Rubella Outbreak among Vaccinated Children Propagated by Attending School X, Nakaseke District, Uganda, January 2020
Quarterly Epidemiological Bulletin : April to June 2020 Volume 5 Issue 2 Article No. 8
Authors: Irene B. Kyamwine1*, Maureen Katusiime1, John Kamulegeya1, Benon Kwesiga1, Alex R. Ario1, Julie Harris2
1Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda,
2Centers for Disease Control and Prevention, Kampala, Uganda
Summary
On 10 January 2020, the Uganda National Expanded Program on Immunization was notified of five patients testing IgM-positive for rubella in Nakaseke District, Uganda. We investigated to determine the scope of the outbreak, identify transmission-related exposures, and recommend control and prevention measures. We defined a suspected case as fever and maculopapular rash, or suspicion of measles/rubella by a healthcare worker, in a resident or visitor of Semuto sub-county, Nakaseke District from 1 October 2019 to 2 March 2020. A confirmed case was a suspected case positive by rubella-specific IgM. We reviewed health facility records and conducted active community case-finding. In a case-control study, we compared potential exposures between 18 case-patients and 72 asymptomatic village- and age-matched controls. We identified 21 suspected case-patients, five confirmed (no deaths). The overall sub-county attack rate (AR) was 7.8/10,000. Males (AR=10/10,000) were more affected than females (AR=4.8/10,000). All case-patients were from a single parish. Seventeen (94%) case-patients received the MR vaccine in October 2019, a median of 61 days (range: 8-96) before symptom onset. The vaccine lot used in the affected parish was also used in other unaffected sub-counties. Vaccination was not associated with illness (OR(M-H)=3.0, CI: 0.41-22). Eight (44%) case-patients and 12 (17%) control-persons attended School X (OR(M-H)=3.9, CI: 1.2-12). We concluded that the recent rubella vaccination was ineffective in preventing this outbreak. This outbreak was likely propagated by patients mixing with other children attending School X. We recommended intensifying sensitization of communities and schools on rubella transmission and prevention and evaluation of the recent MR vaccine potency, vaccine storage and cold chain before more of the same vaccine is administered.
Background
Rubella is an acute viral infection transmitted by airborne droplets. It is less contagious than measles. The average incubation period for rubella is 14 days but can range from 12–23 days (1). Rubella causes a mild disease characterized by a rash, fever, arthritis and joint pain among children and adults(2). Rubella is diagnosed by detection of rubella specific IgM or Ig G antibody, positive viral culture for rubella or detection of rubella virus by polymerase chain reaction (PCR) from nasal, blood, throat, urine and cerebrospinal fluid specimens (1). Rubella infection is vaccine preventable.
Following vaccination Ig M and Ig G antibodies develop within 2 weeks. However, I g M antibodies quickly fade away to almost undetectable after 2 months of vaccination (1). Despite the availability of the rubella containing vaccine since 1969 Uganda introduced a rubella‐containing vaccine into the routine schedule in October 2019 following measles-rubella outbreaks in the country in 2018 (1)(3). In Uganda, all suspected measles cases tested for anti-measles are also tested for antirubella immunoglobulin M (IgM) antibodies (4).
On 10 January 2020, Uganda Ministry of Health (Uganda National Expanded Program on Immunization) received notification of 5 patients testing Rubella IgM positive. We investigated to determine the scope of the outbreak, exposure risk factors, estimate vaccine effectiveness and vaccination coverage, and guide evidence-based control measures.
Methods
We defined a suspected case as a fever and maculo-papular rash, or a health care worker suspicion of measles in a resident or visitor of Semuto sub-county, Nakaseke District from 1 October, 2019 onwards; a confirmed case as a suspected case with a positive blood test for rubella-specific Ig M. We reviewed health facility records and conducted active case finding. We performed descriptive analysis of the cases and developed hypotheses. We conducted a case control study to identify exposures for transmission. We estimated rubella vaccination coverage (VC) using the percent of control-persons vaccinated assuming that the controls were representative of the general population.
Results
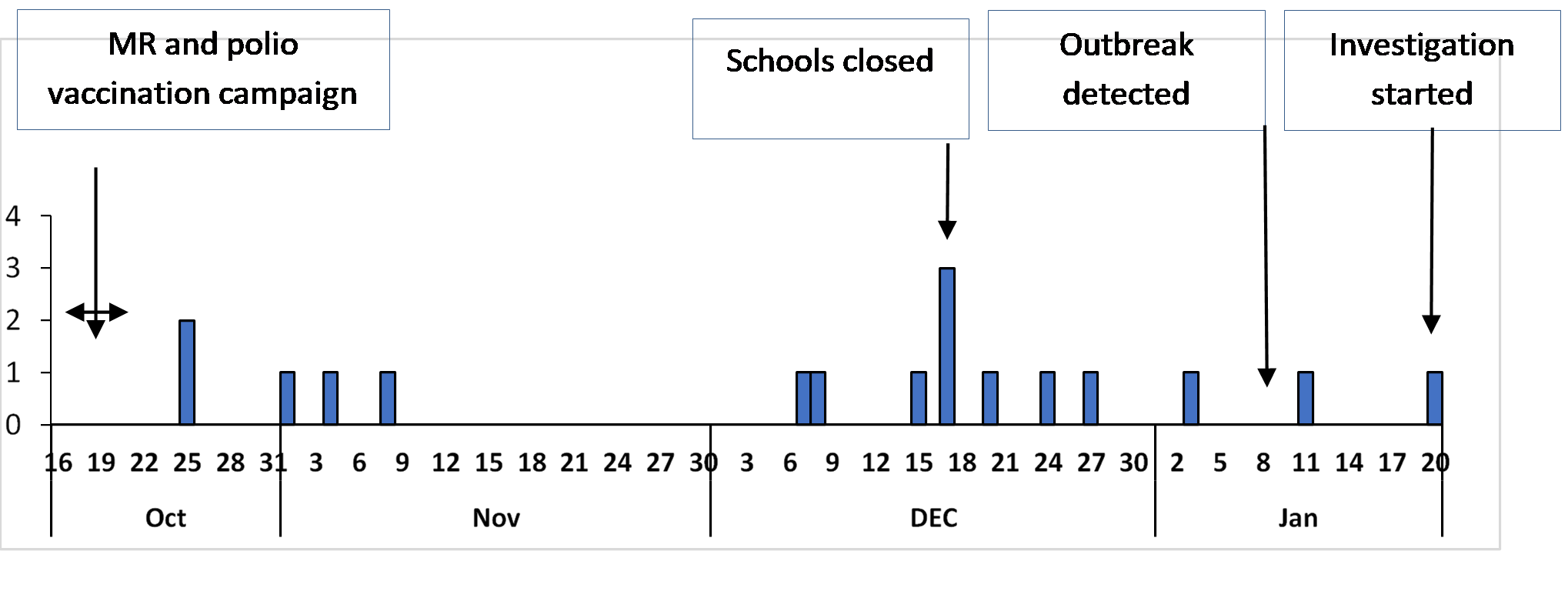
We identified 21 suspected cases in Semuto sub-county, 5 of whom were confirmed. The sub-county attack rate [AR] was 7.8/10,000 persons and no death. The epidemic curve shows a propagated outbreak (Figure 1).
Median age was 5 years (Range: 1-15 years). Age-group 9 months-<15 years had the highest proportion of cases (20), >15 years had only one case and the age-group <9 months did not have any cases. Males (AR: 10/10,000) were more affected than females (AR: 4.8/10,000).
Segalye parish was the only parish affected in Semuto sub-county. Nvunaanwa (20 cases) and Kalege (1 case) were the only villages affected in the parish. Attending school X was associated with rubella infection among 8 (44%) case-patients compared to 12 (17%) control-persons (OR(M-H)=3.9, CI: 1.2-12), (Table 1). The VC, estimated by the percent of control-persons who had a history of rubella vaccination, was 83%.
Table 1: Exposure status among Cases and Controls in a rubella outbreak, Semuto sub-county, Nakaseke District, January 2020
| Exposure | Number Exposed | Percent Exposed | Odds Ratio | 95%
CI |
||
| Cases | Controls | Cases | Controls | |||
| Attending school X | 8 | 12 | 44 | 17 | 3.9 | 1.2-12* |
| Contact with a person with febrile rash | 13 | 11 | 72 | 15 | 21 | 4.2-109* |
| Rubella Vaccination | 17 | 60 | 94 | 83 | 3.0 | 0.41-22 |
| Visiting public water source | 12 | 53 | 67 | 74 | 0.58 | 0.14-2.4 |
| Attending religious gatherings | 15 | 43 | 83 | 60 | 3.1 | 0.91-11 |
* Statistically significant OR
Discussion
Our investigation showed that attending school X was associated with rubella infection. The continuous transmission of rubella was likely propagated by school children continuing to attend school during illness, hence spreading the infection to others in class or during play time through sneezing and coughing at school. This finding is consistent with other studies conducted in Ethiopia and Chile where institutional outbreaks of rubella were registered (5,6).
Our finding is also biologically plausible considering that rubella is spread through respiratory secretions. Isolation of the case-patients at home could have stopped the spread of rubella to school going children (7). Therefore, during rubella outbreaks, schools and communities should be advised to isolate children with fever and rash from other children.
We also, found that children below the age of 15 years were the most affected. This finding is similar with earlier studies in Zimbabwe, Ethiopia and Kenya. Chimhuya, et al and Mitiku, et al both demonstrated that over 90% of the rubella cases were children <15 years (8–10). The mean age in our study was 6 years which is similar with findings in Zimbabwe (11). The high incidence of rubella cases among younger children could be attributed to lack of immunity that the older people may have acquired from infection. This therefore, calls for intensifying the MR vaccination to ensure that all children are vaccinated.
Contrary to other rubella outbreaks, in this investigation almost all the cases were vaccinated with rubella vaccine. However, the rubella infection acquired after vaccination cannot be passed on to other people hence the vaccine could not have been the cause of this outbreak (12). Rubella could have occurred among vaccinated children due to vaccine failure.
The outbreak could have occurred because the children did not mount immunity against rubella which would have interrupted transmission. In study by US CDC in 1992-94, 8% of the vaccinees were found to lack serologic evidence of immunity to rubella (CDC, unpublished data) (13) which could be the case in our outbreak.
Therefore, sero-epidemiologic studies of IgG levels are needed to assess rubella immunity among the vaccinated population. This outbreak also highlights the importance of a thorough epidemiologic and laboratory investigation of suspected cases of measles and rubella, regardless of vaccination status, as well as the need for active surveillance.
Conclusion
The recent rubella vaccination was ineffective in preventing this outbreak. This rubella outbreak was associated with contact with a case and likely propagated at School X. Ministry of Health should evaluate the recent MR vaccine potency, vaccine storage, and cold chain records before more of the same vaccine is administered. We also, recommended intensifying sensitization of communities and schools on rubella transmission and prevention.
References
- rubella.pdf [Internet]. [cited 2020 Feb 10]. Available from: https://www.cdc.gov/vaccines/pubs/pinkbook/downloads/rubella.pdf
- manual_diagnosis_lab_mea_rubella.pdf.
- Statement from Uganda’s Minister of Health on the National Measles-Rubella and Polio Immunisation Campaign 2019 – Uganda [Internet]. ReliefWeb. [cited 2020 Feb 11]. Available from: https://reliefweb.int/report/uganda/statement-uganda-s-minister-health-national-measles-rubella-and-polio-immunisation
- Tushabe P, Bwogi J, Abernathy E, Birungi M, Eliku JP, Seguya R, et al. Descriptive epidemiology of rubella disease and associated virus strains in Uganda. J Med Virol. 2020 Mar;92(3):279–87.
Reference this Article as below
Irene B. Kyamwine1*, Maureen Katusiime1, John Kamulegeya1, Benon Kwesiga1, Alex R. Ario1, Julie Harris2 Rubella Outbreak among Vaccinated Children Propagated by Attending School X, Nakaseke District, Uganda, January 2020. Kampala Uganda National Institute of Public Health. 2020 June 30th. Available from:https://uniph.go.ug/rubella-outbreak-among-vaccinated-children-propagated-by-attending-school-x-nakaseke-district-uganda-january-2020.


Comments are closed.