Trends of key surveillance performance indicators of acute flaccid paralysis: A descriptive analysis of the surveillance system, Uganda, 2015-2020
Quarterly Epidemiological Bulletin: Volume 6 / Issue 2/Article No. 4 April -June, 2021
Authors: Bob O. Amodan1, 2*, Annet Kisakye3, Daniel Kadobera1, Alfred Driwale2, Alex R. Ario1, 2
Affiliations: 1Uganda Public Health Fellowship Program, Kampala, Uganda; 2Ministry of Health Uganda, Kampala, Uganda; 3World Health Organization, Country Office-Uganda, Kampala, Uganda
*Corresponding author: Email: bomoda@musph.ac.ug, Tel: 0782152194
Summary
Poliovirus infection causes irreversible paralytic disease, presenting as Acute Flaccid Paralysis (AFP). A sensitive AFP surveillance system is central to the overall polio eradication initiative. We described the Uganda’s AFP surveillance performance, 2015-2020, based on the World Health Organization (WHO) recommended epidemiological performance indicators for AFP surveillance.
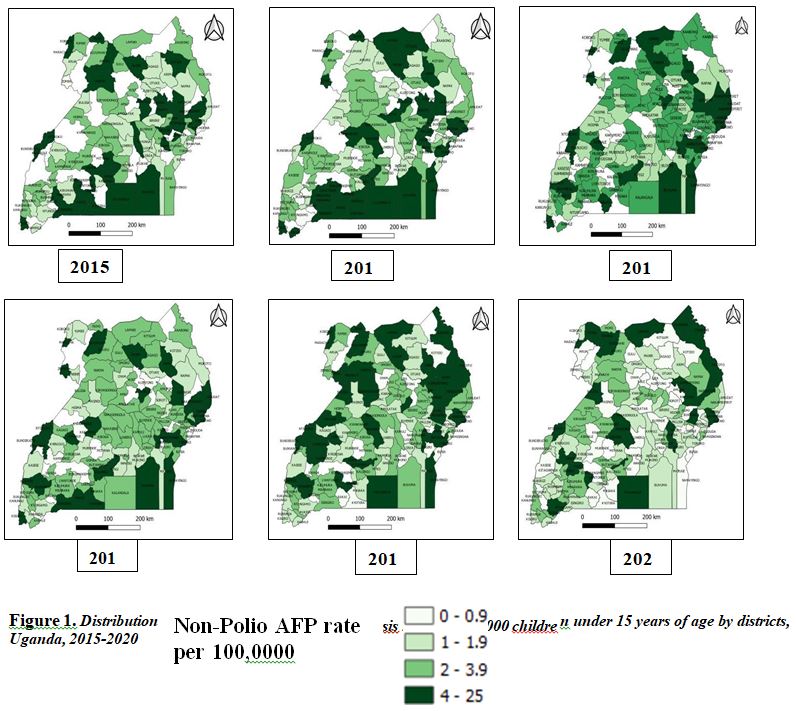
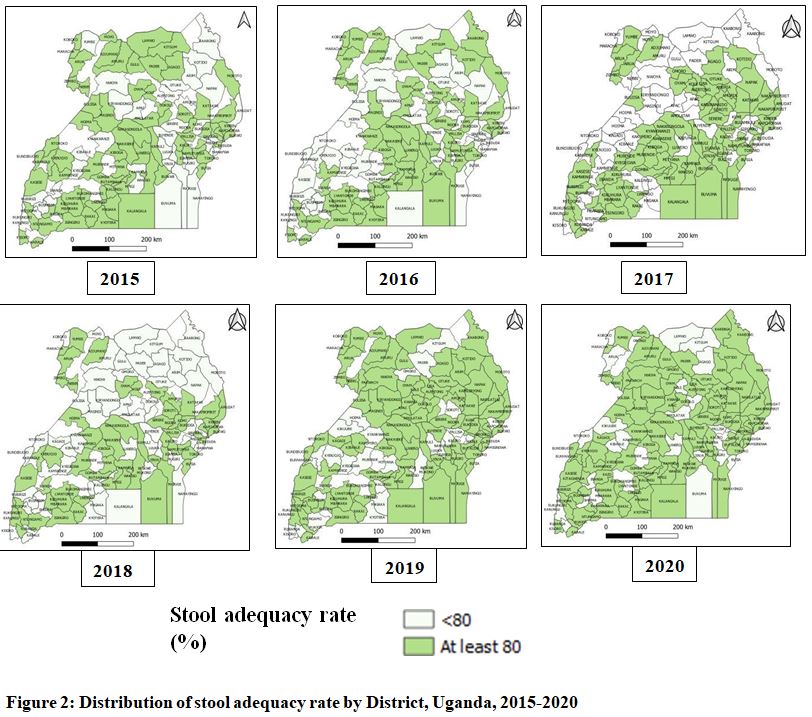
We conducted a retrospective descriptive study using AFP surveillance secondary data submitted to ministry of health and WHO, Uganda office by districts, 2015-2020. Comparisons across the three indicators, including non-polio AFP and stool adequacy rate were made to assess for any relationships therein using trend analysis. We used QGIS to illustrate differences of non-polio AFP and stool adequacy rate across districts.
Of 3,605 AFP cases reported and investigated throughout the Country, 3,475 (96%) were true AFP cases. Majority of the true AFP cases (85%) had received the recommended three and above doses of oral polio vaccine. Of the true AFP cases, none of the detected cases were classified as poliomyelitis, but 445 (13%) AFP cases were caused by non-polio enteroviruses (NPEV). The mean non-polio AFP rate generally declined from 3.1 per 100,000 in 2015 to 2.1 per100,000 in 2020. In every year, less than 40% of the districts achieved the non-polio AFP target rate of at least 4 per 100,000 population of children under 15 years of age. The proportion of districts with non-polio AFP rate of at least 4 per 100,000 significantly declined by 43% (OR=2.2; 95% CI: 1.1-4.1) between 2015 and 2020. Nationally, 2020 recorded the least (20%) proportion of districts that met the minimum non-polio AFP target rate of at least 4 per 100,000 children under 15 years of age. The proportion of districts with stool adequacy rate of at least 80% significantly declined by 15% (OR=0.53; 95% CI: 0.30-0.94) between 2015 and 2020. Nationally, 2018 recorded the least (52%) proportion of districts that met the minimum stool adequacy target rate of at least 80%. The worst performance in AFP surveillance was recorded in 2020. There is need for UNEPI and WHO to train health staff, intensity support supervisions, and hold review and feedback meeting with districts.
Background
Poliomyelitis is a disease caused by the wild poliovirus (WPV) [1], and it can cause lifelong paralysis or death. In 200 poliovirus infections, one will present with an irreversible paralytic disease, known as Acute Flaccid Paralysis (AFP) with, 5 to 10% of them will die when their breathing muscles become immobilized [2]. Polio mainly affects children under 5 years of age [3, 4]. Poliomyelitis has no cure but can be preventable through vaccination. Wild polioviruses are human enteroviruses with three individual and immunologically distinct serotypes 1, 2 and 3; serotypes 2 and 3 have been declared eradicated by WHO in September 2015 and October 2019, respectively [5]. In addition, Poliomyelitis caused by vaccine-derived poliovirus (VDPV) or vaccine-associated paralytic poliomyelitis (VAPP) are also targeted for eradication. VAPP occurs when the live attenuated poliovirus strain in the oral polio vaccine (OPV) changes in the intestines and causes development of symptoms of paralytic polio within the vaccine recipient or a very close contact, but does not spread to cause paralysis in other cases. VDPV rarely occurs when a strain of poliovirus in OPV changes and revert to a form that may be able to cause paralysis in humans and develop the capacity to spread from person to person [6].
The Poliovirus spreads from person to person through contact with faucal matter or droplets from cough or sneeze of an infected person [1, 7]. The Poliovirus enters through the mouth and multiplies in the pharynx and intestines of its human host and consequently replicates in the motor neurons of the anterior horn and brain stem, destroying cells and thus manifesting poliomyelitis. Before the onset of illness (which is usually after 7 to 21 days), the virus is present in the throat for 1 to 2 weeks but remains shaded in the stool for several weeks [8].
The Global Polio Eradication Initiative (GPEI) Polio Endgame Strategy 2019-2023 targets to eradicate the poliovirus worldwide by 2023. The initiative emphasised in goal 1 (Eradication) the following core strategies to interrupt transmission: maintaining AFP surveillance and Environmental surveillance (ES), and providing polio vaccines through supplementary immunization activities (SIA) [9]. A sensitive acute flaccid paralysis (AFP) surveillance system is central to the overall polio eradication initiative [9]. WHO recommends minimum standards for AFP surveillance in a nationwide, case-based syndromic manner with laboratory confirmation of poliovirus from stool specimens. AFP cases are identified, reported and investigated using both active and passive surveillance, and community-based detection methods [1].
All children less than 15 years of age presenting with sudden onset of floppy paralysis or muscle weakness affecting either one or two limbs; or any person of any age with paralytic illness if poliomyelitis is suspected by a clinician are categorised as AFP cases [10].
This assessment aims to describe Uganda’s AFP surveillance performance from 2015 to 2020 based on the Uganda’s ministry of health and WHO recommended epidemiological performance indicators [1] for AFP surveillance. The information generated from this analysis contributes to evidence which guides the implementation of AFP surveillance interventions toward global eradication of polio.
Methods
Study setting
Uganda is a tropical country located in eastern Africa. The projected population of Uganda was 37,084,566 in 2015; 37,084,566 in 2016; 37,673,800 in 2018; 38,866,300 in 2019 and 41,583,600 in 2020 with a growth rate of 3.3% (UBOS). As of 2020, Uganda had 135 districts all report their AFP surveillance data to the Ministry of Health.
Study design and data source
We conducted a retrospective descriptive quantitative study using AFP surveillance secondary data submitted to ministry of health and WHO, Uganda office by districts using case-based reporting from 2015 to 2020.
Uganda adopted the WHO recommended AFP surveillance performance indicator targets, which include: At least 90% of all expected AFP monthly reports received in time; Annualized Non- polio AFP (NPAFP) rate of at least 4 per 100,000 children under 15 years of age; 80% of reported AFP cases investigated within 48hrs At least 80% of cases whose Specimens are arriving at the lab ≤ 3days; At least 80% of cases whose specimens arrive at the lab in “Good condition”; At least 10% of cases whose Specimens NPENT was isolated; At least 80% of cases whose Specimens are collected within 14 days of onset of Paralysis; At least 80% of proportion of cases (6 months-15 years) with OPV3+ immunization status; and At least 80% of stool adequacy rate.
There are two key AFP surveillance performance indicators [10] namely . Non-polio AFP Rate of at least 4 per 100,000 children under 15 years of age and stool adequacy rate of at least 80%. Non-polio AFP rate is an indicator of surveillance sensitivity that reduces likelihood of missing WPV cases. Non-polio AFP rate is measured by getting number of non-polio AFP cases under the age of 15 years / population under 15 years of age X 100 000. Stool adequacy rate is percentage of AFP cases with two adequate stools collected at least 24 hours apart within 14 days after onset of paralysis and arriving at the laboratory in good condition (“Good condition” means that upon arrival within 72 hours: There is ice or a temperature indicator (showing < 8°C) in the container, the specimen volume is adequate (>8 grams) there is no evidence of leakage or desiccation (It is important to fill the case investigation and specimen tracking form).
Study variables
We obtained already downloaded and organized district level annual data from Ministry of health (MOH), Uganda. The data included the following performance variables , total cases investigated, true AFP cases, minimum expected no. of non-polio AFP cases, Non polio AFP rate, proportion of reported AFP cases investigated within 48hrs, proportion of cases whose
Specimens are arriving at the lab ≤ 3days, proportion of cases whose sspecimens are arriving at the lab in “Good condition”, proportion of cases whose specimens (Non-polio enterovirus (NPENT) was isolated, proportion of cases whose specimens are collected within 14 days of onset, proportion of cases (6 months-15 years) with OPV3+, stool adequacy rate, and surveillance index.
Data analysis
From district level data, some sub regional, and national level variables were generated by getting sums. For example, proportion of districts with non-polio AFP rate of at least 1 per 100,000, 2 per 100,000 and 4 per 100,000 children under 15 years of age; proportion of districts with OPV3 immunization status of at least 80%; proportion of districts with stool adequacy rate of at least 80%; and percentage of districts that reported at least a case in the various groups.
In 2015, there were 112 districts, and this number increased gradually to 135 districts. For place analysis, the population of the districts created later were added to their mother district and given the same surveillance performance achievement.
We calculated proportion of districts with non-polio AFP rate of at least 1 per 100000, 2 per 100000 and 4 per 100000, proportion of districts with oral polio vaccine dose ≥3 (OPV3+) immunization status of at least 80%, proportion of districts with stool adequacy rate of at least 80% and percentage of districts that reported at least a case in the various groups. The analyses were stratified by sub regions, national, and calendar year.
Comparisons across the two indicators, including non-polio AFP and stool adequacy rate were made to assess for any relationships therein using trend analysis in STATA/ SE 14. We used QGIS to illustrate differences of NPAFP and stool adequacy rate across districts, sub regions and nationally.
Results
Acute flaccid paralysis cases and oral polio vaccine coverage ≥3 doses, Uganda, 2015-2020
Between 2015 and 2020, the population of children under 15 years of age increased from 18,171,438 to 21,623,472. During the study period, a total of 3,605 AFP cases were reported and investigated throughout the Country. Of the investigated AFP cases, 3,475 (96%) were true AFP cases (Table 1). Majority of the true AFP cases (85%) had received the recommended ≥3doses of oral polio vaccine. Of the true AFP cases, none were classified as poliomyelitis. Four hundred forty five (13%) AFP cases were caused by non-polio enteroviruses (NPEV).
Table 1: Acute flaccid paralysis cases and oral polio vaccine coverage ≥3 doses, Uganda, 2015-2020
| Year | Under 15 population | AFP cases investigated | True AFP
cases |
Districts with cases of OPV3+ immunization status of at least 80%, n (%) | Average proportion of cases with OPV3+ Immunization status |
| 2015 | 18,171,438 | 600 | 570 | 82 (73) | 88% |
| 2016 | 18,171,438 | 713 | 674 | 85 (76) | 90% |
| 2017 | 19,590,376 | 610 | 590 | 59 (51) | 74% |
| 2018 | 19,590,376 | 628 | 606 | 85 (73) | 88% |
| 2019 | 20,210,476 | 595 | 580 | 86 (67) | 84% |
| 2020 | 21,623,472 | 459 | 455 | 103 (76) | 88% |
| Total | 117,357,575 | 3,605 | 3,475 | 500 (70) | 85% |
Non-polio acute flaccid paralysis rate as a surveillance indicator, Uganda, 2015-2020
The mean non-polio AFP rate generally declined from 3.14 per 100,000 in 2015 to 2.1 per100,000 in 2020 (Figure 1). The mean non-polio AFP rate in the study period was 3.0 per 100,000 population of children under 15 years of age. During the study period, year 2016 recorded the largest non-polio AFP target rate of 3.71 whereas in every year, less than 40% of the districts achieved the non-polio AFP target rate of at least 4 per 100,000 population of children under 15 years of age, majority of the districts recorded non-polio AFP target rate of at least 2 per 100,000 population of children under 15 years of age (Table 2).
Table 2: Non-polio acute flaccid paralysis rate and trend analysis of proportion of districts with non-polio acute flaccid paralysis rate of at least 4 per 100,000, in Uganda, 2015-2020
| Years | Non-polio AFP rate per 100,000 (Min-Max) | Districts with non-Polio AFP rate | Districts with no report of AFP | Trends analysis, Odds | |
| at least 4/100000, n (%) | at least 2/100000, n (%) | ||||
| 2015 | 3.14 (0.80-28) | 39 (35) | 72 (64) | 0 (0.0) | 1 |
| 2016 | 3.71 (0.0-15) | 40 (36) | 77 (69) | 1 (0.89) | 0.96 (0.54 -1.7) |
| 2017 | 3.01 (0.52-14) | 29 (25) | 81 (70) | 0 (0.0) | 1.57 (0.87-2.8) |
| 2018 | 3.09 (0.52-14) | 31 (27) | 85 (73) | 0 (0.0) | 1.46 (0.80 -2.7) |
| 2019 | 2.87 (0.36-17) | 49 (38) | 86 (67) | 0 (0.0) | 0.88 (0.49-1.6) |
| 2020 | 2.10 (0.0-20) | 27 (20) | 56 (41) | 3 (2.2) | 2.2 (1.1-4.1) |
| Total | 2.99 (0.37-18) | 4 (0.52) | |||
CI=Confidence Interval
In the study period, 4 districts did not report any AFP cases (silent district); most (3) of the silent districts were observed in the year 2020 (Table 2). There was an overall decline in proportion of districts with the targeted non-polio AFP rate of at least 4 per 100,000 between year 2015 (at 35%) and 2020 (at 20%). The proportion of districts with non-polio AFP rate of at least 4 per 100,000 significantly declined by 43% (OR=2.2; 95% CI: 1.1-4.1) between 2015 and 2020 (Table 2). Nationally, year 2020 recorded the least (20%) proportion of districts that met the minimum non-polio AFP target rate of at least 4 per 100,000 children under 15 years of age.
Similarly, year 2020 recorded the least (41%) proportion of districts that achieved non-polio AFP target rate of at least 2 per 100,000 children under 15 years of age (Table 2).
Distribution of Non-polio AFP rate per 100,000 by districts, Uganda, 2015-2020
Most districts did not generally attain the non-polio AFP target rate (4 per 100,000 children <15 years) (Figure 1).
Stool adequacy rate as a surveillance indicator, Uganda, 2015-2020
In Uganda, the stool adequacy rate has generally increased from 88% in 2015 to 91% in 2020 (Table 4). The mean stool adequacy rate in the study period was 88%. Throughout the study period, majority of the districts achieved the stool adequacy target rate of at least 80% (Table 4).
Table 4: Oral polio vaccine coverage ≥3 doses (OPV3+), stool adequacy rates and trend analysis of proportion of districts with stool adequacy rate of at least 80%, Uganda, 2015- 2020
| Year | Districts with cases of OPV3+
immunization status of at least 80%, n (%) |
Average proportion of cases with OPV3+ Immunization status | Districts with cases of stool adequacy rate of at least 80%, n (%) | Average Stool adequacy rate | Trends analysis, Odds ratio (CI) |
| 2015 | 82 (73) | 88% | 76 (68) | 88% | 1 |
| 2016 | 85 (76) | 90% | 69 (62) | 89% | 1.3 (0.76 -2.3) |
| 2017 | 59 (51) | 74% | 77 (66) | 82% | 1.1 (0.61-2.0) |
| 2018 | 85 (73) | 88% | 60 (52) | 88% | 2.0 (1.2 -3.4) |
| 2019 | 86 (67) | 84% | 88 (69) | 90% | 0.96 (0.56-1.7) |
| 2020 | 103 (76) | 88% | 108 (80) | 91% | 0.53 (0.30-0.94) |
| Total | 500 (70) | 85% | 478 (66) | 88% |
CI=Confidence Interval
There was an overall increase in proportion of districts that met the stool adequacy rate of at least 80% between 2015 and 2020. The proportion of districts with stool adequacy rate of at least 80% significantly increased by 15% (OR=0.53; 95% CI: 0.30-0.94) between 2015 and 2020 (Table 4). Nationally, 2018 recorded the least (52%) proportion of districts that met the minimum stool adequacy target rate of at least 80% (Table 4).
Distribution of stool adequacy rate by districts, Uganda, 2015-2020
Most districts had generally not attained the stool adequacy target rate. At district level, the map generally had a bigger number of districts with less than 80% stool adequacy rate in 2015 and reduced as every year passed by, which implied that stool adequacy rate was improving over time in several districts (Figure 2).
Discussion
This study aimed at describing the AFP surveillance performance in Uganda from 2015 to 2020, based on the two key recommended performance indicators for AFP surveillance i.e. non-polio AFP and stool adequacy rate. This current study showed that majority of the AFP cases investigated were true AFP cases, and yet majority of them had received three or more (OPV3+) doses of oral polio vaccine. This is similar to the study findings in Ethiopia [11], Kenya [12], and Iran [4]. Whereas polio vaccination coverage of at least 90% yields herd immunity, this assessment indicated that the OPV3+ coverage among AFP cases was lower. It is possible that the OPV3+ coverage stated in this study was underestimated, as this could be affected by recall bias.
Nationally, the non-polio AFP rate significantly declined between 2015 and 2020. This was contrary to many similar studies that showed increase in non-polio AFP rates over the period of assessment [12, 13]. In addition, the country also did not meet the target of 4 per 100,000 children under 15 years as adopted [10]. Significant decline in non-polio AFP rates over the assessment period, and non-attainment of the non-polio AFP target rates indicates that there was decreasing sensitivity of the AFP surveillance system with more likelihood of missing any ongoing transmission of either circulating VDPV or WPV. It is possible that districts are yet to understand this new AFP surveillance indicator of 4 per 100,000 children under 15 years, and thereafter intensifying efforts and resources towards meeting the target is critical. Most of the silent districts were recorded in 2020. Similarly, in 2020, the least proportion of districts met the non-polio AFP target rate of at least 4 per 100,000 children under 15 years of age. Furthermore, there was generally poor performance in meeting the non-polio AFP target rate in 2020 compared to other years. This could be attributed to the fact that COVID-19 interrupted health service delivery in the whole country [13, 14].
The national stool adequacy rate significantly increased in between 2015 and 2020, with mean stool adequacy rate in the study period being higher than the recommended target of 80%. This finding is in line with a study conducted in Ethiopia [11], some eastern and southern African countries [13], Liberia [15]. There were sub regional variations in terms of stool adequacy. This could be attributed to the good attitude and skill of the health facility staff or district surveillance focal persons. High stool adequacy rates indicate that two enough stool samples reached the laboratory in time in good condition within 72 hours. In this assessment, it likely that the surveillance system will not miss the virus in the stool.
Limitations
The dataset did not have data on variables such as sex, age, and AFP categorization. This did not allow explicit description of AFP surveillance. For example, we could not the proportion of <5 years fully vaccinated with OPV.
Conclusion
The majority of the true AFP cases had received three or more (OPV3+) doses of oral polio vaccine. Nationally, there was a significant decline in non-polio AFP rate, and significant increase in stool adequacy rate between 2015 and 2020. The non-polio AFP target rate of 4 per 100,000 children under 15 years was not met by the country, and yet the average stool adequacy target rate of 80% was met. The worst performance in AFP surveillance was recorded in 2020. There is need for ministry of health and WHO to train health staff, intensity support supervisions, and hold review and feedback meeting with districts.
Acknowledgments
Special thanks go to the WHO office in Uganda for being cooperative and supportive in availing cleaned AFP surveillance dataset.
References
- World Health O: Surveillance standards for vaccine-preventable diseases, 2nd ed. Geneva: World Health Organization; 2018.
- Fact sheets: Poliomyelitis [https://www.who.int/news-room/fact- sheets/detail/poliomyelitis]
- Lam RM, Tsang TH, Chan KY, Lau YL, Lim WL, Lam TH, Leung NK: Surveillance of acute flaccid paralysis in Hong Kong: 1997 to 2002. Hong Kong medical journal = Xianggang yi xue za zhi 2005, 11(3):164-173.
- DAVARPANAH MA, BAKHTIARI H, MEHRBANI D, KHADEM ALHOSSEINI F: A 12-YEARS SURVEILLANCE OF POLIOMYELITIS AND ACUTE FLACCID PARALYSIS IN FARS PROVINCE, SOUTHERN IRAN. IRANIAN RED CRESCENT MEDICAL JOURNAL (IRCMJ) 2008, 10(4):-.
- Dyer O: Polio: WHO declares type 3 poliovirus eradicated after 31 year campaign. BMJ 2019, 367:l6201.
- WHO: Vaccine-associated paralytic polio (VAPP) and vaccine-derived poliovirus (VDPV). In: Fact Sheet – February 2015.
- Global Immunization: What is Polio? [https://www.cdc.gov/polio/what-is- polio/index.htm#:~:text=Poliovirus%20only%20infects%20people.,infected%20person% 20(less%20common).]
- CDC: Poliomyelitis. In: edn. Edited by Concepcion F. Estivariz MRL-G, PhD, MPH; and Tom Shimabukuro, MD, MPH, MBA: US Centers for Disease Control and Prevention; 2020: 297-310.
- World Health Organization: Polio Endgame Strategy 2019-2023: Eradication, interration, certification and containment. In: WHO/Polio/1904. Geneva;
- UNEPI: IMMUNIZATION IN PRACTICE UGANDA. In: A Reference Manual for Pre & In-service Health Workers. Uganda National Expanded Programme on Immunization, Kampala: Ministry of Health; 2016.
- Tegegne AA, Fiona B, Shebeshi ME, Hailemariam FT, Aregay AK, Beyene B, Asemahgne EW, Woyessa DJ, Woyessa AB: Analysis of acute flaccid paralysis surveillance in Ethiopia, 2005-2015: progress and challenges. Pan Afr Med J 2017, 27(Suppl 2):10-10.
- Tesfaye B, Sowe A, Kisangau N, Ogange J, Ntoburi S, Nekar I, Muitherero C, Camara Y, Gathenji C, Langat D et al: An epidemiological analysis of Acute Flaccid Paralysis (AFP) surveillance in Kenya, 2016 to 2018. BMC Infectious Diseases 2020, 20(1):611.
- Manyanga D, Byabamazima C, Masvikeni B, Daniel F: Assessment of acute flaccid paralysis surveillance performance in East and Southern African countries 2012 – 2019. Pan Afr Med J 2020, 36:71.
- Abila DB, Ainembabazi P, Wabinga H: COVID-19 pandemic and the widening gap to access cancer services in Uganda. Pan Afr Med J 2020, 35(Suppl 2):140.
- Clarke A, Blidi N, Dahn B, Agbo C, Tuopileyi R, Rude MJ, Williams GS, Seid M, Gasasira A, Wambai Z et al: Strengthening acute flaccid paralysis surveillance post Ebola virus disease outbreak 2015 – 2017: the Liberia experience. Pan Afr Med J 2019, 33(Suppl 2):2.
Read and download full article bellow;
Reference this page as below
Bob O. Amodan1, 2*, Annet Kisakye3, Daniel Kadobera1, Alfred Driwale2,Alex R. Ario1, 2. Trends of key surveillance performance indicators of acute flaccid paralysis: A descriptive analysis of the surveillance system, Uganda, 2015-2020. Kampala, Uganda National Institute of Public Health. 2021 June 30th. Available from:https://uniph.go.ug/trends-of-key-surveillance-performance-indicators-of-acute-flaccid-paralysis-a-descriptive-analysis-of-the-surveillance-system-uganda-2015-2020.

