COVID-19 cluster within health facilities in Abim District, October 2020
Quarterly Epidemiological Bulletin: Volume 6 / Issue 2/Article No. 5 April -June, 2021
Authors: Immaculate Akusekera1*, Bob Amodan1, Peter Oumo1, Benon Kwesiga1, Lilian Bulage 1, Ario Alex1
Affiliations: 1Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda
*Corresponding author: iakusekera@musph.ac.ug, Tel: 0788109081
Summary
Coronavirus Disease (COVID-19) has been an ongoing epidemic in Uganda since March 2020. As of 8 October, 2020, more than 9,500 cases had been confirmed, with nearly 350 (4%) among health care workers (HCWs). During September 2020, a cluster of COVID-19 cases was identified among health care workers and community members in Abim District, northern Uganda. We investigated to describe the transmission pattern in the cluster and recommend evidence-based prevention and control measures.
We defined a case as a laboratory-confirmed SARS-CoV-2 infection in a resident of Abim district during September and October 2020. We identified cases from the hospital records and interviewed case-patients on contact and exposure histories.
Abim District in Northern Uganda experienced a COVID-19 cluster of 25 patients with COVID-19. A 35-year-old expectant female HCW was the index case. She reportedly had no travel history and had no known contact with persons with suspected or confirmed COVID-19. She interacted widely without protective gear with persons at Abim Hospital, Morulem health centre (HC) III, and Aremo village for at least 18 days (September 4-22) while symptomatic. She was hospitalised in Abim hospital for this illness but not isolated, testing was not conducted until a week after she presented with symptoms. Results took 11 days to return. Despite her pending COVID-19 test results, the patient was released from the hospital.
Most (76%) of the patients in the cluster were HCWs. The most affected facilities were: Morulem HC III (31/100 HCWs infected) where the index case spent two days and Abim hospital (4/100 HCWs infected) where the index case-patient spent seven days while hospitalised. An additional case-patient existed at Morulem HC III around the same time that may have also contributed to the high attack rate there.
We recommended strict adherence to guidelines around isolation of patients with COVID-19 related symptoms in Abim hospital, self-isolation of the symptomatic individuals and a training on suspicion and effective isolation of COVID-19 cases for HCWs in Abim District. The Ministry of Health should also decrease the turnaround time for COVID-19 samples to avoid instances of releasing positive case-patients.
Introduction
Coronavirus Disease (COVID-19) is a viral respiratory illness caused by SARS-CoV-2. It causes a range of human respiratory tract infections varying from mild cold to severe respiratory distress syndrome and even death [1].The virus is spread primarily via respiratory droplets during close face-to-face contact [2, 3]. Infection can be spread by asymptomatic, pre-symptomatic, and symptomatic carriers and the medium virus shedding time is around 19 days [4]. The average time from exposure to symptom onset is 5 days, and 98% of people who develop symptoms do so within 12 days [4]. Spread of COVID-19 from patients to healthcare workers (HCW) and between healthcare workers has also been reported [4].
COVID-19 has been an ongoing epidemic in Uganda since March 2020. As of 8 October, 2020, more than 9,500 cases had been confirmed, with nearly 350 (4%) among HCWs[5]. Abim District in Northern Uganda had registered only two cases of COVID-19 since the beginning of the pandemic. On 11 September 2020, Abim hospital medical staff suspected COVID-19 in one of the patients admitted in the hospital. Samples were picked from the patient on 11 September, but did not return positive until 22 September 2020. Following the positive test confirmation, contacts were listed and samples taken for COVID-19 testing. Of these, 25 persons tested COVID-19-positive, of whom 19 were HCW. It was not clear what had caused the cluster and what the missed opportunities were for the prevention of COVID-19 spread among HCW. We described the cluster, its transmission dynamics, and provide evidence-based recommendations to reduce future hospital related COVID-19 clusters.
Methods
Study setting: The cluster occurred in Abim District, northern Uganda which had a projected 2020 population of approximately 153,000 persons [6]. The district has one hospital and 17 lower-level health facilities. The hospital had 134 staff, while the lower health center IIs and IIIs have an average of seven and 11 staff each, respectively.
Case definition and finding: We defined a confirmed case as a positive PCR for SARS-CoV-2 in a resident of Abim District from 4 September to 5 October, 2020. We identified the cases using the district health records and visited Abim Hospital COVID-19 isolation unit to seek verbal consent from case-patients for the phone interviews.
Investigation: We conducted phone interviews with all case-patients in the isolation using a standardized COVID-19 questionnaire modified from the national general case and HCW investigation forms. We asked about contact with suspected or confirmed COVID-19 cases, dates of contact with these persons, presence of symptoms, dates of symptom onset for the symptomatic, wearing appropriate personal protective equipment (PPE) while handling patients (for HCW), PPE while in the community (for HCW and community members), practices around hand hygiene and social distancing and visits to any social gatherings in the last month before symptom onset or positive test result (for asymptomatic persons).
Data analysis: We described the case-patients by person, place, and time. We constructed transmission chains and used epidemic curves by date of symptom onset to describe the characteristics of the cluster over the investigation period. We calculated attack rates by health facility and by cadre of HCW (for HCW).
Ethical considerations: This investigation was conducted as part of the Ministry of Health (MoH) efforts to control the COVID19 pandemic in Uganda. The MoH of Uganda through the office of the Director General Health Services gave the directive and approval to conduct this investigation. Additionally, the office of the Associate Director for Science, Centers for Disease Control and Prevention, Uganda, determined that this investigation was not human subjects’ research because the primary purpose was to identify, characterize, and control disease in response to a perceived immediate public health threat. We sought permission to interview the patients from the District health office. We obtained verbal informed consent from case-persons before the interviews.
Index case and sequence of events leading to index case identification
The index case-patient was a 35-year-old female HCW at Koya HC II, one of the lower-level health facilities in Abim District.
She reportedly had no travel history and had no known contact with persons with suspected or confirmed COVID-19.
On 4 September, she presented to Koya HCII with a dry cough and chest pain. She was 8.5 months pregnant at the time of her onset. She was managed as an outpatient for the cough and treated with antibiotics, but not tested for COVID-19. However, she developed a pneumonia and on 9 September, she was referred to Abim Hospital where she was admitted to the maternity ward. While at the hospital, she was continued on antibiotic treatment despite worsening of her illness.
On 11 September, she developed difficulty in breathing, at which point staff suspected COVID- 19 and took a sample for testing. Despite not having results, she had improved by 16 September and was discharged, after which she returned to her residence at Koya for two days.
On 18 September, she travelled to Aremo village with in Abim District to stay with relatives while waiting to deliver her baby. While there, she interacted socially with the community including fellow HCWs while visiting their homes.
On 20 September, she delivered a healthy infant at Morulem HC III (within Aremo village). On 22 September, her test results were returned, confirming her infection with SARS CoV-2. She was isolated the same day at the Abim Hospital; contacts were identified and also tested for COVID-19.
Table 1: Characteristics of the COVID-19 case-patients identified in Abim District, Uganda, October 2020
| Characteristic (N=25) |
Frequency |
Percent |
| Sex
Female |
19 |
76 |
| Male | 6 | 24 |
| Occupation
Healthcare worker |
19 |
76 |
| Farmer | 3 | 12 |
| Teacher | 2 | 8 |
| Student | 1 | 4 |
| Facility with affected staff
Abim Hospital |
12 |
63 |
| Morulem HCIII | 5 | 26 |
| Karenga HCIV | 1 | 5 |
| Koya HCII | 1 | 5 |
| Health care worker cadres affected
Midwife |
8 |
42 |
| Nurse | 8 | 42 |
| Records Assistant | 2 | 11 |
| Hospital admin | 1 | 5 |
| Symptomatic | 17 | 68 |
| Contact with suspected/confirmed case-patient | 19 | 76 |
In total, 25 case-patients (including the index case-patient and those who were contacts to the index case-patient) were identified in this cluster.
Seventeen (68%) of these were symptomatic,19 (76%) of them were HCWs.
Mean age was 34 years (range, 13-56 years) and 19 (76%) were female. Twelve (52%) HCWs had direct contact with the index case-patient. Sixteen (84%) of the 19 HCWs were either nurses or midwives (Table 1).
Table 2: Attack rates of the COVID-19 infection among HCWs, Abim District, Uganda, October 2020
| Risk group(N=19) | Case(n) | Estimated population at risk | Attack rate/100 |
| Facility | |||
| Morulem HC III | 5 | 16 | 31 |
| Koya HC II | 1 | 5 | 20 |
| Abim hospital | 12 | 270 | 4 |
| Karenga HC * | 1 | ||
| Nurses
Morulem HC III |
2 |
7 |
29 |
| Abim hospital | 5 | 119 | 7 |
| Karenga * | 1 | ||
| Midwives
Morulem HC III |
2 |
2 |
100 |
| Koya HC II | 1 | 1 | 100 |
| Abim hospital | 5 | 32 | 16 |
| Abim Hospital Administrator | 1 | 1 | 100 |
| Abim Records assistant | 1 | 2 | 50 |
| Morulem HC III HIA | 1 | 1 | 100 |
*One of the HCW (from Karenga Health facility) was infected while visiting his family in Aremo village and therefore his facility and cadre AR are not calculated since it was not a work-related exposure.
HIA: Health information assistant
Morulem HC III was the most affected health facility with an Attack rate 31/100 while midwives were the most affected cadre in Morulem HC III with an AR of 100%
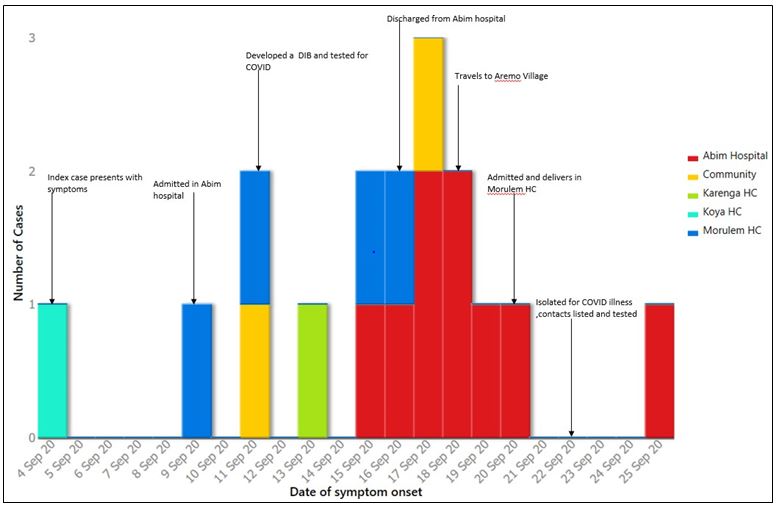
Figure 1: Distribution of the COVID-19 cases by date of symptom onset in Abim District Uganda, October 2020.
Among 17 (68%) who were symptomatic, onsets ranged from 4-25 September. The first case-patient after the index case had onset on 9 September (Figure 1). This patient was a HCW at Morulem HC III, and could have contributed to the infections at that facility. The epidemic curve demonstrated that the index case-patient could not have been the direct source of the infections before September 20 at Morulem HC III.
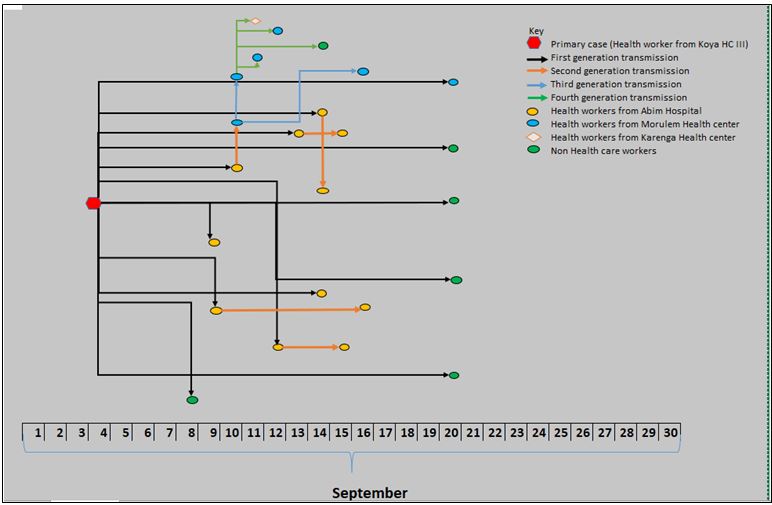
The SARS-CoV-2 infection transmissions in Abim hospital (where she spent seven days) were primarily or secondarily linked to the index case-patient. However, the index case was primarily linked to only one case patient in Morulem HC III (where she later delivered) her baby (Figure 2).
Discussion
Twenty-three (92%) of the cases, in the cluster of 25 SARS-CoV-2 infections in Abim District, Uganda during September, 2020 were epidemiologically linked to one infected HCW. The HCW had no known history of contact with a suspected or confirmed COVID-19 patient. She interacted widely without protective gear with persons at Abim Hospital, Morulem HC III, and Aremo village for at least 18 days (September 4-22) while symptomatic. While ill, she was hospitalised in the maternity ward in Abim hospital. She was therefore not isolated. Testing was not conducted until a week after she presented with symptoms and results took 11 days to return. Despite her pending COVID-19 test results, the patient was released from the hospital. None of the guidelines in and around isolation of the patient and health care worker interaction with communities while treating COVID-19 patients was adhered to.
Our findings established that the attack rate among the HCWs was 4/100 persons, the affected HCWs were from Abim hospital where the index case-patient spent seven days, Morulem HC III where she spent two days, Koya HC II where the case patient worked and Karenga HC whose case patient had visited His family in Aremo village where Morulem HC III is located. Our epidemiologic assessment demonstrated that the Morulem HC III was most affected and that midwives were the most affected cadre in Morulem HC III. We also demonstrated that there was no epidemiological evidence of transmission from the index case to cases that occurred 9 and 11 September in Morulem health facility.
Morulem HC III had its first case (GP), who reportedly interacted with staff from another health facility (Karenga) during the time they had lost a COVID-19 patient and had active cases. He reported no contact with the index case and no cases were linked to Him in this cluster. We also established one of the midwives in Abim hospital interacted with staff from Morulem HC III after treating the index case-patient during her stay on admission in Abim hospital. This interaction of the midwife probably resulted in spread and subsequent identification of cases in the facility (Morulem HC III) before being identified in Abim where the exposure initially happened. The index case therefore was not the sole source of exposure for all the cases in Morulem HC III and probably this explains the observed attack rate in and around Morulem HC III.
The community members affected in this cluster were mostly relatives to the health care workers, these likely contracted the infection during their social interaction with the infected HCWs. Studies elsewhere have evidenced possibilities of non-nosocomial infection among HCWs. In fact some highlight the possibility of them occurring more often than the work‐related acquisitions of COVID-19 [7].
The care taking staff in Abim hospital took almost four days before suspecting COVID-19. During this period, no extra precautional measures were taken while handling the index patient in the health facilities. Studies elsewhere have observed this kind of behaviour among HCWs, this situation may lead to a lack of recognition of the infection while patients are highly contagious [8], resulting in repeated opportunities for infection of unsuspecting HCW. In this investigation, we observed a propagated infection among the midwives since the initial exposure to the index case occurred in maternity ward and the staff reportedly used ordinally cloth masks while handling their patients. This observation was also similar to one in a prospective cohort study of nearly 100,000 HCW and more than 2 million community individuals in the US and the UK showed that frontline healthcare workers had 11.6 times higher risk of COVID-19 disease [9]. The non-medical staff was probably infected due to the fact that these non-front liners are rarely trained on infection control and are therefore less concerned with personal protective equipment use.
The turnaround time for the results was almost ten days which led to the release of the suspected case-patient before her results were confirmed. This then created an opportunity for the index patient to interact and spread the infection wider in the Abim community and other health facilities. At the time of the outbreak, samples from the district hospitals were picked by regional vans and delivered to regional referral hospitals. These would then be transported to the testing laboratories by through the hub system. The testing would take an average 24 hours and the test results communicated on wats up and email to the District health officers. This whole process would often take a week or longer, exceeding the time in which the results would be practically useful. However, a lot has changed since then, health facilities are able to screen patients for the SARS-Cov infection using Rapid diagnostic tests, private laboratories have been authorised to test for the Covid infection, and the government has procured testing machines that can produce results within a shorter time. All these efforts are geared towards reducing the time taken between sample collection and receipt of the test results.
Strengths and Limitations
The transmission tree was constructed based on history taking of contact with a suspected or confirmed case and also recall of the dates of contact. These might have been inaccurate due to the inability of the participants to recall the exact dates of contact and dates of symptom on set.
The symptoms of COVID-19 are very similar to the ordinally flu symptoms and therefore contact history and symptom onset date in this investigation might have been misrepresented or interpreted. Despite the limitations, the study highlights important behaviours of HCWs that need to be considered while managing COVID-19 infections in the facilities.
Conclusion
This COVID-19 cluster in Abim district started with one HCW who was not suspected early and therefore was not effectively isolated. Her COVID-19 test results took long and while waiting for the test results, she interacted with HCWs and community members. During the two weeks of waiting, she was not isolated, was symptomatic and infectious.
We recommend a training on suspicion and effective isolation of COVID-19 cases for HCWs in Abim District. We additionally recommend strict adherence to guidelines around isolation of suspected cases and HCW managing suspected cases. Ministry of Health should consider decreasing the turnaround time for COVID-19 samples.
Acknowledgements
We acknowledge the support of the Uganda Public Health fellowship programme and the Uganda US CDC for funding the investigation, Ministry of Health, Abim Hospital staff, and the entire District health team for supporting us with all the data we needed to accomplish the investigation.
References
- Wiersinga, J., et al., Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. Jama, 2020. 324(8): p. 782-793.
- Guo, R., et al., The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Mil Med Res, 2020. 7(1): p. 11.
- Raoult, , et al., Coronavirus infections: Epidemiological, clinical and immunological features and hypotheses. Cell stress, 2020. 4(4): p. 66.
- Wang, , et al., Nosocomial outbreak of COVID-19 pneumonia in Wuhan, China. Eur Respir J, 2020. 55(6).
- Ministry of health
- UBOS, Buikwe District Population Projection 2015-2020. 2015: Kampala,
- Muhi, S., L.B. Irving, and K.L. Buising, COVID‐19 in Australian health care workers: early experience of the Royal Melbourne Hospital emphasises the importance of community The Medical Journal of Australia, 2020. 213(1): p. 44-44. e1.
- Chang, , et al., Protecting health-care workers from subclinical coronavirus infection.
Lancet Respir Med, 2020. 8(3): p. e13.
- Nguyen, L.H., et al., Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health, 2020. 5(9): p. e475-e483.
Read and download the full article below;
Reference this Article as Below
Immaculate Akusekera1*, Bob Amodan1, Peter Oumo1, Benon Kwesiga1, Lilian Bulage1, Ario Alex1. COVID-19 cluster within health facilities in Abim District, October 2020, Kampala, Uganda National Institute of Public Health. 2021 June 30th . Available from: :https://uniph.go.ug/covid-19-cluster-within-health-facilities-in-abim-district-october-2020.

