Re-Classifying Anthrax as a Public Good Disease: A Policy Brief
Authors: Geoffrey Amanya*, Richard Migisha, Esther Kisakye; Affiliation: Uganda National Institute of Public Health, Ministry of Health; Corresponding Author*: Email: gamanya@musph.ac.ug, Tel: +256777100032
Key Messages
- Anthrax is an acute infection with a very high case fatality rate ranging from 25-80%.
- In 2018 alone, 3 districts accounted for a total of 186 human cases and 721 animal deaths.
- Government loses an average of 140 USD in the management of one anthrax case.
- WHO recommends 80% anthrax vaccination for effective control; however, less than 6% of animals are vaccinated in Uganda.
- Re-classification of anthrax from private to public can eliminate anthrax.
Problem Statement
Anthrax is a zoonotic disease, caused by a bacteria transmitted to humans through handling or eating meat from infected animal carcasses or by breathing in spores1. Anthrax among livestock presents as a severe infection with a high death rate. About 3-8 people with severe infection die1,2. Uganda has had continuous and recurring outbreaks of anthrax since 1968, with an average of 3 to 5 investigated outbreaks per-year3. In 2018 alone, Kween, Kiruhura and Arua districts accounted for a total of 186 human cases and 721 animal deaths. Due to increasing cases, the government loses approximately $140 per person in management of complex anthrax cases in humans. Limited vaccination coverage is one of the most important contributing factors to re-occurrence of anthrax outbreaks in Uganda. Currently the vaccination coverage for anthrax in Uganda is estimated at 0-6%, Falling short of the WHO recommendation for 80% coverage4.
Uganda is vulnerable to zoonotic diseases due to its unique biological diversity, and population increase which is associated with encroachment of game parks and reserves, which facilitates close contact between humans and animals (domestic and wild) across the country. The population’s heavy engagement in agriculture indicates increased interaction between livestock and humans, which is a ground for transmission of anthrax. Moreover, over 80% of Uganda’s population is engaged in agriculture with 58% of these individuals involved in livestock farming. Uganda has an estimated 14.3 million cattle, 15.7 million goats, 4.3 million sheep, and 4 million pigs, which generates a lot of income to the farmers, and revenue to the government – the livestock sector contributes to 1.54% to Uganda’s Gross Domestic Product.
Currently, anthrax is classified as a “private good disease” which means that the management and control of anthrax in Uganda is done by farmers. Unlike other diseases like foot and mouth disease, Contagious bovine pleuropneumonia (CBPP) and Rabies which are state-controlled diseases. Reclassifying anthrax as a public good disease will ensure state control and management of anthrax, thus may reduce the frequency of outbreaks reported among animals and humans across the country. Therefore, the main objective of this policy brief is to highlight the benefits of reclassifying anthrax as a public good disease, which is critical to the prevention and control of future anthrax outbreaks in Uganda.
Policy Options
Policy Option 1: [Maintain status-quo]
Under this policy, Currently Anthrax is classified as a “private disease” this means that farmers are responsible for treatment and disposal of animals affected by anthrax, Farmers can go ahead treat the animals, and Vaccinate but not through a MAAIF or MOH affiliated program.
Policy Option 2: [Anthrax to be reclassified as a public good disease:] – (100% vaccination)
Under this policy, Government to fund anthrax vaccination and its administration / community sensitization, Procurement and delivery of vaccines and carcass disinfectants to households, administration of vaccines to livestock and Post exposure prophylaxis
Policy Option 3: [Compulsory vaccination of 80%
Under this policy, Government to fund 80% of the anthrax vaccination, its administration / community sensitization, procurement and delivery of vaccines and carcass disinfectants to households and Post exposure prophylaxis
Methods
We used a decision analysis approach. We used country reports, and Uganda-specific governmental reports to obtain data to inform our assumptions, where we couldn’t find enough literature or country level data, where no documented data were available, we used informed guesses. We constructed a decision tree to compare different options for reclassifying Anthrax as a public good disease. We calculated incremental cost effectiveness ratios (ICERs) expressed as US$ per additional in the low and high transmission scenarios
We conducted sensitivity analysis for the Animals if infected.
Results
Cost-effectiveness analysis for the three policy options, Uganda 2021
| S/n | Outcome | Policy Option 1
Status-Quo |
Policy Option 2
100% Vaccination |
Policy Option 3
80% Vaccination |
| 1 | Animal Cases | 22,460,483 | 47,101 | 581,681 |
| 2 | Animal Deaths | 2,246,048 | 4,4710 | 9,420 |
| 3 | Human Infections | 4,492,097 | 9,420 | 116,336 |
| 4 | Increment effect (Human Deaths) | 49,413 | 104 | 1,280 |
| 5 | Total costs for each intervention (US$) | – | 23,299,236 | 21,429,977 |
| 6 | ICER cost/case averted* | – | 473 | 445 |
| 7 | Political Feasibility | Feasible | Feasible | Feasible |
| 8 | Operational Feasibility | High | Moderate | High |
*ICER: Incremental cost-effectiveness ratio, ICER = (Costs 2 -Costs 1)/(Effectiveness2-Effectiveness1).
At a prevalence of 0.13% for Anthrax infection among the livestock, a total of 22,460,483 for Option 1, 47,101 for Option 2 and 581,681 for Option 3 infected animals would be identified in one Horizon ,through this program we would expect 2,246,048 infected animals die from Anthrax to be to be for Option 1,4,4710 for Option 2 and 9,420 for Option 3. A total of 4,492,097 infected Human Infections would be identified for Option 1, 9,420 for Option 2 and 116,336 for Option 3. However, implementation costs for these interventions would cost Option 2 ($22.3 million USD) an ICER of $473 per case averted, for Option 3 and an ICER of $445 per case averted ($21.4 million USD) for Option 3
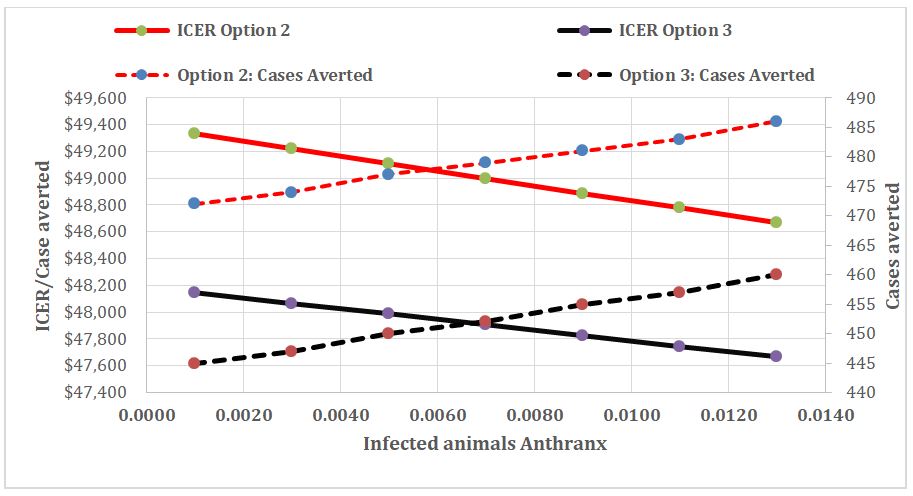
Figure 1; Showing Sensitivity – Variation in ICER by infection prevalence
Anthrax Infection prevalence had a major impact on the ICER, at high prevalence of animals infected Option 3 is still cost effective, i.e. the ICER/cases averted is lower than when compared to Option 2.
Conclusion
While compared to Option 1, status quo Both vaccination Options 2 (%100 vaccination) and Option 3(80% vaccination), indicate better alternatives to control of Anthrax from animals to humans, over a ten-year period. However, implementation costs for these interventions would cost Option 2 ($22.3 million USD) an ICER of $473 per case averted, for Option 3 and an ICER of $445 per case averted ($21.4 million USD) for Option 3, making Option3 Cheaper this is also reflected in sensitivity figure above for High and Low transmission scenario
Recommendation
Overall the 80% vaccination of all animals is the most effective approach to eliminating Anthrax.
Acknowledgments
We appreciate the CDC- Bloomberg Data for Health Initiative for funding and supporting the Policy development. We also appreciate the Ministry of Agricultural Animals and Fisheries, National Animal Disease Diagnostics and Epidemiology Centre for giving access to data from the animal surveillance platform on anthrax, and the Uganda National Institute of Public Health and Ministry of Health Uganda, and the National One health Platform for giving us access to some of the data used to develop this policy brief. We also appreciate the technical support rendered to use by all the institutions highlighted in this section.
References
- WHO/FAO. Anthrax in humans and animals Fourth edition Food and Agriculture Organization of the United Nations World Organization for Animal Health.
- JK B, E K, F A-B, et al. High Case-Fatality Rate for Human Anthrax, Northern Ghana, 2005-2016. Emerg Infect Dis. 2021;27(4):1216-1219. doi:10.3201/EID2704.204496
- Kisaakye E, Ario AR, Bainomugisha K, et al. Outbreak of anthrax associated with handling and eating meat from a cow, Uganda, 2018. Emerg Infect Dis. 2020;26(12):2799-2806. doi:10.3201/EID2612.191373
- CDC. Experts Team Up to Tackle Deadly Anthrax Across Uganda | Division of Global Health Protection | Global Health | CDC. Accessed August 24, 2021. https://www.cdc.gov/globalhealth/healthprotection/fieldupdates/fall-2018/uganda-tackle-anthrax.html
Reference this page as below
Geoffrey Amanya*, Richard Migisha, Esther Kisakye; Re-Classifying Anthrax as a Public Good Disease: A Policy Brief, Kampala, Uganda. Uganda National Institute of Public Health, 2021 December 30th. Available from:https://uniph.go.ug/re-classifying-anthrax-as-a-public-good-disease-a-policy-brief.

