The magic bullet: Using Interpersonal Communication to Increase Consistent Bed Net Use in Uganda: Policy brief
Authors: Alex Ndyabakira*, Daniel Emong, Doreen Gonahasa; Affiliation: Uganda National Institute of Public Health; Corresponding Author*: Email: andyabakira@musph.ac.ug, Tel: +256-774380914
Key Messages
- Uganda has the 3rd highest malaria burden globally and contributes 3% of total malaria cases in the world.
- 59% of people consistently use bed nets compared to the Ministry of Health target of 90%.
- Currently, Uganda utilizes mass media which reaches only 52% of Ugandans with messages of utilization of bed nets.
- Using community-led interpersonal communication could potentially increase the proportion of people reached with messages of utilization of bed nets from 52% to 100% and consequently increase bed net use to 90%.
Problem Statement
In 2019 alone, Uganda registered about twelve million cases of malaria thirteen thousand (13,000) of which resulted in deaths [1]. Furthermore, 3 out of 10 pregnancies were exposed to malaria infection. The World Health Organization (WHO) estimates that the use of long-lasting insecticidal nets (LLINs) alone can prevent up to 69% of malaria cases. Uganda has a target of at least 90% of the target population consistently using LLINs by 2025. The Ministry of Health (MoH) conducted mass LLIN use campaigns in 2009, 2013, 2017 [2] and 2020.
Evidence shows that despite these efforts, less than 8 out of 10 people own a LLIN. Out of these, only 6 out of 10 use LLIN, a figure lower than the national target of 9 out of 10 people using LLINs daily. As of 2019, bed net usage stood at 59% compared to the MoH target of 90% [2-4].
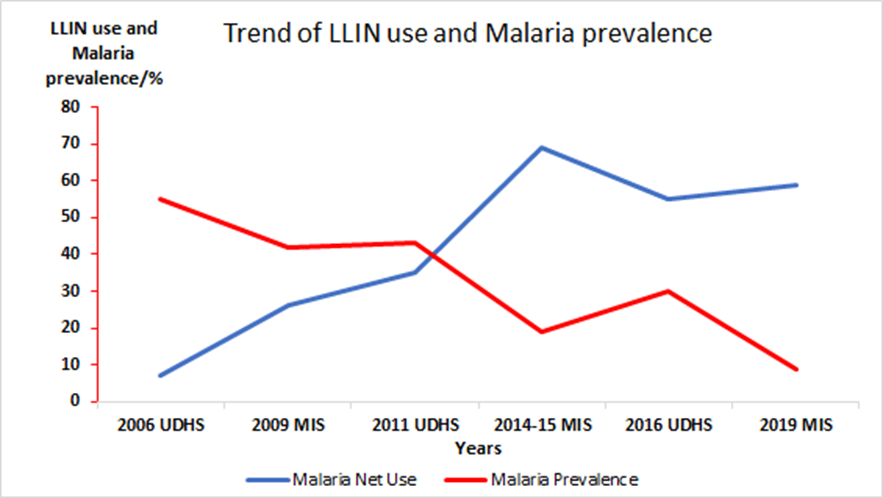
Figure 1 shows trends of LLIN use over a 13-year period and the relationship with prevalence of malaria. In fact, 41% of the population remains at risk of acquiring malaria at any point in time as result of the non-use of LLINs. This may result in 281/1,000 cases of malaria and 9 in 100,000 deaths per year due to malaria.
Messaging for LLIN use is conventionally done through broadcasting over mass media (Radio, TV, flyers/posters, and billboards) which are able to reach many people at once, and health facility-based interpersonal communication (IPC), also known as one on one communication where health workers are able to speak to people that seek healthcare. This has resulted in 59% of the intended national population using LLINs against[2] the MoH national target of 90%[5].
The possible explanation for this gap is that the mass media approach is not accessible by all at-risk populations. For instance, as of 2019, 84 % of the population had access to radio while only 34% could access television and of the 74% population who had access to phones, only 17% could access the internet. At present, 16% of the population reached with messages through interpersonal communication use bed nets[2].
Those who heard messages through interpersonal communication believe that one-on-one communication easily influenced them to use bed nets because it gave an opportunity to seek clarity on the use of bed nets and often eliminated the issue of language barrier.
Community-led interpersonal communication involves direct communication between one person and another; this form of communication has been shown to overcome challenges associated with use of mass media because it allows each person participating in the discussion to seek clarity on any information they have not understood.
Some studies have shown a notable increase in LLIN use following messaging through IPC (1,2)
Policy Options
- Status quo
What: Messaging for Communication of LLIN mosquito net use happens through mass media and by health care workers at health facilities for visiting patients
How: National Malaria Control Division (NMCD) LLINs distribution campaign is conducted simultaneously with messaging for uptake and use via mass media such as TVs, Radio, Mobile vans, newspapers. This is augmented by health workers who conduct health education to patients when they visit the facility to seek health care.
Problem: Mass media is not accessible by all at-risk populations especially the rural and low-income earners who constitute the majority of the at-risk population. In addition, there is a language barrier, limited opportunity to seek clarity, unfavorable time of broadcast, and exclusion of people who may not visit the health facilities to seek care. Despite mass media interventions, 59% of the population only (about 6 out 10 people) sleep under mosquito nets.
Feasibility: High: This strategy requires a lot of funds, transport, and human resources. Its implementation is dependent on donor funding with budgetary constraints.
- Community-led interpersonal communication
What: Conduct population-wide community-led interpersonal communication to reach 100% of the population with beneficial messages that will influence consistent and daily LLIN use, care and regular repair.
Why: Increased population reach with impactful and influential messages requires community-led interpersonal communication. In our model, Village Health Teams (VHTs) in addition to community champion mothers, influential shop attendants, and opinion leaders trained in interpersonal communication would increase LLINs use. For example, in the study conducted in Nakasongola district, Uganda[6], the proportion of under-five children who used LLIN the previous night increased from 51% to 74.7% and from 24% to 78% among pregnant women[6]
Feasibility: High: This strategy builds on the government’s efforts to eliminate malaria by the year 2030. The IPC model allows one on one direct engagement between the interpersonal communicator and the targeted individuals and has high influence to cause the desired change. It will require an operational legal framework, training, and placement of more trained community interpersonal communicators.
Economic Evaluation Results
We conducted an economic evaluation of two policy options to ascertain which is the most cost-effective strategy to reach the population with malaria messages in Uganda. The results are as shown in the table below.
| Status Quo
|
Reinforcing community-led interpersonal communication for increased population reach and influence LLIN use, care, and repair | |
| Expected no of target population reached | Varies depending on media used; difficult to assess | Population-wide (100%) |
| Number of Malaria cases | 2,377,000.0 | 2,242,000 |
| Expected no. of Malaria Cases averted per year | 135,000 | |
| Expected total cost ($) | 2,472,019.2 | 1,082,474.6 |
| Incremental Costs | (1,389,544.6) | |
| Cost/life saved ($) | 10.3 | |
| Political feasibility | High | High |
| Operational feasibility | High | High |
The results indicate that the communication intervention strategy based on simulated health impact to improve the use of LLIN use is community-led interpersonal communication. This strategy reduces the proportion of new malaria infections by 6% for a period of 1 year. On the other hand, this intervention has a lower cost compared to the status quo. Overall, community-led interpersonal communication is very cost-effective as it costs $10.3 to avert an additional case of Malaria.
Recommendations
We, therefore, recommend reinforcing community-led interpersonal communication as the most impactful, cost-effective, and feasible option to increase consistent bed net use in Uganda. We recommend substitution of the current messaging via mass media with community-led interpersonal communication strategy as a key medium for malaria messaging for the Ministry of Health of Uganda. This should involve using Village Health Teams (VHTs) in addition to community champion mothers, influential shop attendants, and opinion leaders to ensure increased population reach with impactful and influential messages through interpersonal communication.
Acknowledgement
We thank the Uganda Public Health Fellowship Program, particularly the team that investigated an upsurge in malaria cases in Nwoya District in 2018, which revealed that applying integrated malaria prevention methods was associated with reduced malaria transmission and illness, upon which this policy brief is based. We also appreciate the MoH National Malaria Control Division for continued efforts towards reducing malaria incidence in the country, and the entire team that worked towards formulating this policy brief.
References
- Organization, W.H., World malaria report: 2020. 2020, World Health Organization: Geneva.
- UBOS, U.B.o.S., Uganda Malaria indicator survey 2018-2019. 2020: Kampala Uganda and Rockville, Maryland, USA.
- Staedke, S.G., et al., Effect of long-lasting insecticidal nets with and without piperonyl butoxide on malaria indicators in Uganda (LLINEUP): a pragmatic, cluster-randomised trial embedded in a national LLIN distribution campaign. The Lancet, 2020. 395(10232): p. 1292-1303.
- Gonahasa, S., et al., LLIN Evaluation in Uganda Project (LLINEUP): factors associated with ownership and use of long-lasting insecticidal nets in Uganda: a cross-sectional survey of 48 districts. Malaria journal, 2018. 17(1): p. 421.
- MOH, CONTINUOUS LONG LASTING INSECTICIDAL NETS (LLIN) ACCESS AND USE GUIDELINES N.M.C. Division, Editor. 2019, Ministry of Health: Kampala. p. 1-10.
- Mugisa, M. and A. Muzoora, Behavioral change communication strategy vital in malaria prevention interventions in rural communities: Nakasongola district, Uganda. The Pan African Medical Journal, 2012. 13(Suppl 1).
Reference this page as;
Alex Ndyabakira*, Daniel Emong, Doreen Gonahasa. The magic bullet: Using Interpersonal Communication to Increase Consistent Bed Net Use in Uganda: Policy brief. Kampala, Uganda, Uganda National Institute of Public Health, 2021 December 30th. Available from:https://uniph.go.ug/the-magic-bullet-using-interpersonal-communication-to-increase-consistent-bed-net-use-in-uganda-policy-brief.


Comments are closed.