Trends and spatial distribution of perinatal deaths, Uganda: a descriptive analysis of surveillance data, 2017 – 2021
Authors: Brian Agaba1*, Hellen Naiga Nelly1, Zainah Kabami1, Saudah Namubiru Kizito1, Brenda Simbwa1, Robert Zavuga1, Robert Mutumba2, Bruno Ssemwanga2, Carol Nanziri1, Daniel Kadobera1, Lilian Bulage1, Richard Migisha1, Alex Riolexus Ario1; Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda, 2Reproductive Health Division, Ministry of Health, Kampala, Uganda; *Correspondence: Email: agababrian@uniph.go.ug, Tel: +256774125554
Summary
Background: Over the last two decades, there have been multiple interventions aimed at reducing the burden of perinatal deaths in Uganda. These include perinatal death audits and newborn care packages. Despite this, the country has not reached the World Health Organization (WHO)/Every newborn action plan (ENAP) target of <12 still births per 1,000 births and <12 newborn deaths per 1,000 live births. We describe temporal and spatial trends of perinatal deaths during 2017 to 2021 to evaluate progress towards targets.
Methods: We extracted data on macerated stillbirths (MSB), fresh stillbirths (FSB), early newborn deaths (END), livebirths, and total births from the District Health Information System (DHIS2), 2017–2021. As per the DHIS2, FSB was intrauterine death of a fetus ≥28 weeks of gestation or ≥1,000 grams; MSB was intrauterine death of a fetus before labor onset in which the fetus showed degenerative changes, and END was death of a baby (≥28 weeks of gestation/≥1,000g) at 0-7 days of life. MSB, FSB, and END were summed to obtain total perinatal deaths; rates were calculated per 1,000 total births. We analyzed trends using logistic regression and described spatial distribution by district.
Results: Among 139,948 perinatal deaths (53,001 MSB, 51,566 FSB and 35,381 END), the annual average perinatal death rate was 23/1,000 births, reducing by an average of 8% per year from 28/1,000 in 2017 to 19/1,000 in 2021 (OR=0.92, CI=0.91-0.92). Stillbirths declined by an annual average of 6%(OR=0.94, CI=0.94-0.95). Early newborn deaths declined at an annual average of 9%(OR=0.91, CI=0.90-0.9). Districts with regional referral hospitals such as Masaka, Hoima, Mubende, Jinja, and Kampala reported the highest perinatal death rates.
Conclusion: Perinatal deaths declined between 2017 and2021 but remained above the WHO /ENAP target. The ministry of health could focus perinatal death reduction interventions and resources to districts with regional referral hospitals.
Introduction
A perinatal death is defined as death of a fetus after 28 weeks of pregnancy up to 7 days of life. It encompasses both stillbirths and early newborn deaths. Perinatal deaths persist as a global public health problem. In 2021, perinatal deaths were responsible for 75% of the 2.3 million children that died in the first month and 47% of all under-5 year child deaths in the world[1]. Each year, 1.4 million perinatal deaths occur in Sub-Saharan Africa[2-4]. Developing countries contribute 98% of the global burden of perinatal deaths[5].
In Uganda, perinatal deaths are still persistently high. The 2016 demographic health survey indicates a perinatal death rate of 38 per 1,000 births[6]. In Uganda, perinatal deaths are caused by prematurity, birth asphyxia, obstructed labor, birth trauma, infections, and congenital anomalies[7, 8]. The causes of perinatal deaths in Uganda are largely preventable thus providing opportunities for prevention and reduction strategies.
In response to the high rates, Uganda has implemented interventions to end preventable perinatal deaths for over two decades. Interventions such as perinatal death notification and audits, increasing antenatal care coverage, increasing proportion of births attended to by a skilled birth attendant, essential newborn care package, and family planning have been implemented[9, 10]. However, these interventions have yielded less than expected outcomes as perinatal death rates remain above the World Health Organization/Every Newborn Action Plan target of less than 12 stillbirths per 1,000 total births and less than 12 newborn deaths per 1,000 livebirths[11].
Through perinatal death surveillance, Uganda collects perinatal death data from all health facilities that conduct deliveries. This data is critical in understanding the progress towards meeting targets and is essential in evaluating effectiveness and impact of prevention strategies. Despite this, there is limited national level analysis and documentation of trends and distribution of perinatal deaths. We described trends and spatial distribution of perinatal deaths in Uganda, 2017 – 2021, to inform interventions.
Methods
Study design and data source
We conducted a descriptive analysis of perinatal surveillance data captured in the District Health Information System version 2 (DHIS2). The DHIS2 is an electronic database that contains nationwide data on health conditions of interest. All health facilities that conduct deliveries are mandated to report data. This data is stored in DHIS2. As per DHIS2, perinatal death was defined as the death of a fetus after 28 completed weeks of pregnancy up to seven days of life. Perinatal deaths are the sum of macerated stillbirths (MSB), fresh stillbirths (FSB), and early (0-7 days) newborn deaths (END). FSB was defined as the intrauterine death of a fetus ≥28 weeks of gestation / ≥ 1,000 grams during labor or delivery. MSB was defined as the intrauterine death of a fetus sometime before the onset of labor, where the fetus showed degenerative changes. END was defined as death of a baby (≥28 weeks of gestation/≥1,000g) between birth and 7 days of life.[4]
Study variables, data collection, and data management and analysis
We abstracted nationwide data using pivot tables from DHIS2 on MSB, FSB, END, livebirths, total deliveries in the health facilities and reporting rates, January 2017- December 2021.
Data on MSB, FSB, and END were summed up to generate total number of Perinatal Deaths. Perinatal death rate was calculated by dividing the perinatal deaths by total number of deliveries. The perinatal death rate was expressed per 1,000 total births. Perinatal death rates were calculated by health facility level, district, and year. We calculated average annual percentage change in stillbirth, END, and perinatal deaths rate.
We demonstrated annual trends in perinatal death rates using line graphs. We performed logistic regression analysis to determine significance of trends using Epi info version 7.25. Choropleth maps were drawn using Quantum Geographic Information System (QGIS) to show the distribution of districts with perinatal deaths twice (>24/1,000) the WHO target.
Ethical considerations
We obtained permission to use data from the Ministry of health. Data was stored on a password protected computer and only accessed by the study team. Data abstracted did not have unique identifier information. We also obtained a non-research determination from the US CDC.
Results
Annual average perinatal death rate, Uganda, 2017-2021
Over the study period (2017 – 2021), 139,948 perinatal deaths were reported in DHIS2. Of these, 53,001(38%) were MSB, 51,566 (37%) were FSB, and 35,381(25%) were END. The annual average perinatal death rate was 23/1,000 births.
Temporal trends in annual perinatal deaths incidence, Uganda, 2017 – 2021
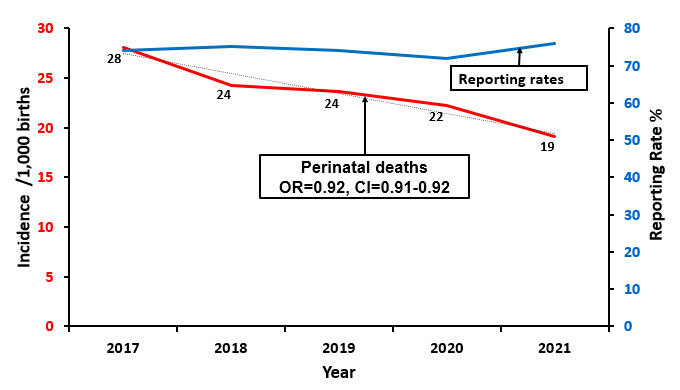
The perinatal death rate declined by an average of 8% per year from 28/1,000 births in 2017 to 19/1,000 births in 2021. The greatest decline was between 2017 and 2018 (Figure 1). Reporting rates where stable over the study period (74% –76%) (Figure 1).
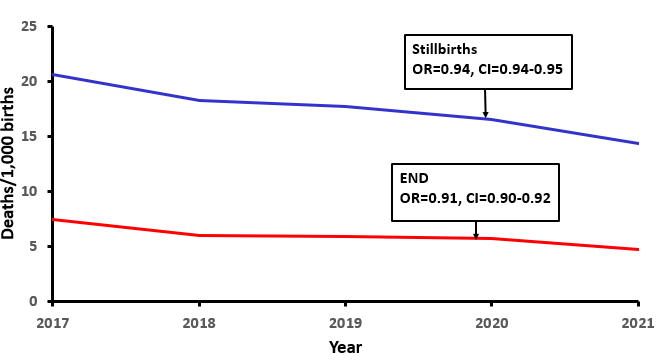
Stillbirths declined at a slower rate of 6% per year compared to END that declined at 9% per year (Figure 2).
Trends in perinatal deaths incidence, health facility level, Uganda, 2017 – 2021
We observed that regional referral hospitals (RRH) and general hospitals had higher perinatal death rates compared to lower health facilities (Health center IV and III) (Figure 3).
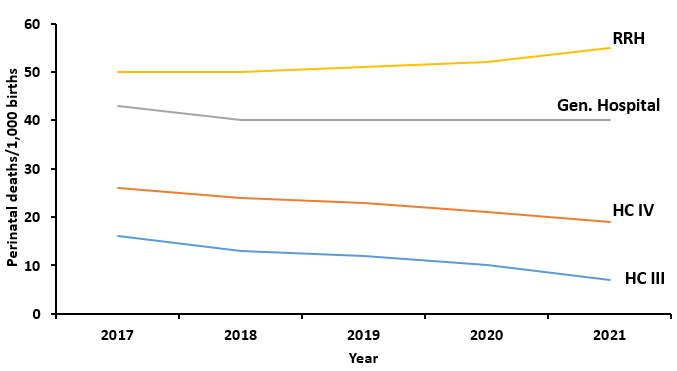
RRH: Regional referral hospital, Gen. Hospital: General hospital, HC IV: Health centre four, HC III: Health centre three
Distribution of perinatal deaths incidence, district level, Uganda, 2017–2021
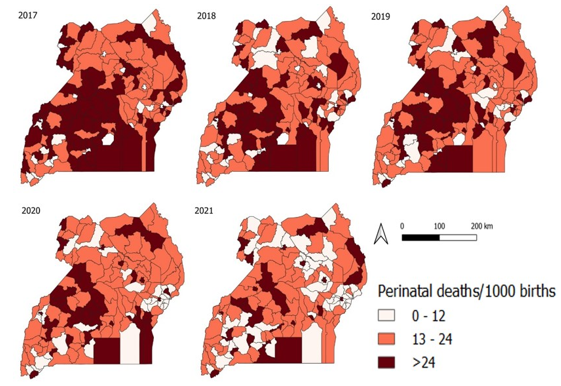
The proportion of districts with perinatal deaths > 24/1,000 decreased from 48% in 2017 to 20% in 2021. Masaka, Hoima, Mubende, Jinja, and Kampala and other districts with regional referral hospitals had perinatal deaths > 24/1,000 throughout the study period. (Figure 4).
Discussion
In our assessment of the distribution, temporal, and spatial trends of perinatal deaths in Uganda, 2017 to 2021, we observed a significant decline of perinatal deaths by an average of 8% per year. Stillbirths contributed the bulk of perinatal deaths over the study period. Districts with regional referral hospitals had higher perinatal deaths compared to other districts.
The positive trend in reduction of perinatal deaths in Uganda mirrors that of the world. The WHO estimates that the global number of newborn deaths declined from 5 million in 1990 to 2.4 million in 2020[12]. However, our study highlights a higher reduction in perinatal deaths compared to other African countries. Between 1990 and 2021, neonatal mortality decreased by 1.7% per year in sub-Saharan Africa[13]. In the last decade, Uganda was a beneficiary of increased funding, technical assistance, and political will for newborn and child health interventions. This could have led to the great magnitude in reduction of perinatal deaths.
Stillbirths contributed the bulk of perinatal deaths, consistent with other studies that have reported that stillbirths contribute more than 50% of perinatal deaths in developing countries[14]. Stillbirth rates are an indicator of quality of obstetric care. In developing countries such as Uganda, high stillbirth rates are due to lack of access to quality antenatal and delivery care[15-17]. A study in Western Uganda found that none of the mothers received appropriate intrapartum care[15, 18]. Another study done at the national referral hospital in Uganda found that monitoring of labor was incomplete in 61% of patients[19]. Despite making gains in antenatal care attendance and proportion of births attended by a skilled birth attendant, stillbirths in Uganda remain high suggesting a lack of quality in these services.
Districts with regional referral hospitals had perinatal deaths in excess of 24/1000 births throughout the study period. Perinatal deaths are reported from the health facility where they occur and not the health facility of origin[20]. Therefore, districts with regional referral hospitals receive patients from facilities in districts without referral hospitals. Uganda’s health care referral system is plagued by several shortfalls such as delays in transportation, poor transportation means, and incomplete referrals [21].This could explain the high perinatal death rates at regional referral hospitals.
Limitations
This study had a couple of limitations. First, it only looked at reported perinatal deaths. These were more likely to be health facility perinatal deaths. A number of community perinatal deaths could have been missed out leading to underestimation of the burden of perinatal deaths. Second, we utilized secondary data. There was missing data on the full range of variables necessary to comprehensively assess the problem of perinatal deaths in the country.
Conclusion
Although Uganda registered significant decline in perinatal deaths from 2017 to 2021, there is still need for improved efforts to meet the global reduction target by 2030. The ministry of health and its partners could focus on areas and health facilities that had persistently high perinatal deaths during this time period.
Conflict of interest
The authors declare that they had no conflict of interest.
Acknowledgments
The authors would like to thank the Ministry of Health and the Reproductive Health Division for their permission and support in accessing the data utilized in this project.
Copyright and licensing
All materials in the Uganda National Institute of Public Health Quarterly Epidemiological Bulletin is in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- WHO, Fact sheet: Newborn Mortality. 2022, WHO.
- Network, H.N. Africa Newborn Network. 2022 [cited 2022 8/12/2022]; Available from: https://www.healthynewbornnetwork.org/partner/africa-newborn-network/.
- UNICEF. Stillbirth. 2020 October 2020 [cited 2022 7/12/2022]; Available from: https://data.unicef.org/topic/child-survival/stillbirths/.
- WHO, Stillbirths. 2022, WHO: Geneva Switizerland.
- UNICEF, Neonatal Mortality. 2021: New York , USA.
- UDHS, U.B.o.S., Uganda demographic and health survey 2016. 2016, UBOS: Kampala.
- Arach, A.A.O., et al., Perinatal death in Northern Uganda: incidence and risk factors in a community-based prospective cohort study. Glob Health Action, 2021. 14(1): p. 1859823.
- Musaba, M.W., et al., Incidence and determinants of perinatal mortality among women with obstructed labour in eastern Uganda: a prospective cohort study. Maternal Health, Neonatology and Perinatology, 2021. 7(1): p. 13.
- Serbanescu, F., et al., Impact of the Saving Mothers, Giving Life Approach on Decreasing Maternal and Perinatal Deaths in Uganda and Zambia. Global Health: Science and Practice, 2019. 7(Supplement 1): p. S27-S47.
- Sensalire, S., et al., Saving Mothers, Giving Life Approach for Strengthening Health Systems to Reduce Maternal and Newborn Deaths in 7 Scale-up Districts in Northern Uganda. Glob Health Sci Pract, 2019. 7(Suppl 1): p. S168-s187.
- WHO, The Every Newborn Action Plan. 2015: Geneva, Switzerland.
- WHO, Newborns: improving survival and well-being. 2020: Geneva, Switzerland.
- UNICEF. Neonatal mortality. The neonatal period is the most vulnerable time for a child 2023 january 2023 [cited 2023 31/1/2023]; Available from: https://data.unicef.org/topic/child-survival/neonatal-mortality/.
- Cnattingius, S. and O. Stephansson, The epidemiology of stillbirth. Semin Perinatol, 2002. 26(1): p. 25-30.
- Benova, L., et al., Two decades of antenatal and delivery care in Uganda: a cross-sectional study using Demographic and Health Surveys. BMC Health Services Research, 2018. 18(1): p. 758.
- Sserwanja, Q., et al., Continuum of care for maternal health in Uganda: A national cross-sectional study. PLOS ONE, 2022. 17(2): p. e0264190.
- Ssetaala, A., et al., Antenatal Care Practices Among Hard-to-Reach Fishing Communities on Lake Victoria: A Community-Based Cross-Sectional Survey. Journal of Primary Care & Community Health, 2020. 11: p. 2150132720923101.
- Muwema, M., et al., Perinatal care in Western Uganda: Prevalence and factors associated with appropriate care among women attending three district hospitals. PLOS ONE, 2022. 17(5): p. e0267015.
- Mukisa, J., et al., Level of Partograph completion and healthcare workers’ perspectives on its use in Mulago National Referral and teaching hospital, Kampala, Uganda. BMC Health Serv Res, 2019. 19(1): p. 107.
- Kamwesiga, J., Uganda Health Care System. Kampala, Uganda: Makerere University, 2011.
- Mwanga-Amumpaire, J., et al., A Qualitative Exploration of the Referral Process of Children with Common Infections from Private Low-Level Health Facilities in Western Uganda. Children, 2021. 8(11): p. 996

