Anthrax outbreak associated with consumption and handling of meat from suddenly dead cattle, Kabira Sub-County, Kyotera District, Uganda, June–December 2023
Authors: Lawrence Tumusiime¹*, Dominic Kizza¹, Anthony Kiyimba¹, Esther Nabatta¹, Aggrey Byaruhanga², Benon Kwesiga¹, Richard Migisha¹, Alex Riolexus Ario¹; Institutional affiliations: ¹Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda; ²Department of Integrated Epidemiology Surveillance and Public Health Emmergency, Ministry of Health, Kampala, Uganda; Correspondence*: Tel: +256779712458, Email: ltumusiime@uniph.go.ug
Summary
Background: In November 2023, a strange illness was reported in Kabira Sub-County Kyotera District, characterized by itching, rash, swelling, and skin lesions. Subsequent investigation confirmed the illness as anthrax. We investigated to assess its magnitude, identify potential exposures, and propose evidence-based control measures.
Methods: A suspected cutaneous anthrax case was acute onset of skin itching or swelling plus ≥2 of skin reddening, lymphadenopathy, headache, fever, general body weakness in a resident of Kabira sub-county, June–December, 2023. A suspected gastrointestinal anthrax case was acute onset of ≥2 of abdominal pain, vomiting, diarrhea, mouth lesions, neck swelling, in a resident of Kabira sub-county, June–December, 2023. A confirmed anthrax case was a suspected case with Bacillus anthracis PCR-positive results. We reviewed medical records and community active case-finding. In a case-control study, we compared exposures between 50 case-patients and 200 neighborhood controls.
Results: We identified 63 cases (46 suspected and 17 confirmed); most (n=48; 76%) were male. Of these, 55 cases (87%) were cutaneous and 8 (13%) were gastrointestinal, with a mean age of 42 years. Overall attack rate was 3.1/1,000; males were more affected (4.5/1,000) than females (AR=1.5/1,000). Case-fatality rate was 19% (n=12). Only 29% (n=18) of the cases sought care from health facilities with majority (52%, n=33) being managed from shrines by traditional healers. 74% (37/50) case-patients and 21% (41/200) control-persons consumed meat from cattle that died suddenly (aOR = 6.19; 95% CI: 2.76–13.9). 62% (31/50) case-patients and 18% (36/200) control-persons had contact with meat or other products from animals that died suddenly (aOR = 2.52; 95% CI: 1.08–5.91).
Conclusion: The anthrax outbreak in Kyotera District was primarily attributed to the consumption and handling of meat from suddenly deceased cattle. To prevent future outbreaks, we recommended implementing inspection protocols for cattle before slaughter, instituting widespread vaccination campaigns against Bacillus anthracis in livestock and community sensitization on healthcare seeking. These proactive measures could reduce the risk of anthrax transmission to humans and mitigate the impact of outbreaks on public health and agricultural livelihoods in the region.
Background
Anthrax is a serious infectious zoonotic disease caused by gram-positive, rod-shaped, and spore forming bacteria known as Bacillus anthracis(1). The bacteria naturally present in soil and causes severe illness in both animals and humans. Domestic and wild animals become infected when they breathe in or ingest spores in contaminated soil, plants or water(2). The age, sex and condition of animals may all influence the incidence of the disease at any one site(3). There are no reports of person to person transmission of anthrax, people get sick with anthrax through contact with infected animals or occupational exposure to infected or contaminated animal products (e.g. hair, wool, hides, bones)(4). When anthrax spores get inside the body, they are activated, multiply, spread out in the body, produce toxins, and cause severe illness(5). The incidence of the disease depends on the level of exposure to the affected animals. In contrast to animals, age- or sex-related bias is generally not apparent in humans, though males generally have higher occupational risk rates in many countries(6).
Human anthrax infection is classified into four forms depending on the route of exposure, with varying degree of severity and incubational period; cutaneous (1–12 days), inhalational (1–60 days), gastrointestinal (1–6 days), injectional (1–10 days)(7).
Cutaneous anthrax is the most common form, accounting for >95% of human cases, and results from direct contact with or exposure to infected animals or contaminated animal products(8). It is typically a localized skin infection, often occurring on the face, neck, arms, or hands.
Approximately 2,000 to 20,000 cases of human anthrax are reported globally annually, with 75% occurring in African countries with low livestock vaccination rates(9). Uganda has reported sporadic anthrax outbreaks in different sub regions of the country(10). The outbreaks mainly occurs in areas where people commonly keep livestock primarily within western, eastern, and northern Uganda(11).
On November 21, 2023, a strange illness was reported in Kabira Sub-County, Kyotera District, characterized by itching, rash, swelling, and skin lesions. Subsequent investigation confirmed the illness as anthrax. We investigated to assess its magnitude, identify potential exposures, and propose evidence-based control measures.
Methods
Outbreak area
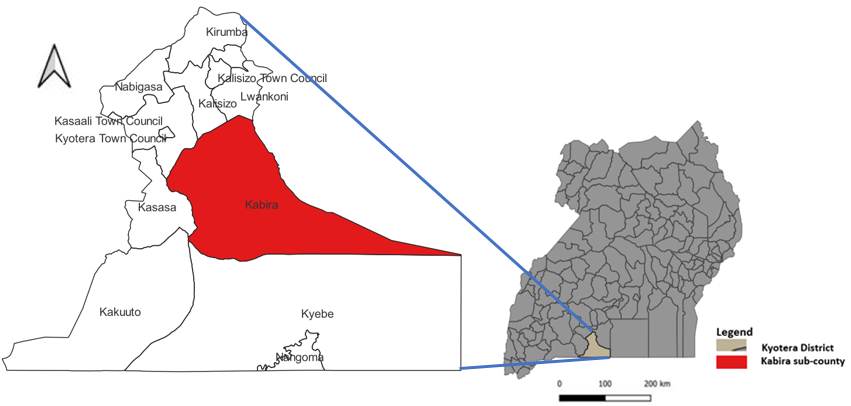
This outbreak occurred in Kabira Sub-County, Kyotera District which is located in the South Western part of Uganda (Figure 1). The district has a total area of 1,722 (sq. km), with a population of approximately 261,000 (12). Agriculture forms the backbone of the economy of the district although most of the agriculture is at subsistence level.
Case definition and case finding
We defined a suspected case as follows:Cutaneous anthrax: Acute onset of skin itching or swelling plus ≥2 of; skin reddening, lymphadenopathy, headache, fever, general body weakness in a resident of Kabira sub-county from June–December 2023 OR Gastrointestinal anthrax: An acute onset of ≥2 of the following symptoms; abdominal pain, vomiting, diarrhea, mouth lesions, neck swelling, in a resident of Kabira sub-county from June–December 2023. A Confirmed anthrax case: A suspected case patient with PCR-positive results for Bacillus anthracis.
We conducted house to house and health facility active case search using our case definition to identify case-patients in the affected areas since June 1, 2023. We also asking already identified case-patients to lead us to people with similar signs and symptoms in the community. We interviewed identified case-patients to identify possible exposures for contracting Anthrax.
Descriptive epidemiology
We calculated proportions to describe the distribution of case-persons by age, sex, and symptoms. We also described case-persons by time of onset of symptoms using an epidemiological curve and calculated attack rates to describe the distribution of cases by age, sex, and parish.
Laboratory Investigations
In humans, 57 samples (30 whole blood and 27 swabs) were collected from anthrax-suspected cases and available fluids from lesions. In cattle, 24 samples (18 swabs and 6 body tissue (ear lobe) were collected from carcasses and cattle already butchered. All samples were packaged using a triple package technique and transported using the hub system to the Uganda Virus Research Institute (UVRI) in Arua and the National Animal Disease Diagnostics and Epidemiology Centre (NADDEC) laboratory in Entebbe Uganda for anthrax testing in humans and animals respectively.
Environmental investigations
We inspected animal farms in the affected villages using snowballing and house-to-house visits to identify farms that had reported sudden death of cattle, goats or sheep within Kabira Sub County between June 1, 2023 and December 15, 2023. We interviewed the farm owner and herdsman to gather information on the farm management practices and how the meat and other animal products were distributed. We visited the affected farms and observed the pasture in the grazing area, and also areas where the cattle were slaughtered or buried. We interviewed the identified dealers of meat from cattle that had died suddenly and slaughtered for distribution.
Hypothesis generation interviews
We conducted interviews with the 63 suspected cases to identify possible sources and factors associated with contracting anthrax. We explored for meat consumption from cattle that died suddenly, contact with livestock that suddenly died, presence of skins and hides, animal ownership, and occupation.
Case-control study
To test the hypotheses, we conducted a case-control study in the in Kabira sub-county, Kyotera District. We recruited and interviewed the first 50 case-patients on the line list in the case-control study. For each case-patients, we selected 4 control persons. A control person was an individual who never had any signs of cutaneous or gastrointestinal anthrax from June 1, 2023 to the time of the investigation, resident in the same village as the case-patient. To randomly select control persons, we obtained the locations of case patients’ households and spun a bottle while at these households to obtain the first control-person household. The bottle was spun after every interview until the four different households were got. All members present in the households at the time of data collection were listed and one was chosen randomly as a control-person.
For each case and control, we obtained information on their meat consumption history, contact with dead livestock (slaughtering, dissecting, carrying), eating meat of an animal that had died suddenly, the clinical characteristics, as well as demographic variables.
We used logistic regression to identify factors associated with anthrax. Variables that had a p-value <0.2 at bivariate level were included in the final model for multivariable analysis and corresponding adjusted odds ratios (aOR’s) and 95% confidence intervals were reported.
Ethical considerations
This investigation was a response to a public health emergency. The Ministry of Health (MOH) gave permission to investigate the deaths and the Centre for Global Health, US Center for Disease Control and Prevention determined the activity as non-human research but rather aimed at improving public health practices or disease control. We sought permission to conduct this investigation from Kyotera District health authorities. We also sought verbal informed consent from the respondents who were caretakers of the deceased, family members and suspect cases. The respondents were informed that their participation was voluntary and were free to continue or opt out with no negative consequences. The data collected was coded with no individual personal identifiers so as to maintain confidentiality.
Results
Descriptive epidemiology
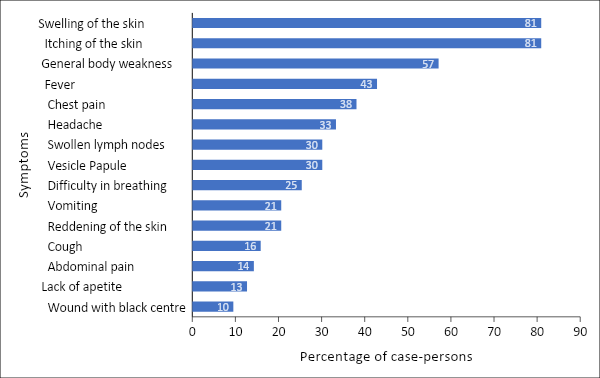
We line listed 63 Anthrax case-patients, with 17 confirmed and 46 suspected as of December 31, 2023. Seventy-six percent (n=48) were males, 12 case-patients died, with an overall attack rate of 3.1/1,000 population and case fatality rate of 19%. Of the 63 case-patients, 55 were cutaneous and 8 gastrointestinal, with a mean age of 42 years (interquartile range: 13-75 years). Males were more affected (AR: 4.5/1,000) than females (AR: 1.5/1,000), age-group 50-69 was most affected (AR = 14/1,000). Swelling of the skin (81%), itching of the skin (81%) and general body weakness (57%) were the most common sign and symptom of illness among case-persons (figure 2). Only 29% of the case-patients sought care from Health facilities.
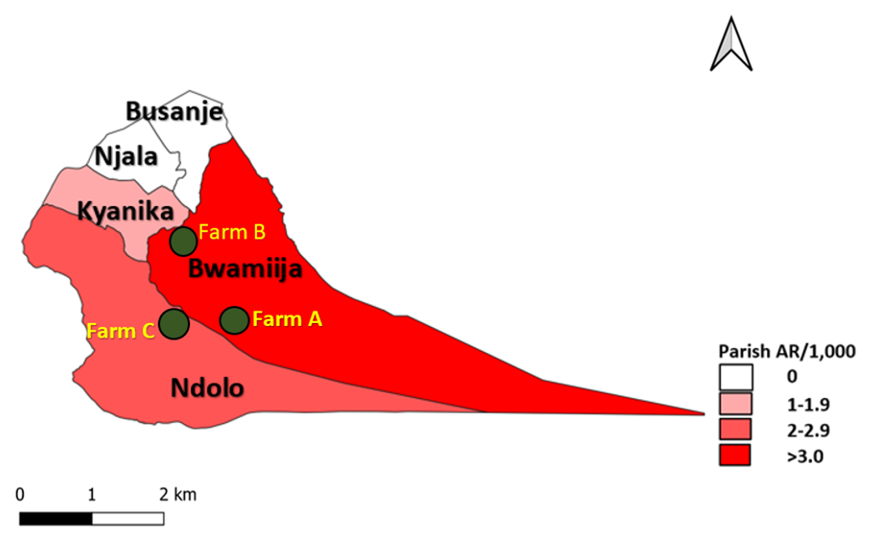
As of December 31, 2023, a total of three parishes of Bwamijja, Ndolo and Kyanika were affected. Bwamijja parish was the most affected (AR: 5.3/1,000), followed by Ndolo (AR: 2.6/1,000) while Kyanika was the least affected (AR: 1.4/1,000) (Figure 3).
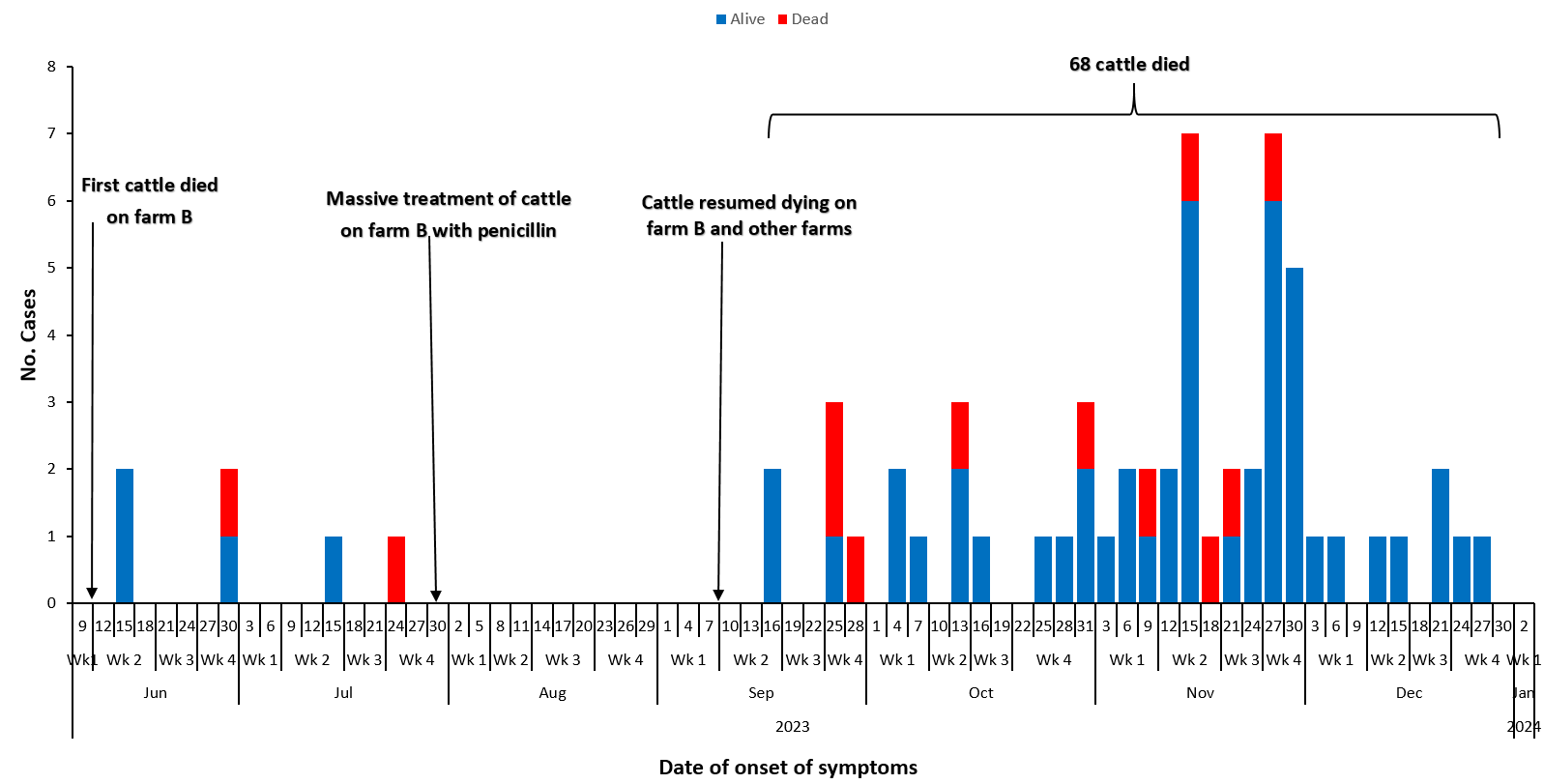
Following the sudden death and slaughtering of an animal on Farm B on June 10, 2023, case-persons started to appear from June 15, 2023 (Figure 8). There was no case-person recorded from July 27, 2023 up to September 13, 2023. This coincided with no animal deaths reported following a massive treatment of cattle on Farm B with penicillin therapy. Case-persons reappeared starting September 16, 2023 just 1 week after cattle had resumed dying on farm B and two other farms. The number of case-persons rapidly increased and peaked in November, 2023. This epidemic curve suggests a multiple-source outbreak.
Laboratory investigation findings
A total of 81 (57 human and 24 cattle) samples were collected and tested for Bacillus anthracis. Seventeen of the human samples returned PCR positive (positivity rate of 30%) while we were not able to obtain results of the 24 animal results.
Environmental assessment findings
There were 68 suspected cases of animal anthrax that died on three different farms (A, B & C) located in Kidda, Kyamayembe, and Kifambi villages in Bwamiija and Ndolo parishes respectively in Kabira sub-county. These three farms share one stream of drinking water with two of them (Farm A and C) having a common point of drinking water. The first animal died on farm B on June 10, 2023, and the dead animal was slaughtered by meat dealers who sold it to the surrounding community at the trading centers of Kyanika, Kyamayembe, and Kifambi at an average price of $1.28 per Kilogram. Farm B subsequently lost 22 cattle, and all of them were sold to the local community by the meat dealers. According to the farm manager, the deaths of cattle on farm coincided with the heavy rains. An organized network of people dealing in cheap meat from cattle that died suddenly was discovered in Kabira Sub-county, Kyotera District. We also identified an area next to dead meat stall where meat was prepared very fast for the slaughtering teams and people drinking in the next bar. Boiled meat termed ‘Huta Huta ko’ was sold cheaply to people such that it’s affordable for everyone.
Hypothesis generation
Based on the 63 hypothesis generating interviews, 79% of the respondents indicated they had consumed meat from cattle that had died suddenly, 63% had contact with dead livestock, wildlife or their body fluids, while 33% had participated in slaughtering or handling of animal products. We hypothesized that consuming and handling meat from cattle that died suddenly were associated with the December 2023 anthrax outbreak in Kyotera District.
Case-control study findings
Following adjustment for age and sex in the case-control investigation, 74% (37/50) of case-patients compared to 21% (41/200) of control-persons consumed meat from an animal that had died suddenly (aOR = 6.19; 95% CI: 2.76–13.9). In addition, 62% (31/50) of case-patients compared to 18% (36/200) had contact with meat or other products from cattle that had died suddenly (aOR = 2.52; 95% CI: 1.08–5.91).
Table 1: Distribution of exposure status among cases and controls during an anthrax outbreak: Kyotera District, Uganda, June–December, 2023
| Variables | Cases, n=50(%) | Controls, n=200(%) | Crude ORs
(95% CI) |
Adjusted ORs (95% CI) |
| Consumed dead cattle meat | 37(74.0) | 41(20.5) | 11.0 (5.38, 22.7) | 6.19 (2.76, 13.9) |
| Contact with meat or other products from dead cattle | 31(62.0) | 36(18.0) | 7.43 (3.78, 14.6) | 2.52 (1.08, 5.91) |
| Butcher man | 8(16.0) | 3(1.5) | 2.52 (1.15, 3.89) | 2.77 (1.04, 4.51) |
| Presence of hides in the household | 6(12.0) | 7(3.5) | 1.32 (0.19, 2.46) | 0.77 (-0.65, 2.19) |
| Owned animals | 27(54) | 83(41.5) | 0.5 (-0.12, 0.13) | 0.34 (-0.36, 1.04) |
| Meat trader | 4(8.0) | 1(0.5) | 2.85 (0.63, 5.06) | 2.93 (0.23, 5.64) |
| Cattle keeper | 2(4.0) | 14(7.0) | -0.6 (-2.11, 0.92) | -1.4 (-3.56, 0.76) |
Discussion
This investigation confirmed an anthrax outbreak among humans in Kabira sub-county, Kyotera District with both cutaneous and gastrointestinal clinical signs and symptoms observed. The study found that male were more affected than women, with the majority case-patients being managed by traditional healers. There was evidence that the outbreak was caused by Bacilius anthracis and was spread through handling and consuming meat from cattle that died suddenly on local farms.
Cutaneous cases were more than the gastrointestinal, these findings were consistent with other studies(13)(14). Since hands are used for handling meat, they are at higher risk of developing abrasions, bruises, and cuts, thereby creating a route of entry for the anthrax spores. The findings also agree with a study by Chakraborty A. et al (2012) on anthrax outbreaks in Bangladesh which indicated that fewer gastrointestinal cases were due to cooking meat for a long period (15). The process of cooking destroys the Bacillius anthracis thus reducing the virulence and chances of causing the disease.
The study found that males were more affected than females, the findings were in agreement with a study that revealed males are most likely to be engaged in exposures to animal carcasses such as slaughter, skinning, transportation, and selling of meat from cattle that have died of anthrax(6).
The case fatality rate of 19% was high, this finding was contrary to other studies that had recorded low fatality cases in anthrax outbreaks(16)(17). This was probably due to failure or delay to seek appropriate care especially during the initial stage of the outbreak as many people believed that witchcraft was the cause of the disease and thought care from traditional healers in shrines(18).
The onset of symptoms in case-patients in the 11 villages coincided with the slaughtering and selling of the meat from the affected farms, this indicates that persons who ate or had contact with the dead cattle had an increased risk of cutaneous and Gastrointestinal Anthrax. Previous studies of anthrax outbreaks in Uganda also found an association of anthrax to handling and eating of meat from cattle that died suddenly before slaughter(19)(20)(21). This investigation demonstrated that consumption and contact with meat from the cattle that died suddenly resulted in the Anthrax outbreak. This information was utilized by Kyotera District to implement immediate interventions to limit the spread of infection and stop the outbreak.
Study limitations
Some cases may not have been line-listed during case finding given that many people were managed in secret shrines by traditional healers and we could not be allowed to access them. This likely lead to an under estimation of the magnitude of the outbreak. The presentation of gastrointestinal anthrax is similar to other diseases such as ulcero glandular tularemia and bubonic plague. Additionally, some anthrax cases only develop mild symptoms and may not know that they have anthrax, so the likelihood of missing them out during case finding is high hence the possible under estimation of the magnitude of this outbreak.
Conclusion
Eating and handling meat from cattle that died suddenly was the cause of the Anthrax outbreak in Kabira Sub County, Kyotera District. We recommended the inspection of all cattle before slaughter and vaccination of livestock against B. anthracis. We also recommended continued risk communication and community engagement sessions regarding Anthrax throughout the District.
Public health actions
Following our recommendations, the task force immediately announced an animal quarantine for 14 days. Additionally, the affected communities were sensitized to create Anthrax awareness. Farm managers were also supported to properly dispose off animal carcass whenever an animal died on the farm.
Conflict of interest
The authors declare no conflict of interest
Author contribution
LT, DK, BK, RM, DK, ARA conceived and designed the study. LT, DK, AK, BK, RM, DK, ARA contributed to data collection, cleaning and analysis. AK, EN, AB, participated in coordination of laboratory work. LT, DK, AK, EN, BK, RM, DK, ARA took lead in developing the bulletin. All authors contributed to the final draft of the bulletin. All the authors read and approved the final bulletin.
Acknowledgements
We thank the ministry of health for permitting us to respond to this outbreak. We thank the Kyotera district local government for granting permission and overall guidance to the team.
Copyright and licensing
All the materials in the Uganda Public Health Bulletin is in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Kamal SM, Rashid AKMM, Bakar MA, Ahad MA. Anthrax: an update. Asian Pac J Trop Biomed. 2011;1(6):496–501.
- Sweeney DA, Hicks CW, Cui X, Li Y, Eichacker PQ. Anthrax infection. Am J Respir Crit Care Med. 2011;184(12):1333–41.
- Range RWH. Anthrax in free-ranging wildlife. Fowler’s Zoo Wild Anim Med Curr Ther (Miller, RE Fowler, ME eds), Elsevier Heal Sci St Louis. 2011;98.
- Doganay M, Demiraslan H. Human anthrax as a re-emerging disease. Recent Pat Antiinfect Drug Discov. 2015;10(1):10–29.
- Moayeri M, Leppla SH, Vrentas C, Pomerantsev AP, Liu S. Anthrax pathogenesis. Annu Rev Microbiol. 2015;69:185–208.
- Organization WH, Epizootics IO of. Anthrax in humans and animals. World Health Organization; 2008.
- Cieslak TJ, Eitzen Jr EM. Clinical and epidemiologic principles of anthrax. Emerg Infect Dis. 1999;5(4):552.
- Doganay M, Metan G, Alp E. A review of cutaneous anthrax and its outcome. J Infect Public Health. 2010;3(3):98–105.
- Gachohi J, Bett B, Otieno F, Mogoa E, Njoki P, Muturi M, et al. Anthrax hotspot mapping in Kenya support establishing a sustainable two-phase elimination program targeting less than 6% of the country landmass. Sci Rep. 2022;12(1):21670.
- Coffin JL, Monje F, Asiimwe-Karimu G, Amuguni HJ, Odoch T. A One Health, participatory epidemiology assessment of anthrax (Bacillus anthracis) management in Western Uganda. Soc Sci Med. 2015;129:44–50.
- Musewa A, Mirembe BB, Monje F, Birungi D, Nanziri C, Aceng FL, et al. Outbreak of cutaneous anthrax associated with handling meat of dead cows in Southwestern Uganda, May 2018. Trop Med Health. 2022;50(1):1–8.
- Statistics UBO. The national population and housing census 2014-main report. Kampala Uganda Bur Stat. 2016;
- Gombe NT, Nkomo BMM, Chadambuka A, Shambira G, Tshimanga M. Risk factors for contracting anthrax in Kuwirirana ward, Gokwe North, Zimbabwe. Afr Health Sci. 2010;10(2):159–64.
- Patassi AA, Saka B, Landoh DE, Agbenoko K, Tamekloe T, Salmon-Ceron D. Detection and management of the first human anthrax outbreak in Togo. Trop Doct. 2016;46(3):129–34.
- Chakraborty A, Khan SU, Hasnat MA, Parveen S, Islam MS, Mikolon A, et al. Anthrax outbreaks in Bangladesh, 2009–2010. Am J Trop Med Hyg. 2012;86(4):703.
- Opare C, Nsiire A, Awumbilla B, Akanmori BD. Human behavioural factors implicated in outbreaks of human anthrax in the Tamale municipality of northern Ghana. Acta Trop. 2000;76(1):49–52.
- Takawira E, Charimari L, Tshimanga M. An outbreak investigation of Anthrax in Rushinga District of Mashonaland Central Province in Zimbabwe. Harare: Zim-FETP. 2004;
- Kracalik I, Malania L, Tsertsvadze N, Manvelyan J, Bakanidze L, Imnadze P, et al. Human cutaneous anthrax, Georgia 2010–2012. Emerg Infect Dis. 2014;20(2):261.
- Monje F, Kisaakye E, Ario AR, Eurien D, Ntono V, Kadobera D, et al. Anthrax Outbreaks among Domestic Ruminants Associated with Butchering Infected Livestock and Improper Carcass Disposal in Three Districts of Uganda, 2016-2018. 2020;
- Aceng FL, Ario AR, Alitubeera PH, Neckyon MM, Kadobera D, Sekamatte M, et al. Cutaneous anthrax associated with handling carcasses of animals that died suddenly of unknown cause: Arua District, Uganda, January 2015–August 2017. PLoS Negl Trop Dis. 2021;15(8):e0009645.
- Kibwika B, Namulondo E, Aanyu D, Nuwamanya Y, Rek J, Kiza D, et al. Anthrax outbreak associated with handling and consuming meat from animals that died suddenly, Ibanda District, Uganda, May 2023.


Comments are closed.