Investigation of a Measles Outbreak in Semuto Subcounty, Nakaseke District, Uganda, June–August 2021
Authors: Edirisa Juniour Nsubuga1*, Job Morukileng1, Josephine Namayanja1, Daniel Kadobera1,2, Fred Nsubuga3, Irene Byakatonda Kyamwine1,2, Lilian Bulage1,2, Benon Kwesiga1,2, Alex Riolexus Ario1,2, Julie R. Harris4__ Affiliations: 1Uganda Public Health Fellowship Program, Kampala, Uganda, 2Uganda National Institute of Public Health, Kampala, Uganda, 3Uganda National Expanded Programme on Immunization, Ministry of Health, Kampala, Uganda, 4United States Centers for Disease Control and Prevention, Kampala, Uganda__ * Corresponding author: Email: nsubugaeddiej@musph.ac.ug, Tel: +256704131375
Summary
Background: On 25 August 2021, a measles outbreak was reported in Semuto Subcounty, Nakaseke District. We investigated the outbreak to determine the scope, assess factors associated with transmission, estimate vaccine coverage, and effectiveness, and recommend evidence-based control measures.
Methods: A probable case was an acute onset of fever and generalized maculopapular skin rash with ≥1 cough, cold, or red eyes in a resident of Semuto Subcounty from 1 June–August 31, 2021. A confirmed case was a probable case with a positive blood test for measles-specific IgM. We reviewed medical records to identify cases and snowballed to identify additional community cases. We conducted a 1:4 unmatched case control study.
Results: We identified 30 case-persons, overall subcounty attack rate [AR]=3.2/1,000, with zero deaths. Attack rates increased with age; children aged 5-9 years were the most affected (AR=5.0/1,000). Twenty-two (73%) case-persons and 117 (96%) control persons had received measles vaccine (ORMH=0.13, 95% CI=0.037-0.43). Eighteen (60%) case-persons and 12 (10%) control persons interacted with a symptomatic person (ORMH=15, 95% CI=5.7-41), while 21 (70%) case-persons and 46 (38%) control persons played away from home (ORMH =4.2, 95% CI=1.7-11) during their exposure period. Vaccination coverage was 97% (95% CI: 92-99%); vaccine effectiveness was 86% (95% CI: 45–96%).
Conclusions: Contact with symptomatic persons and playing away from home facilitated measles transmission in this outbreak. Measles vaccination was protective against measles infection. We recommended mass community revaccination for children 6 months to 9 years of age in Semuto Subcounty to capture pockets of unvaccinated children and parents to isolate children with measles-like symptoms.
Introduction
Measles is one of the top five causes of vaccine-preventable morbidity and mortality worldwide (1). Major measles epidemics occurred almost every 2-3 years globally, causing an estimated 2.6 million deaths each year before measles vaccinations were introduced in 1963 (2). More than 140,000 people, who were mostly children aged less than 5 years, died from measles in 2018 despite the availability of a safe and effective vaccine (2).
In Uganda, measles vaccination coverage improved from 73% in 2010 to 95% in 2020 (3). Despite this coverage, Uganda has recorded frequent measles outbreaks in the past decade (2010 to 2020). In the past three years (2018 to 2020), measles outbreaks alone (4) affected 89 (66%) districts in Uganda (Public Health Emergency Compendium Reports, Uganda Public Health Emergency Operations Centre, unpublished data).
Measles is a notifiable disease in Uganda. Measles surveillance is case-based as part of the National Integrated Disease Surveillance and Response System (5). When a measles case is suspected, a case investigation form is completed, and blood samples are submitted to the Uganda Virus Research Institute (UVRI) for laboratory confirmation (5). On 25 August 2021, the Ministry of Health (MoH) was notified of three blood samples that tested positive for measles-specific IgM in the Semuto Subcounty. We investigated the measles outbreak to determine the scope, assess factors associated with transmission, estimate vaccine coverage and effectiveness, and recommend evidence-based control measures.
Methods
Outbreak area
Nakaseke District is located in the central region of Uganda. Semuto Subcounty is located in the south of Nakaseke District. Semuto Subcounty has 4 health centers (HCs), two of which are government-owned (Kalege HC II and Kikandwa HC II), and the other two are privately owned (Kirema HC III and Bukatira HC II). All 4 health facilities provide only outpatient care services, including immunization. These HCs primarily receive vaccines from the Nakaseke District vaccine store and at times from other HCs in the district. The administrative measles vaccination coverage in Nakaseke District from January–August 2021 was 79%, which was more than the expected 66%, while the administrative measles vaccination coverage in Semuto Subcounty from January–August 2021 was 24%, which was below the expected 66% (District Health Information System version 2 (DHIS2), Nakaseke District, 2021, unpublished data) (6).
Case definition and finding
We defined a suspected case as acute onset of fever with at least one of the following: cough, cold, red eyes, or a generalized maculopapular skin rash in a resident of Semuto Subcounty from 1–June to 31–August 2021. A probable case was a suspected case with a generalized maculopapular skin rash and at least one of the following: cough, cold or red eyes. A confirmed case was a suspected or probable case with a positive measles-specific IgM test. We reviewed outpatient medical records in all 4 health facilities in Semuto Subcounty. We line listed all the suspected measles cases. We interviewed the suspected cases to document a detailed clinical history and reclassify them as either probable or not. We used the snowballing approach to search for additional cases from the community. Using an electronic standardized case investigation form, we collected data on the case-person’s demographics, clinical information, vaccination status, and exposure history. Laboratory confirmation was conducted by the Uganda National Expanded Program on Immunization (UNEPI) Laboratory at UVRI using the recommended World Health Organization (WHO) procedures (7).
Descriptive epidemiology
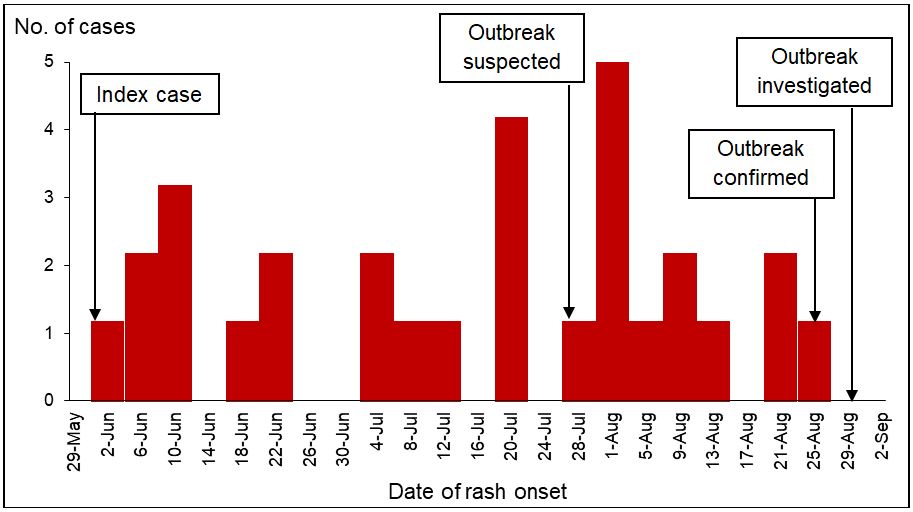
We computed measles attack rates [AR] by person and place using the Uganda Bureau of Standards (UBOS) 2021 projected population of children in Semuto Subcounty as the denominator (6). We constructed an epidemic curve to assess the time distribution of measles cases.
Hypothesis generation
We conducted 11 hypothesis-generating interviews using a standardized measles case investigation form. We asked the case-persons’ caretakers about potential risk factors for measles transmission within the 21 days before symptom onset, including attending social gatherings, attending worship places, visiting health facilities, vitamin A supplementation in the six months before symptom onset, vaccination status before symptom onset evidenced by child health cards or through caretakers’ recall, and confirmed by word of mouth, play site, visiting water collection points, attending medical camps, congestion levels in the household, being in contact with a symptomatic patient, and having received a visitor in the household. We generated hypotheses about exposures based on findings from the descriptive epidemiology analysis and hypothesis-generation interviews.
Case control investigation
We conducted an unmatched case control investigation in the 3 affected parishes (Segalye, Kirema, and Kikandwa) of the Semuto Subcounty to test the hypothesis. We investigated children aged 6 months to 9 years because all cases were in this age range. We interviewed the caregivers and administered an electronic questionnaire to the guardians or caregivers since all the case-persons were minors. We considered only probable or confirmed measles cases for the case–control. We recruited all 30 case-persons we identified, 3 of which were confirmed. We defined a control as any person aged 6 months to 9 years without signs and symptoms of measles from 1 June to 31 August 2021 residing in the three affected parishes of Semuto Subcounty. We selected cases and controls at a ratio of 1:4. We used simple random sampling to select controls from the same village as cases. Our sampling frames were the village health team (VHT) household lists. We used Epi Info 7.2.4.0 for analysis. To assess factors associated with measles infection, we stratified by parish and obtained Adjusted Mantel-Haenszel Odds Ratios (ORMH) (8, 9) and their corresponding 95% confidence intervals (CIs) (10). We also merged all the variables that dealt with meeting symptomatic persons (met a symptomatic person at a water point, shared home with a symptomatic person, met a symptomatic person at a health facility) and came up with a new variable about meeting a symptomatic person generally.
Vaccination coverage (VC) and vaccine effectiveness (VE)
We estimated the one-dose VC by using the percentage of controls that had a history of measles vaccination in our case control investigation. We calculated the measles VE using the formula VE =1-ORMH (11), where ORMH was the protective Mantel–Haenszel odds ratio associated with having been vaccinated with at least one dose of the measles vaccine estimated from the case control investigation.
Ethical considerations
The Ministry of Health of Uganda gave the directive and approval to investigate this outbreak. In agreement with the International Guidelines for Ethical Review of Epidemiological Studies by the Council for International Organizations of Medical Sciences (1991) and the Office of the Associate Director for Science, CDC/Uganda, it was determined that this activity was not human subject research and that its primary intent was public health practice or disease control activity (specifically, epidemic or endemic disease control activity). Verbal informed consent was obtained from the participants before the start of each interview. Parental/legal guardian verbal informed consent was obtained on behalf of all the children before the start of each interview since they were aged less than 10 years.
Results
Descriptive epidemiology
We identified 30 case-persons (27 probable and 3 confirmed cases) and no deaths. The overall subcounty attack rate [AR] was 3.2/1000. The most affected parish was Segalye (AR=9.5/1,000), followed by Kikandwa (AR=7.4/1,000) and Kirema (AR=3.0/1,000). The age range of the case-persons was 6 months to 9 years. The most affected age group was 5-9 years (AR=5.0/1,000), followed by 1-4 years (AR=2.6/1,000). The attack rate was similar between males (3.3/1,000) and females (3.2/1,000).
All (100%) cases presented with a history of fever, a generalized rash, and red eyes. Twenty-seven (90%) had a history of cough and cold. Ten (33%) had pneumonia, 8 (27%) had oral and throat sores, and 2 (6.7%) had otitis media as complications of measles.
The epidemic curve (Figure 1) showed a propagated measles outbreak. The outbreak lasted 88 days. On 2 June 2021, the index case of the outbreak was identified in the Kirema Parish of Semuto Subcounty. The outbreak was not suspected until 28 July 2021, when health workers in Kalege Health Center II received reports of children with measles-like symptoms in the community. The outbreak was confirmed on 25 August 2021. Investigations started on 29 August 2021. The last case occurred between 25 and 28 August 2021.
Hypothesis generation findings
Of the 11 case-persons, 8 (73%) had visited a water collection point during the exposure period, 3 (27%) did not receive vitamin A supplementation in the six months preceding the infection, 3 (27%) played in the neighborhood, and 2 (18%) were not vaccinated. None of the case-persons reported having the other exposures. We, therefore, considered a visit to a water collection point, vitamin A supplementation, playing in the neighborhood, vaccination status, and visiting a health facility as the likely drivers for this outbreak.
Case control study findings
Twenty-two (73%) case-persons and 117 (96%) control persons were vaccinated (ORMH =0.13, 95% CI: 0.037-0.43). Nine (30%) case-persons and 12 (10%) control persons met a symptomatic person at a water collection point (ORMH =4.4, 95% CI: 1.6-12). Eighteen (60%) case-persons and 12 (10%) control persons met a symptomatic person generally (ORMH =15, 95% CI: 5.7-41). Twenty-one (70%) case-persons and 46 (38%) control persons played away from home (ORMH =4.2, 95% CI: 1.7-11). The other exposures assessed in the case control were not significantly associated with measles infection (Table 1).
Among control persons aged ≥9 months to 9 years, we estimated vaccination coverage to be 97% (95% CI: 92-99%). We estimated VE=86% (95% CI: 45–96%) among 22 (79%) case-persons compared to 116 (97%) control persons with a history of measles vaccination (ORMH =0.14; 95% CI: 0.037–0.55).
Table 1: Factors associated with the measles outbreak, Semuto Subcounty, Nakaseke District, Uganda, June–August 2021
| Risk factor | Cases %(n) | Controls %(n) | ORMH (95% CI) |
| Measles vaccination | 73 (30) | 96 (122) | 0.13 (0.037-0.43) * |
| Received vitamin A in last 6 months | 50 (30) | 45 (29) | 2.5 (0.77-7.9) |
| Visited health facility | 20 (26) | 17 (121) | 1.3 (0.47-3.6) |
| Travel to a different area during the exposure period | 3.3 (30) | 7.4 (122) | 0.44 (0.052-3.6) |
| Longline at a health facility | 33 (30) | 27 (122) | 1.4 (0.59-3.3) |
| Visit water collection point | 73 (30) | 67 (122) | 1.4 (0.55-3.3) |
| Played at a water collection point | 50 (30) | 56 (121) | 0.8 (0.35-1.8) |
| Long lines at a water collection point | 33 (6) | 25 (20) | 1.7 (0.21-14) |
| Met a symptomatic person at a water point | 30 (30) | 10 (120) | 4.4 (1.6-12) * |
| Shared home with a symptomatic person | 57 (30) | 0 (122) | Undefined ** |
| Met a symptomatic person at a health facility | 0 (6) | 20 (20) | Undefined ** |
| Generally, met a symptomatic person | 60 (30) | 10 (120) | 15 (5.7-41) * |
| Played away from home | 70 (30) | 38 (122) | 4.2 (1.7-11) * |
* Significant association at p value <0.05
** Undefined due to having “0” in some cells
Discussion

Our investigation showed that this community outbreak was mild and affected only 3 parishes in the Semuto Subcounty. Older children aged 5-9 years were the most affected. Measles infection was lower among vaccinated children. The outbreak was propagated by children playing away from home and meeting symptomatic measles case-persons. The high vaccination coverage and suboptimal vaccine effectiveness may have reduced community susceptibility to infection.
Measles infection increased with an increase in age. A shift in the age distribution of measles cases toward older age groups has also been described in other countries (12). The findings in this investigation could be due to waning immunity (13) and the accumulation of the susceptible population as the children grow older. The waning immunity with age may have increased the susceptibility of the older children to measles infections. This can be avoided in the future by introducing a second dose of the measles-rubella vaccine for older children into the national routine immunization schedule (14). Contrary to the findings in this outbreak, an investigation of a measles outbreak in the Somali Region of Ethiopia showed that the younger age group <1 year was the most affected compared to all other age groups (15). This could be due to the difference in vaccination coverage in the two regions at the time of the outbreaks. The current outbreak occurred in an area with high vaccination coverage, whereas the outbreak in the Somali Region occurred in an area with very low vaccination coverage of the <1-year-olds (15).
This investigation showed that the history of being vaccinated with the measles vaccine was protective against measles virus infection. This is in line with findings from other measles outbreak investigations conducted in Ethiopia that found that being vaccinated with the measles vaccine was protective against measles (16). Other investigations conducted in Uganda and China also noted that not being vaccinated against measles was a risk factor for measles infection (17, 18). The current outbreak mainly occurred among pockets of un-vaccinated children. These un-vaccinated children exposed some of the vaccinated children to measles infection. The findings in this investigation are expected because measles vaccination is the best approach for preventing measles infections and outbreaks (2). The measles vaccine confers immunity to the person who has been vaccinated, and the WHO recommends at least 2 doses of measles vaccine to be administered at 9 and between 15–18 months of age (19). One can also get immunity through being infected with measles, but it comes with severe complications (2).
Children who met with symptomatic measles case-persons while at the water collection points were more likely to contract measles than those who did not meet any symptomatic measles case-persons at the water collection point. This finding is similar to findings in another outbreak investigation, where measles was associated with the congregation of children at water collection points (18). This is not surprising since measles is an airborne disease (1, 2). In this community, similar to most African settings, women are the default caretakers for children (18). These women usually move with children as they collect water for domestic use. The older children aged more than 5 years at times go without adults. For adults, water collection points are meeting points where they converse with each other. As the children wait for the adults to fill up the water collecting containers and finish their conversations, they mingle and play with other children. If one of the children is symptomatic and in the infectious phase, this facilitates transmission of measles to the other children, as was demonstrated in several other studies (18). Contrary to the findings in our investigation, visiting water collection points was protective in another outbreak investigation (20), which was due to it being a sign of healthy children and therefore a lower chance of visiting a pediatric ward in a hospital, which was the source and site of the outbreak at the time.
During this outbreak, playing away from home and meeting a symptomatic person were generally strongly associated with measles infection. These findings agree with results from several other studies (18), which demonstrated that congregation settings facilitate measles transmission. As children move away from their homes to other places to play with other children, their chances of getting in contact with an infected measles person increase. This is not surprising since measles is a highly contagious airborne infection that is transmitted from an infected person to a noninfected person via the respiratory route or through direct contact with the infected person (2).
This was a mild measles outbreak with vaccine coverage and vaccine effectiveness falling in the recommended ranges (2). Other studies have also shown that measles outbreaks can occur in communities with >95% vaccine coverage and with documented vaccine effectiveness of >85% (21). However, most previous investigations have shown that measles outbreaks are primarily due to low vaccine coverage of <95%, low vaccine effectiveness of <85%, or both (15), which is understandable due to the existence of a susceptible population and lack of herd immunity. The vaccination coverage and vaccine effectiveness in this investigation could explain the small size and limited spread of this outbreak (22). The findings in this investigation are also consistent with reports that when measles occurs in immunized individuals, the illness is less severe (23). This is also predictable since the measles vaccine is not 100% effective (21). Uganda currently administers a one-dose measles-rubella-containing vaccine to children at 9 months as part of the routine vaccination schedule (24). Measles outbreaks still occur even in countries with high vaccination coverage of the two-dose measles vaccine because a susceptible population still accumulates fairly swiftly (21). Therefore, it is not surprising that measles outbreaks still occur in Uganda.
Study limitations
This investigation had some limitations. The lack of a sufficient sample size rendered it impossible to conduct a more detailed analysis (multivariate regression analysis) to control for confounding. Vaccination status was based on caretakers’ recall, which might have led to recall bias leading to an overestimation of vaccine effectiveness and vaccination coverage. In this investigation, we assumed that the controls were representative of the general population and used the proportion of controls vaccinated to estimate vaccination coverage instead of the standard WHO community survey method. This result might have overestimated the vaccination coverage. Additionally, we could not triangulate with the administrative coverage, since vaccination records in some of the health facilities were not up to date, hence, the low administrative coverage compared to the calculated vaccination coverage. We did not ascertain the history of measles infection outside our exposure and outbreak period as a source of measles immunity among the controls, which could have confounded the calculation of vaccine effectiveness.
Conclusion
We concluded that contact with symptomatic children either at home or at a water collection point and playing away from home were associated with this measles outbreak. Measles vaccination was protective against measles infection. The vaccination coverage and vaccine effectiveness could not explain the occurrence of this outbreak.
We recommended that the Nakaseke District Health team conduct a mass community measles revaccination campaign for all children 6 months to 9 years in Semuto Subcounty to capture pockets of unvaccinated children in the area and act as the booster dose for those who might have received only one dose. Parents and guardians to isolate children with measles-like symptoms. Children who had not received the measles-rubella vaccines were referred to the nearby health facilities, where they received their vaccines.
Acknowledgement
The authors would like to thank Nakaseke District leadership, including the District Health Team who spearheaded the district outbreak response efforts, Mr. Yawe Moses the Biostatistician, and the District Surveillance Focal Person of Nakaseke District for coordinating the investigation activities. Ms. Namisango Christine, a Nurse at Kalege Health Centre III, is also acknowledged for her vigilance in identifying the measles cases as well as involvement in the investigation.
References
- Control CfD, Prevention. Vaccine preventable deaths and the Global Immunization Vision and Strategy, 2006-2015. MMWR Morbidity and mortality weekly report. 2006;55(18):511-5.
- WHO. Measles Fact Sheets WHO Website: World Health Organisation; 2019 [updated 5 December 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/measles.
- Uganda: Measles vaccination coverage [Internet]. World Health Organisation. 2021 [cited December 6, 2021]. Available from: https://immunizationdata.who.int/pages/coverage/MCV.html?CODE=UGA&ANTIGEN=MCV1&YEAR=.
- UGANDA LAUNCHES NATIONAL MEASLES- RUBELLA AND POLIO IMMUNISATION CAMPAIGN [Internet]. Ministry of Health, Republic of Uganda. 2019 [cited 06/11/2021]. Available from: https://www.health.go.ug/2019/11/27/uganda-launces-national-measles-rubella-and-polio-immunisation-campaign/.
- MoH. National technical guidelines for integrated disease surveillance and response. Kampala: Uganda Ministry of Health; 2012. p. 437.
- UBOS. The National Population and Housing Census 2014 – Main Report. Kampala: Uganda Bureau of Statistics; 2016.
- WHO. Manual for the Laboratory Diagnosis of Measles and Rubella Virus Infection. 2nd ed. Geneva: World Health Organisation; 2007.
- Analysis of case control studies [Internet]. Available from: https://sites.google.com/site/outbreaktoolkit/website-builder/analysis-of-case-control-studies?tmpl=%2Fsystem%2Fapp%2Ftemplates%2Fprint%2F&showPrintDialog=1.
- MANTEL-HAENSZEL TEST [Internet]. National Institute of Standards and Technology, Statistical Engineering Division. [cited 06/11/2021]. Available from: https://www.itl.nist.gov/div898/software/dataplot/refman1/auxillar/mantel.htm.
- Fleiss JL, Levin B, Paik MC. Statistical methods for rates and proportions: john wiley & sons; 2013.
- Weinberg GA, Szilagyi PG. Vaccine epidemiology: efficacy, effectiveness, and the translational research roadmap. The Journal of infectious diseases. 2010;201(11):1607-10.
- Wichmann O, Siedler A, Sagebiel D, Hellenbrand W, Santibanez S, Mankertz A, et al. Further efforts needed to achieve measles elimination in Germany: results of an outbreak investigation. Bulletin of the World Health Organization. 2009;87:108-15.
- Yang L, Grenfell BT, Mina MJ. Waning immunity and re-emergence of measles and mumps in the vaccine era. Current opinion in virology. 2020;40:48-54.
- WHO. M-M-R® II (MEASLES, MUMPS, and RUBELLA VIRUS VACCINE LIVE). 2004.
- Mohammed Y, Alemu A. Measles Outbreak Investigation and Response in Jarar Zone of Ethiopian Somali Regional State, Eastern Ethiopia. 2017;8:86-91.
- Yusuf M, Ayalew N. Measles Outbreak Investigation and Response in Jarar Zone of Ethiopian Somali Regional State, Eastern Ethiopia. Int J Microbiol Res. 2017;8(3):86-91.
- Hao L, Ma C, Wannemuehler KA, Su Q, An Z, Cairns L, et al. Risk factors for measles in children aged 8 months–14 years in China after nationwide measles campaign: A multi-site case-control study, 2012–2013. Vaccine. 2016;34(51):6545-52.
- Majwala RK, Nakiire L, Kadobera D, Ario AR, Kusiima J, Atuhairwe JA, et al. Measles outbreak propagated by children congregating at water collection points in Mayuge District, eastern Uganda, July–October, 2016. BMC infectious diseases. 2018;18(1):1-7.
- Immunization, Vaccines and Biologicals: Measles [Internet]. World Health Organisation. [cited 15 December 2021]. Available from: https://www.who.int/teams/immunization-vaccines-and-biologicals/diseases/measles.
- Biribawa C, Atuhairwe JA, Bulage L, Okethwangu DO, Kwesiga B, Ario AR, et al. Measles outbreak amplified in a pediatric ward: Lyantonde District, Uganda, August 2017. BMC infectious diseases. 2020;20:1-8.
- Marin M, Nguyen HQ, Langidrik JR, Edwards R, Briand K, Papania MJ, et al. Measles transmission and vaccine effectiveness during a large outbreak on a densely populated island: implications for vaccination policy. Clinical infectious diseases. 2006;42(3):315-9.
- Yeung LF, Lurie P, Dayan G, Eduardo E, Britz PH, Redd SB, et al. A limited measles outbreak in a highly vaccinated US boarding school. Pediatrics. 2005;116(6):1287-91.
- Aaby P, Bukh J, Leerhøy J, Lisse IM, Mordhorst CH, Pedersen IR. Vaccinated children get milder measles infection: a community study from Guinea-Bissau. Journal of infectious diseases. 1986;154(5):858-63.
- MOH. Immunisation guidelines by the Uganda National Expanded Programme on Immunisation (UNEPI). Kampala: Ministry of Health; 2019.
Reference this page as below
Edirisa Juniour Nsubuga1*, Job Morukileng1, Josephine Namayanja1, Daniel Kadobera1,2, Fred Nsubuga3, Irene Byakatonda Kyamwine1,2, Lilian Bulage1,2, Benon Kwesiga1,2, Alex Riolexus Ario1,2, Julie R. Harris4. Investigation of a Measles Outbreak in Semuto Subcounty, Nakaseke District, Uganda, June–August 2021. Kampala, Uganda National Institute of Public Health. 2022 March 30th. Available from:https://uniph.go.ug/investigation-of-a-measles-outbreak-in-semuto-subcounty-nakaseke-district-uganda-june-august-2021.

