Syndromic Surveillance during 2022 Uganda Martyrs’ Commemoration
Authors: Mackline Ninsiima1,2*, Mercy Wanyana1,3, Thomas Kiggundu1,2, Patrick King1,3, Bernard Lubwama3, Richard Migisha1, Lillian Bulage1, Daniel Kadobera1, Alex Ario Riolexus1; Institution affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda, 2Kampala Capital City Authority, Kampala, Uganda, 3Division of Integrated Epidemiology and Surveillance, Ministry of Health, Uganda; Correspondence*: Email: mninsiima@uniph.go.ug, +256787819496
Summary
Background: Mass gatherings frequently include close, prolonged interactions between people, which can present opportunities for infectious disease transmission. During May 25−June 5, 2022, over 4 million pilgrims gathered at Namugongo Catholic and Protestant shrines to commemorate the annual Uganda Martyr’s Day. We described syndromes suggestive of key priority diseases among visiting pilgrims during this period to inform future planning for mass gatherings in Uganda.
Methods: We conducted a survey among visiting pilgrims at the Catholic and Protestant shrines based on signs and symptoms for key priority diseases: COVID-19 and Viral Hemorrhagic Fevers (VHFs). A suspected COVID-19 case was defined as ≥2 of: fever >37.50C, flu, cough, and difficulty breathing. A suspected VHF case was defined as fever >37.50C and unexplained bleeding. We sampled systematically every 10th pilgrim in the line at main entrance gates. Other pilgrims were selected randomly from demarcated zonal areas. Overall, 1,350 pilgrims participated voluntarily in the survey. We also extracted secondary data on 5,582 pilgrims who sought medical care from on-site emergency medical services at designated medical tents from Health Management Information Systems (HMIS) registers. Descriptive analysis was conducted to identify syndromes suggestive of key priority diseases.
Results: Among 1,350 pilgrims interviewed, 767 (57%) were female and mean age was 37.9 (±17.9) years. A total of 236 (18%) reported ≥1 case definition symptom and 25 (2%) reported ≥2 symptoms. Twenty-two (1.6%) were suspected COVID–19 cases and three (0.2%) were suspected VHF cases, two from Kampala City and Lira District bleeding from the nose and one from Sironko District had bloody vomitus and urine. Among the 5,582 pilgrims who sought medical care from the medical tents (70.1%, n=3,901) were females whereas (27.5%, n=1,521) were aged 50 years and above. Of these, 538 (9.6%) had suspected COVID-19 and one had suspected VHF. None of the suspected cases had samples collected for laboratory testing.
Conclusion: Almost one in fifty pilgrims at the 2022 Uganda Martyrs’ commemoration had symptoms of COVID-19 or VHF. Despite the epidemic potential for these diseases, none of the case-patients were tested, providing an opportunity for disease introduction and spread. Both intensified syndromic surveillance and planned laboratory testing capacity at mass multi-day gatherings could facilitate early detection of public health emergencies that could stem from such events.
Background
According to World Health Organization (WHO), a mass gathering is an event, either organized or spontaneous, characterized by concentration of people at a specific location for a specific purpose over a set period of time and has the potential to strain planning and response resources of the host country or community (1). During mass gatherings, overcrowding of attendees and influx of non-local travelers may present favourable and conducive environments for close, prolonged and frequent interactions increasing the opportunities for infectious disease transmission. What is quite challenging is that any adverse health outcome associated to mass gatherings would most likely be magnified by media and political attention. Furthermore, occurrence of a disease outbreak at or during an international mass gathering has an increased potential for spreading to neighboring countries or even globally; thus, the need for reporting under the 2005 International Health Regulations (IHR) (2). Influx of people during mass gatherings impacts a strain on existing surveillance and response systems. This presents a challenge to the hosting community or country to strengthen surveillance and response systems during preparation, operational and post-event phases of mass gatherings.
Syndromic surveillance — the utilization of health-related data based on clinical observations and symptoms rather than confirmed diagnosis, can serve as an effective strategy for appropriate real time monitoring, early detection, and timely response to public health events during mass gatherings (1, 3, 4). A provisional diagnosis or a “syndrome” can be established through synthesis of a group of symptoms and clinical observations which consistently occur together. During mass gatherings, syndromic surveillance has been implemented through surveys recording symptoms, review of medical registers completed by medical teams and utilization of automated alert systems; followed by real-time analysis of data to generate incident reports necessary for informing timely response actions (5). To date, syndromic surveillance has been utilized in several mass gathering settings: 2002 Winter Olympic Games in Salt Lake City; 2012 Summer Olympic and Paralympic Games in London; 8th Micronesian Games in 2014, 2015 Los Angeles Special Olympic World Games; religious mass gatherings in Southern India; 2016 Grand Magal of Touba in Senegal; and 2016 Arbaeenia mass gathering in Iraq (3, 5-8). Following the declaration of Ebola Virus Disease Outbreak in Democratic Republic of Congo, the Ministry of Health in collaboration with African Field Epidemiology Network (AFENET) conducted syndromic surveillance for Viral Hemorrhagic Fevers during the 2018 Uganda Martyrs’ commemoration (9).
Every year, pilgrims from Uganda and neighboring countries gather at Namugongo Catholic and Protestant shrines to commemorate the lives of Uganda martyrs on June 3, a religious commemoration of great significance. In 2020 and 2021, Uganda Martyr’s Day was not physically commemorated due to stringent strategies deployed by Ministry of Health to curb the spread of the COVID-19 pandemic during mass gatherings. In February 2022, the Ugandan Government relaxed the restrictions that had been put in place to control COVID-19 thus approving full economy operation. Following the relaxation of the COVID-19 restrictions, Catholic and Protestant religious bodies were permitted to organize the commemoration of Uganda Martyr’s Day; a historical religious event that calls for a mass gathering at Namugongo Catholic and Protestant shrines from May 25−June 5, 2022. Due to the distances people travel to attend this event, an infectious disease outbreak that starts during this mass gathering has high potential to spread to neighboring districts or even to other countries.
During the commemoration of the Uganda Martyrs in 2022, the Ministry of Health in collaboration with the Uganda Catholic and Protestant Medical Bureaus provided health services, including on-site emergency medical services in designated tents from May 25−June 5, 2022. The medical teams available included emergency medicine specialists, doctors, nurses, laboratory attendants, and ambulance teams from Ministry of Health, Mulago National Referral Hospital, St. Francis Hospital Nsambya, Uganda Martyrs Hospital Rubaga, Uganda People’s Defence Forces, Uganda Police Force, Uganda Red Cross Society, St. John’s Ambulance, Holy Family Virika Hospital, Mengo Hospital, Zia Angellina Health Centre, and St. Stephens Hospital. The Ministry of Health also provided HMIS registers where data for pilgrims who sought medical care were captured by the medical teams to achieve harmonized reporting from the different institutions. Additionally, Field Epidemiology Fellows from the Public Health Fellowship Programme were assigned to conduct syndromic surveillance for key priority diseases during the event. In this context, we described syndromes suggestive of key priority diseases among visiting pilgrims, May 25−June 5, 2022 to inform future planning for mass gatherings in Uganda.
Methods
Study site and study population
This assessment was conducted among over 4 million visiting pilgrims from Uganda and neighboring countries gathered at Namugongo Catholic and Protestant shrines located in Namugongo Division, Wakiso District, Uganda.
Data Collection
We utilized two different methods for data collection. First, we conducted a survey among pilgrims at the Catholic and Protestant shrines based on signs and symptoms for key priority diseases from June 2−5, 2022. The data collection tool was developed in KoboCollect based on signs and symptoms for selected priority diseases: COVID–19 and Viral Hemorrhagic Fevers inclusive of Ebola Virus Disease, Crimean Congo Hemorrhagic Fever, Yellow Fever, Rift Valley Fever, and Marburg Hemorrhagic Fever. Signs and symptoms investigated were based on suspect case definitions as per the National Technical Guidelines for Integrated Disease Surveillance and Response. Signs and symptoms under investigation were: fever (temperature above 37.5oC), cough, flu, headache, generalized body weakness, difficulty in breathing, jaundice, fainting or sudden collapse, and unexplained bleeding. Any other signs and symptoms reported by the participants were also recorded by the surveillance officers.
We sampled systematically every 10th pilgrim in the line at main entrance gates. Other pilgrims were selected randomly from demarcated zonal areas. Verbal informed consent was obtained prior to anonymous interviews. Overall, surveillance officers from Makerere University School of Public Health interviewed 1,350 pilgrims who voluntarily participated in the survey. Survey data were downloaded in the Excel (.xls) format from the KoboCollect server and processed for analysis.
Second, we conducted records review based on the on-site emergency medical services provided at the Catholic and Protestant shrines from May 25−June 5, 2022. We extracted all the available data on 5,582 pilgrims who sought medical care from HMIS registers for review including age, sex, district of residence, signs and symptoms or provisional diagnosis.
Data analysis
Data analysis was performed using Epi Info 7 software (Centers for Disease Control and Prevention, Atlanta, Georgia). Frequencies of demographic characteristics and syndromes suggestive of public health emergencies among pilgrims who participated in the survey or sought care from the medical tents were presented. Only syndromes suggestive of key priority diseases were of interest to the investigative team. At analysis phase, a suspected COVID-19 case was defined as ≥2 of: fever >37.50C, flu, cough, and difficulty breathing whereas a suspected VHF case was defined as fever >37.50C and unexplained bleeding.
Ethical considerations
Approval to conduct this project under the Non-Research Determination criteria was obtained from the U. S. Centers of Disease Control and Prevention (CDC). Administrative clearance to extract patient data from the HMIS registers was obtained from the Ministry of Health. All methods were performed in accordance with the approval and administrative clearance.
Results
Characteristics of pilgrims who participated in the survey during, Uganda Martyrs’ commemoration mass gathering, June 2−5, 2022
Among the 1,350 pilgrims who participated in the survey, (56.8%, n=767) were females. Nearly all pilgrims (98.6%, n=1,331) were Ugandans. Only (14.3%, n=153) had visited the Protestant shrine (Table 1).
Table 1: Characteristics of pilgrims who participated in the survey during, Uganda Martyrs’ commemoration mass gathering, June 2−5, 2022
| Characteristic | Frequency (n = 1,350) | Percentage (%) | |
| Age* | |||
| <18 years | 85 | 6.3 | |
| 18–29 years | 409 | 30.3 | |
| 30–39 years | 284 | 21.0 | |
| 40–49 years | 237 | 17.6 | |
| ≥50 years | 335 | 24.8 | |
| Sex | |||
| Male | 583 | 43.2 | |
| Female | 767 | 56.8 | |
| Country of residence | |||
| Uganda | 1331 | 98.6 | |
| Kenya | 9 | 0.7 | |
| South Sudan | 4 | 0.3 | |
| Rwanda | 2 | 0.2 | |
| DRC | 1 | 0.1 | |
| Nigeria | 3 | 0.2 | |
| Religious site visited | |||
| Catholic shrine | 1157 | 85.7 | |
| Protestant shrine | 153 | 14.3 | |
*Median age (IQR): 35 (25 – 49) Mean Age (SD): 37.9 (17.6)
Characteristics of pilgrims who sought medical care from medical tents during Uganda Martyrs’ commemoration mass gathering, May 25−June 5, 2022
Among the 5,582 pilgrims who sought medical care from the medical tents (70.1%, n=3,901) were females whereas (27.5%, n=1,521) were aged 50 years and above (Table 2).
Table 2: Characteristics of pilgrims who sought medical care from medical tents during, Uganda Martyrs’ commemoration mass gathering, May 25–June 5, 2022
| Characteristics | Frequency (n = 5,582) | Percentage (%) |
| Age* (n = 5,525)** | ||
| <18 years | 726 | 13.1 |
| 18–29 years | 1,143 | 20.7 |
| 30–39 years | 1,051 | 19.0 |
| 40–49 years | 1,084 | 19.6 |
| ≥50 years | 1,521 | 27.5 |
| Sex | ||
| Male | 1,668 | 29.9 |
| Female | 3,914 | 70.1 |
| Chronic illness | ||
| Diabetes | 33 | 0.6 |
| Hypertension | 111 | 2.0 |
*Median age (IQR): 38 (25 – 51) Mean Age (SD): 38.6 (18.0)
**Age was not recorded among 57 pilgrims who sought medical care from the medical tents
Suspected priority diseases during Uganda Martyrs’ commemoration mass gathering, May 25–June 5, 2022
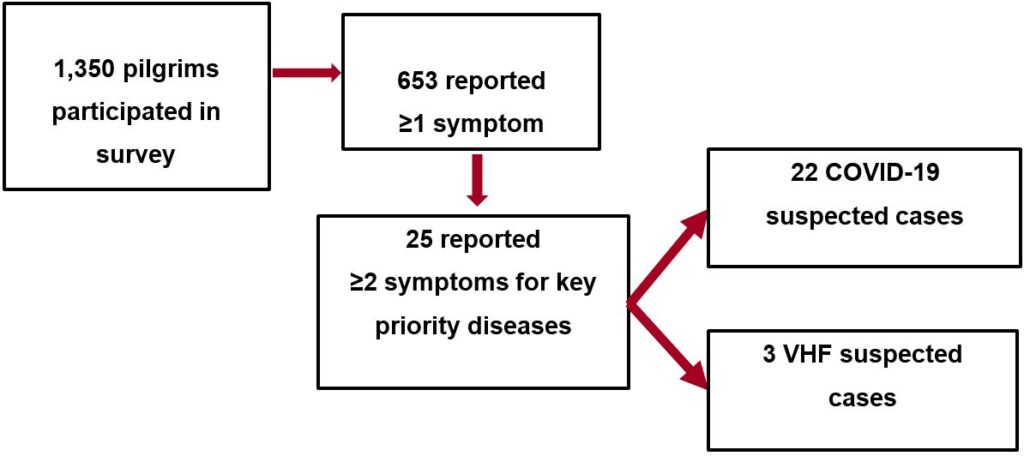
Among the 1,350 pilgrims who participated in the survey, (48.4%, n=653) reported at least one sign or symptom during their visit to the Catholic and Protestant shrines. Of these, 236 (18%) reported ≥1 suspected COVID-19 and Viral Hemorrhagic Fever case definition signs and symptoms and 25 (2%) reported ≥2 symptoms (Figure 1). Twenty-two (1.6%) were suspected COVID–19 cases and three (0.2%) were suspected VHF cases, two from Kampala City and Lira District bleeding from the nose and one from Sironko District had bloody vomitus and urine.
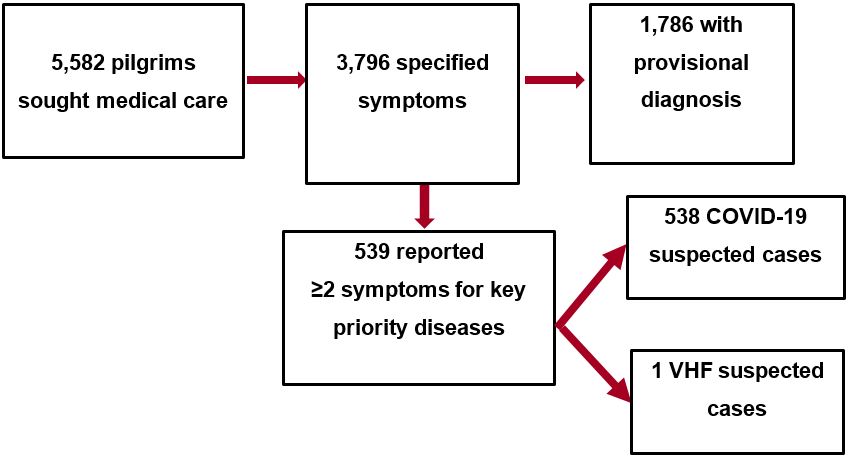
Among 5,582 pilgrims who sought care at the medical tents, 3,796 records specified the presenting signs and symptoms whereas 1,786 records did not have specified signs and symptoms but only had a provisional diagnosis based on the clinician’s assessment. Of 3,796 records, 539 pilgrims reported atleast 2 symptoms suggestive of key priority diseases. Of these, 538 (9.6%) had suspected COVID-19 and one had suspected VHF with bloody vomitus (Figure 2).
Discussion
In this study, we described syndromes suggestive of key priority diseases among visiting pilgrims from May 25−June 5, 2022 to inform future planning for mass gatherings in Uganda. We identified 4 Viral Haemorrhagic Fever and 560 COVID-19 suspected cases through syndromic surveillance during the 2022 Uganda Martyrs’ commemoration. The findings agree with previous incidences where outbreaks have been reported following festive, religious and sporting-related mass gatherings including a COVID-19 outbreak after festivities in Spain; outbreaks of diarrheal diseases during the 2019 Hijja pilgrimage in Saudi Arabia; mumps following festive activities in Austria and Spain; measles after an international youth sporting event in United States of America; meningococcal disease associated with the 23rd World Scout Jamboree gathering in Japan; and influenza H1N1 outbreaks after music festivals in Belgium and Hungary (1, 10-15). Mass gatherings have been highly characterized as transmission sites for infectious diseases due to close proximity and possibility of dissemination of infectious agents after the mass dispersion to different locations (16).
During the COVID -19 pandemic, mass gatherings were highlighted among the sources of transmission due to overcrowding and close interaction between attendees. In 2020, a social gathering at Church X provided an opportunity for a COVID-19 superspreading event in Omoro District, Northern Uganda (17). A recent systematic review reported that religious gatherings in places of worship were vital in COVID-19 transmission accounting for over 50 worship related clusters especially during the first wave of the pandemic (18). Mass gatherings have been significantly associated with COVID-19 transmission (10, 19-21). It should also be noted that risk of transmission of infectious diseases could be partly influenced by the type, venue, location, and demographics of participants who attend the mass gatherings (22-24). Evidence of COVID-19 transmission during mass gatherings has also been reported in Malaysia during the Sri Petaling moslem missionary movement (25). Due to such scenarios, the WHO published interventions which should be implemented to mitigate the spread of COVID-19 during mass gatherings (26).
Limited evidence has been presented on the incidence of Viral Hemorrhagic Fevers during mass gatherings. However, there is still need for great vigilance since most Viral Hemorrhagic Fevers are largely characterized by person to person transmission which could be highly favored by the close contact between attendees during mass gatherings. Experience from mass gathering events held during the West African Ebola epidemic illustrates that these events can be held safely provided interventions are instituted for enhanced surveillance and response systems for infectious diseases (27). This underscores the urgent need of implementing effective measures to mitigate the spread of any Viral Hemorrhagic Fever during a mass gathering; or if possible, postpone the event most especially following the declaration of any Viral Hemorrhagic Fever outbreak.
Study limitations
It should be noted that there were only seventeen trained surveillance officers despite the masses at the Namugongo Protestant and Catholic shrines; who started administering the survey questionnaire on June 2, 2022 instead of having commenced on the May 25, 2022, at the time when pilgrims started gathering. Therefore, it was difficult to generalize the findings on the signs and symptoms for selected priority diseases to the entire population that converged during the 2022 Uganda Martyrs’ commemoration. Additionally, 1,786 out of 5,582 records did not have specified signs and symptoms but only had a provisional diagnosis based on the clinician’s assessment. We could not categorize these pilgrims under any of the key priority diseases since they did not have specified signs and symptoms.
Conclusion
Almost one in fifty pilgrims at the 2022 Uganda Martyrs’ commemoration had symptoms of COVID-19 or Viral Hemorrhagic Fever. Unfortunately, none of the suspected COVID-19 or VHF cases were tested and we do not know what condition they had. While we have no evidence that the suspected VHF cases had any link to the 2022 Ebola Virus Disease outbreak in Uganda, it is clear from these findings that a surveillance system at mass gatherings and the ability to actively respond to possible cases is critical. It is important for us to prioritize intensified syndromic surveillance during mass gatherings to ensure that we reduce the risk for an outbreak at mass gatherings in Uganda and reduce the impact if one should occur. Furthermore, there is utmost need to set up isolation facilities for any suspected cases and provide laboratory testing capacity to facilitate early detection and response to priority key diseases that could stem from such events.
Conflict of interest
The authors declare that they had no conflict of interest.
Acknowledgments
The authors would like to thank medical teams from Ministry of Health, Mulago National Referral Hospital, St. Francis Hospital Nsambya, Uganda Martyrs Hospital Rubaga, Uganda People’s Defence Forces, Uganda Police Force, Uganda Red Cross Society, St. John’s Ambulance, Holy Family Virika Hospital, Mengo Hospital, Zia Angellina Health Centre, and St. Stephens Hospital who provided onsite emergency medical services at the Catholic and Protestant shrines. Additional thanks to surveillance officers from Makerere University School of Public Health who administered survey questionnaires to pilgrims at the Catholic and Protestant shrines.
Copyright and licensing
All materials in the UQEB is in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- WHO. Public health for mass gatherings: key considerations. Available from: https://apps.who.int/iris/bitstream/handle/10665/162109/WHO_HSE_GCR_2015.5_eng.pdf?sequence=1&isAllowed=y. Accessed on: June 12, 2022.
- WHO. International health regulations (2005): Third Edition. Available from: file:///C:/Users/HP/Downloads/9789241580496-eng.pdf. Accessed on: June 12, 2022: World Health Organization; 2016.
- Berry A. Syndromic surveillance and its utilisation for mass gatherings. Epidemiology & Infection. 2019;147.
- Fleischauer AT, Gaines J. Enhancing surveillance for mass gatherings: the role of syndromic surveillance. Public Health Reports. 2017;132(1_suppl):95S-8S.
- Spector E, Zhang Y, Guo Y, Bost S, Yang X, Prosperi M, et al. Syndromic Surveillance Systems for Mass Gatherings: A Scoping Review. International journal of environmental research and public health. 2022;19(8):4673.
- Ganeshkumar P, Muthappan S, Ponnaiah M, Virumbhi V, Thangaraj JV, Muthuperumal P, et al. Syndromic surveillance during religious mass gatherings, southern India 2015–2018. Travel Medicine and Infectious Disease. 2022;47:102290.
- Lami F, Hameed I, Jewad AW, Khader Y, Amiri M. Real-time surveillance of infectious diseases and other health conditions during Iraq’s Arbaeenia mass gathering: cross-Sectional Study. JMIR public health and surveillance. 2019;5(4):e14510.
- Sokhna C, Goumballa N, Van Thuan Hoang BMM, Dieng M, Sylla AB, Diallo A, et al. Senegal’s grand Magal of Touba: syndromic surveillance during the 2016 mass gathering. The American Journal of Tropical Medicine and Hygiene. 2020;102(2):476.
- AFENET. Public Health Surveillance at Namugongo: Martyrs’ Day celebration, Uganda. Available: http://www.afenet.net/index.php/world/63-news-events/420-public-health-surveillance-at-namugongo-martyrs-day-celebration-uganda. Accessed on: 24th August 2022. 2018.
- Domènech-Montoliu S, Pac-Sa MR, Vidal-Utrillas P, Latorre-Poveda M, Del Rio-González A, Ferrando-Rubert S, et al. Mass gathering events and COVID-19 transmission in Borriana (Spain): A retrospective cohort study. PloS one. 2021;16(8):e0256747.
- Karami M, Doosti-Irani A, Ardalan A, Gohari-Ensaf F, Berangi Z, Massad E, et al. Public health threats in mass gatherings: A systematic review. Disaster medicine and public health preparedness. 2019;13(5-6):1035-46.
- Nunan D, Brassey J. What is the evidence for mass gatherings during global pandemics? A rapid summary of best-available evidence. Center for Evidene-Based Medicine (CEBM). 2020.
- Rainey JJ, Phelps T, Shi J. Mass gatherings and respiratory disease outbreaks in the United States–should we be worried? results from a systematic literature review and analysis of the national outbreak reporting system. PloS one. 2016;11(8):e0160378.
- Sassano M, McKee M, Ricciardi W, Boccia S. Transmission of SARS-CoV-2 and other infections at large sports gatherings: a surprising gap in our knowledge. Frontiers in medicine. 2020;7:277.
- Yezli S, Assiri AM, Alhakeem RF, Turkistani AM, Alotaibi B. Meningococcal disease during the Hajj and Umrah mass gatherings. International Journal of Infectious Diseases. 2016;47:60-4.
- Kok J, Blyth CC, Dwyer DE. Mass gatherings and the implications for the spread of infectious diseases. Future Microbiology. 2012;7(5):551-3.
- Thiwe P, Amodan D, Kadobera B, Bulage D, Namayanja L, Akusekera J, et al. Epidemiological assessment of a COVID-19 cluster among attendees of a church activity, Omoro District, Northern Uganda, September 2020. UNIPH Bulletin. 2021;6(3).
- Peano A, Bert F, Lo Moro G, Previti C, Scaioli G, Siliquini R. COVID-19 outbreaks in places of worship worldwide: a systematic review. European Journal of Public Health. 2021;31(Supplement_3):ckab165. 647.
- Furuse Y. Risk at mass-gathering events and the usefulness of complementary events during COVID-19 pandemic. Journal of Infection. 2021;82(3):e20-e1.
- Suñer C, Coma E, Ouchi D, Hermosilla E, Baro B, Rodríguez-Arias MÀ, et al. Association between two mass-gathering outdoor events and incidence of SARS-CoV-2 infections during the fifth wave of COVID-19 in north-east Spain: A population-based control-matched analysis. The Lancet Regional Health-Europe. 2022;15:100337.
- Yasutaka T, Murakami M, Iwasaki Y, Naito W, Onishi M, Fujita T, et al. Assessment of COVID-19 risk and prevention effectiveness among spectators of mass gathering events. Microbial risk analysis. 2022:100215.
- Ebrahim SH, Memish ZA. COVID-19–the role of mass gatherings. Travel medicine and infectious disease. 2020;34:101617.
- Kelvin AA, Halperin S. COVID-19 in children: the link in the transmission chain. The Lancet Infectious Diseases. 2020;20(6):633-4.
- Shi P, Keskinocak P, Swann JL, Lee BY. The impact of mass gatherings and holiday traveling on the course of an influenza pandemic: a computational model. BMC public health. 2010;10(1):1-12.
- Che Mat NF, Edinur HA, Abdul Razab MKA, Safuan S. A single mass gathering resulted in massive transmission of COVID-19 infections in Malaysia with further international spread. Journal of Travel Medicine. 2020;27(3):taaa059.
- WHO. Key planning recommendations for mass gatherings in the context of the current COVID-19 outbreak: interim guidance, 14 February 2020. World Health Organization; 2020.
- Blumberg L, Regmi J, Endricks T, McCloskey B, Petersen E, Zumla A, et al. Hosting of mass gathering sporting events during the 2013–2016 Ebola virus outbreak in West Africa: experience from three African countries. International Journal of Infectious Diseases. 2016;47:38-41


Comments are closed.