ensuring equitable access to COVID-19 vaccines for all countries, regardless of their income level. The first consignment received in Uganda comprised part of 864,000 doses of AstraZeneca vaccine from serum institute of India. Later in December 2021 more than 742,000 doses of AstraZeneca and Moderna vaccines were received from European governments. A total of 1,606,000 doses were availed to the country between March and December 2021 and more doses were received from the United States and other European countries in 2022. Uganda was expected to achieve the initial COVAX short term targets of 3% coverage, and then 20% vaccine coverage through COVAX-secured doses by the end of 2021. This would eventually lead to achievement of the WHO target of 70% of the 44 million population which approximates to 30,800,000 coverage by mid-2022.
Uganda’s COVID-19 Vaccination Implementation Plan (UCVIP) set out to implement COVID-19 vaccination in a coordinated stepwise approach adopting the WHO prioritization framework. The first phase that covered the high priority was from January to March 2021 (Quarter 1) and second phases from April to May 2021 (Quarter 2) prioritized individuals above 18 years (4). The high priority groups included health workers in public and private health facilities, people with co-morbidities above 18 years and teachers; humanitarian and those aged above 50 years of age. There after the third phase (Quarter 3 of 2021) focused on all individuals above 18 years. With current evidence suggesting the safety of vaccines among children aged 5 – 17 years (6, 7), the final phase included on full schedule vaccination for the entire population aged ≥12 years.
Vaccination was initially offered at static sites but to increase uptake, the Ministry of Health (MoH) shifted its strategy to Accelerated Mass Vaccination Campaigns (AMVC). In AMVC, the Ugandan, Ministry of Health increased the number of vaccination points and expanded vaccination access through the establishment of outreaches in communities and at churches, taxi parks, markets among other places.
With the country having a fully re-opened economy and a clearly noted non-adherence to COVID-19 Standard Operating Procedures (SOPs), vaccines remain the most effective public health measure to mitigate the impact of COVID 19. The effectiveness of any vaccination program is dependent on uptake of the vaccine. Although periodic reports on vaccines delivered have been made, no formal assessment of the country’s COVID-19 vaccine uptake and coverage has been made. We assessed progress, compared COVID-19 vaccine uptake and coverage across demographic groups and determined spatial distribution of COVID-19 vaccination uptake and coverage, Uganda, March 2021-June 2022.
Methods
We conducted a descriptive analysis of routinely collected COVID19 vaccination surveillance data obtained from the District Health Information System2 (DHIS2). We specifically obtained data from the EPIVAC, a data base for COVID-19 vaccination in DHIS2. This database contains COVID-19 vaccines administered and social demographic information on vaccinated individuals since March 2021.
We abstracted aggregate data on brand of vaccine received, number of doses received, residence (district, region), risk category (including: Health Care Workers (HCW), Elderly, persons with co-morbidities, and teachers) and socio-demographic variables including: age and gender.
We defined COVID-19 vaccine uptake as the proportion of people vaccinated with at least one COVID-19 vaccine dose. We defined COVID-19 coverage as the proportion of people who had received the full schedule of COVID-19 vaccine (at least two doses of AstraZeneca, Pfizer, Moderna, Sinopharm, Sinovac or one dose Johnson and Johnson).
Data were downloaded in an excel file and imported to Epi info 7 software for analysis. Descriptive statistics including counts and percentages were calculated. Counts on the of type vaccine received and percentages for COVID-19 uptake and coverage were calculated at various time points and across population categories. We calculated uptake as the number of people who had received at least one vaccine dose divided by the eligible population using population statistics obtained from the Uganda Bureau of Statistics. We calculated coverage as the number of people who had received at least one vaccine dose divided by the eligible population using population statistics obtained from the Uganda Bureau of Statistics.
We used logistic regression to evaluate the overall trend for COVID-19 vaccination uptake and coverage using Epi info 7. Chi- square test was used to compare the COVID-19 vaccine coverage and COVID-19 uptake across regions. We drew choropleth maps using QGIS to show the spatial distribution across districts.
We obtained permission to use the COVID19 vaccination data from the Ministry of health. Data was stored on a password protected computer and only accessed by the study team. Data abstracted did not have unique identifier information. We also obtained a non-research determination from the US CDC.
Results
Vaccine doses received by eligible population, Uganda, March 2021-June2022
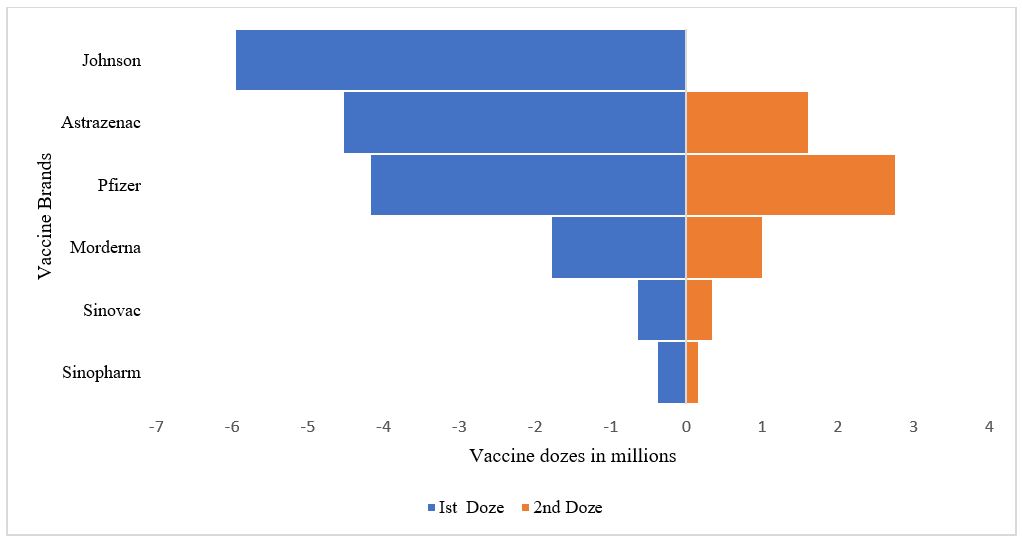
Between March 2021 and June 2022, the eligible population received both single (Johnson & Johnson) and two dose vaccines regimens (AstraZeneca, Moderna, Pfizer, Sinopharm and Sinovac). Johnson and Johnson vaccine was only one single dose vaccine received. Among two dose vaccine regimens, AstraZeneca was the commonest (4,538,682 doses) vaccine received at first dose. While Pfizer was the commonest vaccine received for the second dose (27361366 doses). Sinovac and Sinopharm vaccines were the least received throughout this period (Figure1).
National COVID-19 vaccine uptake progress, Uganda, March 2021- June 2022
For the first phase (Q1) uptake was 33% among teachers, 70% among HCW, 47% among people living with comorbidities. For the second phase (Q2) uptake was 7% among the elderly. The national vaccine uptake was < 10% from March to end of September 2022. Thereafter there was a rapid increase (35%) in vaccine uptake between September and December 2022. By the end of June 2022, vaccine uptake was 62.5%. Overall, the national vaccine uptake increased by 45% (OR:1.45, CI:1.44-1.45, p-value <0.001) between march 2021-June 2022 (Figure 2).
National COVID-17 vaccine coverage progress, Uganda, March 2021- June 2022
The national COVID-19 vaccination coverage was < 10% between quarter 1 and 3, 2021. Thereafter national COVID-19 vaccination coverage rapidly increased between quarter 3 2021 and quarter 1, 2022. By end of quarter 2, 2022 the national vaccine coverage was 42.4%. Overall, there was a 41% increase (OR:1.41, CI:1.41-1.41, p-value <0.001) increase in COVID-19 vaccine coverage, March 2021-June 2022.
Difference in COVID19 Vaccine uptake and Coverage, Uganda, March 2021-June 2022
Differences in COVID19 vaccine uptake and coverage were observed across age groups, gender, and region (Table 1). Both coverage and uptake were higher among females compared to males. The oldest age group (> 50 years) had higher coverage and uptake compared to younger age groups. The Western Region had the highest coverage and uptake compared to the other regions
Table 1: Differences in COVID19 Vaccine uptake and Coverage, Uganda, March 2021 – June 2022
| Characteristics | Uptake | Coverage | |||
| % | P-value | % | P-value | ||
| Age group
12-17 18-29 30-39 40-49 > 50 |
5.9 17.4 26.7 36.5 40.8 |
<0.001
|
2.9 4.7 19.0 21.8 24.9 |
<0.001
|
|
| Gender
Male Female |
49.2 58.2 |
<0.001
|
13.8 16.4 |
<0.001
|
|
| Region
Central Eastern Northern Western |
35.2 40.5 32.8 51.2 |
<0.001
|
22.6 31.4 21.6 33.2 |
<0.001
|
|
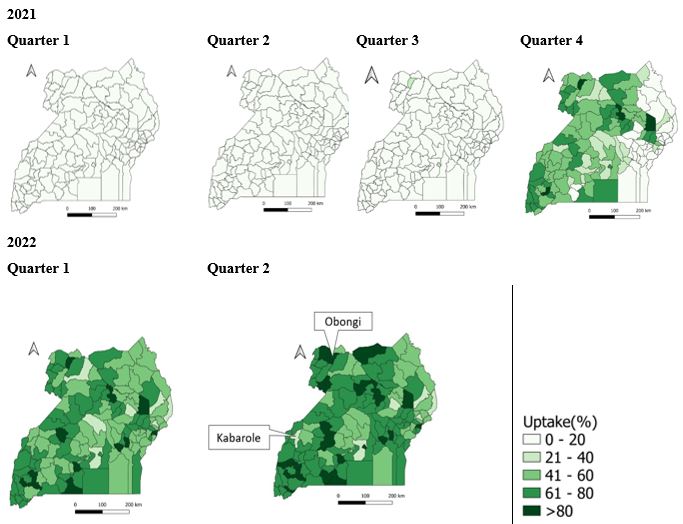
Spatial distribution of COVID-19 vaccine uptake, Uganda, March 2021-June 2022
The national COVID19 vaccine uptake was generally low across all districts between quarter 1 and quarter 3 2021. By the end of quarter 2, 25 districts had a COVID19 vaccine uptake above 80% with the highest percentage of vaccine uptake captured in Obongi District. The lowest recorded vaccine uptake by June 2022 in Uganda was in Kabarole District (Figure.4).
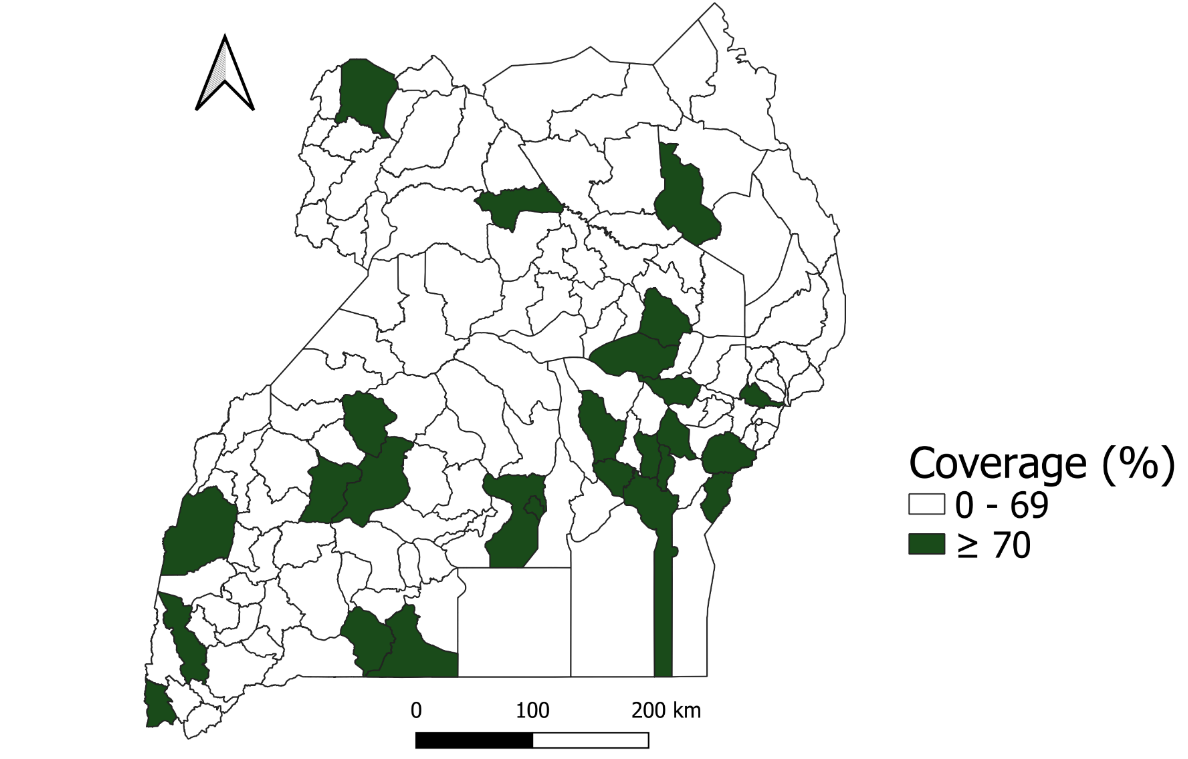
Spatial distribution of COVID-19 vaccine coverage, Uganda, March 2021-June 2022
Overall, 25 districts were able to achieve the WHO target of having 70% of their population fully vaccinated by June 2022. These districts were mainly in the western, eastern, and central parts of the country (Figure 5). Among the districts that did not achieve the target, coverage ranged between 1% to 69%. Twenty-four districts mainly in the Nothern Region had <10% of their populations fully vaccinated against COVID-19 by June 2022.
Discussion
Our findings showed that a variety of COVID-19 vaccines were received by the Ugandan population with a national COVID-19 vaccine uptake of 63% and coverage of 42%, females, individuals >50 years, and those residing in Western Region had significantly higher coverage compared to males, individuals aged 12-17 years, and those residing in the Northern Region by the end of June 2022.
COVID-19 vaccination uptake steadily increased, however, remained lower than anticipated by the Uganda COVID-19 Vaccination Implementation Plan (UCVIP). This plan targeted to have all eligible persons vaccinated by the end of 2022. Previous studies conducted in Uganda had indicated that a high proportion of people was willing or intended to receive a COVID-19 vaccine(8) . The low uptake despite a high willingness to be vaccinated suggests the presence of other barriers that may influence COVID-19 vaccination uptake. A study in Ghana indicated that barriers such as limited supplies of vaccines and long queues could negatively influence COVID19 vaccine uptake (9).
Similar to other studies(10, 11) conducted in Africa, coverage was low. A study by Afolabi et al (11) in 15 West African countries indicated that coverage was on 0.27% by June ’21 which is comparable to 0.4% in Uganda in the same period. In other East African countries like Kenya, a study by Muchiri et al (10) showed coverage to be 30.75% by March 2022 which is below the anticipated WHO target. The low coverage of the COVID-19 vaccine could be attributed to several factors such as lack of competence, infrastructure, logistics and financial resource (12). Another study by Kabagenyi et al in Uganda attributes low coverage to vaccine hesitancy among the population(13).
Our study found differences in COVID-19 coverage across gender, age group, and region, suggesting health inequalities(14, 15). However, unlike other studies in low income countries, vaccine coverage in our study was higher among females compared to males(14). This might suggest unique differences in the Ugandan context. The low coverage of the COVID-19 vaccine among the 12–17year age group could be attributed for the delayed approval of COVID-19 vaccines and eventual roll out in this age group. Globally, approval was obtained mid-2021 and roll out in Uganda only began in 2022(16). The higher coverage among older age groups compared to the other groups could be attributed to their perceived severity of the COVID-19 infection, making them more likely to complete their vaccination(17). Regional differences could be attributed to differences in roll-out of mass vaccination campaigns based on prevalence of COVID-19. The high coverage of COVID-19 vaccination in the eastern and western regions could be attributed to intensified vaccination campaigns following high prevalence of COVID-19 infections.
The study had the following limitations. We used aggregate data therefore our findings can be applied to groups rather individuals(17).We used the national COVID-19 database which may not have been up to date due to delays in data entry. This could have led to underestimation of the true uptake and coverage of COVID-19 vaccination. However, use of nationwide data allows generalization of the findings to the entire country.
Conclusion
By June 2022, Uganda’s COVID-19 vaccination coverage fell short of the goals set by the WHO. The COVID-19 vaccine uptake and coverage were increased when vaccination strategy was changed from static to accelerated mass vaccination. The National Expanded Program for Immunization should continue and expand this strategy to focus its efforts to vaccinate a high percentage of persons in the high priority groups with tailored efforts for groups that lie behind. The programs should continuously track progress to identify groups that need intensified efforts in order to increase coverage.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
The authors appreciate the Ministry of Health for providing access to DHIS2 data that was used for this analysis. We appreciate the technical support provided by the Division of Surveillance, Information and Knowledge Management and the Uganda National Expanded Program for Immunization. Finally, we thank the US-CDC for supporting the activities of the Uganda Public Health Fellowship Program (UPHFP).
Copyright and licensing
All materials in the Uganda National Institute of Public Health Quarterly Epidemiological
Bulletin is in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Oum S, Kates J, Wexler A. Economic Impact of COVID-19 on PEPFAR Countries. KFF; 2022.
- Kim SY, Yeniova AÖ. Global, regional, and national incidence and mortality of COVID-19 in 237 countries and territories, January 2022: a systematic analysis for World Health Organization COVID-19 Dashboard. Life Cycle. 2022;2.
- Rahman MA, Islam MS. Early approval of COVID-19 vaccines: Pros and cons. Human Vaccines & Immunotherapeutics. 2021;17(10):3288-96.
- Organization WH. Strategy to achieve global COVID-19 vaccination by mid-2022. Geneva: World Health Organization. 2021.
- de Bengy Puyvallée A, Storeng KT. COVAX, vaccine donations and the politics of global vaccine inequity. Globalization and Health. 2022;18(1):1-14.
- Oliver SE, Wallace M, Link-Gelles R. COVID-19 vaccines: Safe and effective in children aged 5 to 11 years. Pediatrics. 2022;150(2).
- Rudan I, Millington T, Antal K, Grange Z, Fenton L, Sullivan C, et al. BNT162b2 COVID-19 vaccination uptake, safety, effectiveness and waning in children and young people aged 12–17 years in Scotland. The Lancet Regional Health-Europe. 2022;23:100513.
- Echoru I, Ajambo PD, Keirania E, Bukenya EEM. Sociodemographic factors associated with acceptance of COVID-19 vaccine and clinical trials in Uganda: a cross-sectional study in western Uganda. BMC Public Health. 2021;21(1):1106.
- Afrifa-Anane GF, Larbi RT, Addo B, Agyekum MW, Kyei-Arthur F, Appiah M, et al. Facilitators and barriers to COVID-19 vaccine uptake among women in two regions of Ghana: A qualitative study. PLOS ONE. 2022;17(8):e0272876.
- Muchiri SK, Muthee R, Kiarie H, Sitienei J, Agweyu A, Atkinson PM, et al. Unmet need for COVID-19 vaccination coverage in Kenya. Vaccine. 2022;40(13):2011-9.
- Afolabi MO, Wariri O, Saidu Y, Otu A, Omoleke SA, Ebenso B, et al. Tracking the uptake and trajectory of COVID-19 vaccination coverage in 15 West African countries: an interim analysis. BMJ Glob Health. 2021;6(12).
- Lawal L, Aminu Bello M, Murwira T, Avoka C, Yusuf Ma’aruf S, Harrison Omonhinmin I, et al. Low coverage of COVID-19 vaccines in Africa: current evidence and the way forward. Hum Vaccin Immunother. 2022;18(1):2034457.
- Kabagenyi A, Wasswa R, Nannyonga BK, Nyachwo EB, Kagirita A, Nabirye J, et al. Factors Associated with COVID-19 Vaccine Hesitancy in Uganda: A Population-Based Cross-Sectional Survey. International Journal of General Medicine. 2022:6837-47.
- Ali HA, Hartner A-M, Echeverria-Londono S, Roth J, Li X, Abbas K, et al. Vaccine equity in low and middle income countries: a systematic review and meta-analysis. International journal for equity in health. 2022;21(1):1-30.
- Bayati M, Noroozi R, Ghanbari-Jahromi M, Jalali FS. Inequality in the distribution of Covid-19 vaccine: a systematic review. International journal for equity in health. 2022;21(1):1-9.
- Olson SM, Newhams MM, Halasa NB, Price AM, Boom JA, Sahni LC, et al. Effectiveness of Pfizer-BioNTech mRNA Vaccination Against COVID-19 Hospitalization Among Persons Aged 12-18 Years-United States, June-September 2021. MMWR Morbidity and mortality weekly report. 2021;70(42):1483.
- Basta NE, Sohel N, Sulis G, Wolfson C, Maimon G, Griffith LE, et al. Factors associated with willingness to receive a COVID-19 vaccine among 23,819 adults aged 50 years or older: an analysis of the Canadian longitudinal study on aging. American Journal of Epidemiology. 2022;191(6):987-98.


Comments are closed.