Sustained Vigilance, Preparedness, and Response to All Public Health Emergencies amidst COVID-19 Pandemic
Quarterly Epidemiological Bulletin : April to June 2020 Volume 5 Issue 2 Article No. 7
By Sandra Nabatanzi
Uganda Public Health Fellowship Program, Kampala, Uganda
Introduction
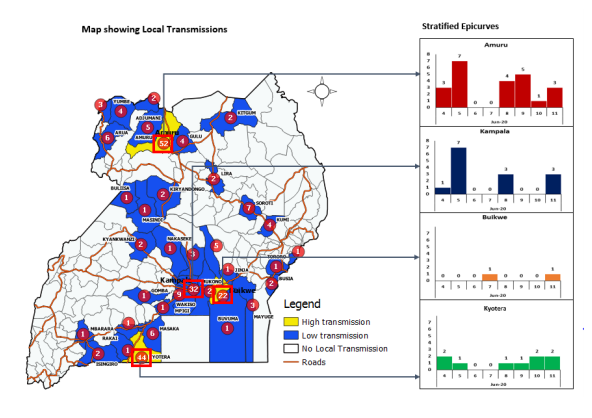
The COVID-19 pandemic has disrupted economies not only in Uganda but the entire World. The health system too has been affected. In Uganda, there were 685 cumulative COVID-19 cases as of 13 June 2020 (1). Unfortunately, there have been 234 community cases reported in 33 districts despite stringent measures put in place by Government of Uganda to avoid spread of COVID-19. (Figure 1). Additionally, 27 health workers had also been infected by COVID-19 but no deaths reported.
During the COVID-19 Pandemic, the number of malaria cases reported at the health facilities has increased by 56% between January and April 2020. Over 70 districts have experienced surges in malaria cases. Health facility deliveries have decreased by 10% while antenatal care (ANC) 4
attendance decreased by 7% between March and April 2020 compared to the same period, last year. The immunization coverage for DPT-1, DPT-3, Polio 3, Measles, and PCV-3 dropped from December 2019 and has remained below the target of 95%. The low reporting rate may have led to the reduction in coverage of immunization during the same period. During the month of March, immunization coverage levels were below 70%. Between February and March 2020, there was a 3% reduction in the number of HIV tests conducted. March had the lowest number of HIV tests conducted this quarter. This may partly be attributed to the movement restrictions that have affected both health providers and patients. Testing yield reduced to 2.4% in March compared to 3.0% of the previous month.
The above identified gaps among many others are possibly due to the effects of COVID-19 on the health care system. A strained health care system increases Uganda’s vulnerability to suffer from other public health emergencies including Cholera, Measles, other immunizable preventable disease, Crimean Congo Hemorrhagic Fever among other diseases of epidemic potential.
In 2020, Uganda has so far reported public health emergencies of COVID-19, West Nile Virus Fever, Crimean Congo Haemorrhagic Fever, Rift Valley Fever, Yellow Fever, Cholera, Rubella, Measles, and floods (Table 1).
| Table 1: Public Health Emergencies in Uganda, January – June 2020Dates | Location | PHE | Cumulative | Confirmed | Deaths |
| 04Mar20 | Moyo | West Nile Virus Fever | 01 | 01 | 00 |
| 31Mar20 | Uganda | COVID-19 | 724 | 724 | 00 |
| 10Feb20 | Kampala | Rift Valley Fever | 01 | 01 | 00 |
| 28Feb20 | Kiboga | Rift Valley Fever | 01 | 01 | 01 |
| 21Jan20 | Kagadi | Crimean Congo Hemorrhagic Fever | 01 | 01 | 00 |
| 10Dec19 | Buliisa | Yellow Fever | 24 | 03 | 01 |
| 21Jan20 | Moyo | Yellow Fever | 10 | 04 | 06 |
| 07Feb20 | Maracha | Yellow Fever | 01 | 00 | |
| 20Jan20 | Busia | Cholera | 10 | 01 | 00 |
| 09Jan20 | Nakaseke | Rubella | 05 | ||
| 13Jan20 | Multiple districts | Measles | |||
| 27Apr20 | Moroto | Cholera | 377 | 00 | |
| 22May20 | Nabilatuk | Cholera | 419 | 10 | 00 |
In November 2019, the Ministry of Health conducted a country wide mass measles-rubella vaccination campaign in order to protect susceptible individuals, interrupt transmission, and protect against measles outbreaks in Uganda. This campaign was successful with a coverage of 103%. However, the number of measles cases reported in 2020 is gradually increasing as indicated (Figure 2). The increasing cases call for an urgent need to intensify routine measles vaccination in the country.
Figure 2: Trends of suspected measles cases in Uganda, 2020
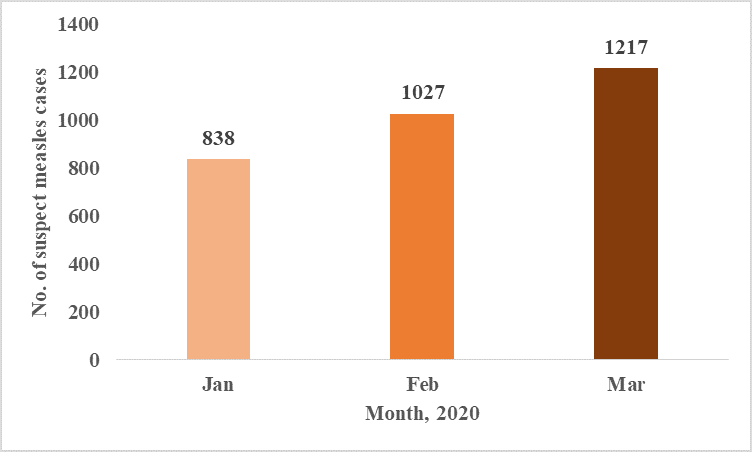
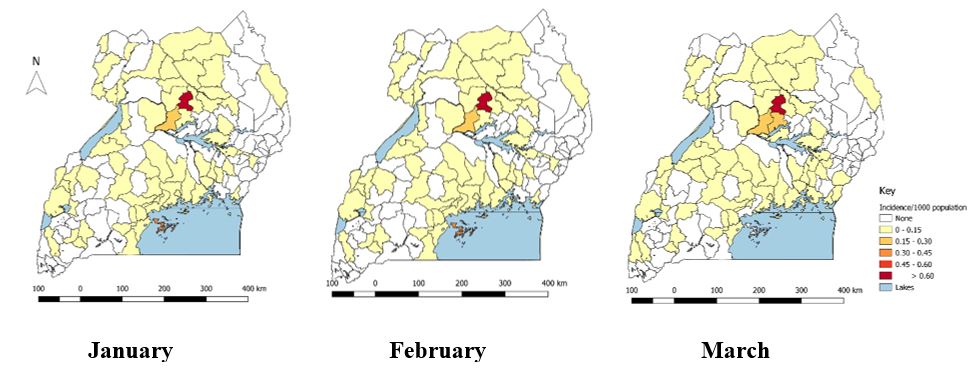
The overall cumulative incidence of suspected measles in Uganda was 9/1,000 population from January to March 2020. The most affected district was Kole District with a cumulative incidence of 2.1/1,000, followed by Apac (0.5), Kalangala (0.3), Kwania (0.3), Gulu (0.3) Obwongi (0.2). Iganga (0.2) and Lamwo (0.2). Over 85/135 districts have reported suspected measles cases in the months of January – March 2020 (Figure 3).
Neighboring countries like the Democratic Republic of Congo continue to battle with the biggest outbreak of Measles ever recorded. On 1 June 2020, the DRC also reported a new EVD outbreak in the Equateur Province. The 11th propagated EVD that affected Ituri and North Kivu, DRC and spilled to Uganda in June 2019 is not linked to current ongoing outbreak in Equateur Province. As 9 June 2020, a total of 12 cases and 8 deaths have been reported in Equateur Province (2).
Although the continuous occurrence of outbreaks of emerging and re-emerging infectious diseases in Uganda is likely primarily due to increased human interaction with forests, caves, and animals, geographic location in filovirus, meningitis, and yellow fever zones, effects of climate change – heavy rains and flooding, conflicts and population displacement in the Great Lakes region, and increased international movement of people among others, the effects of COVID19 on the health care system further increases Uganda’s vulnerability to outbreaks. There is critical need for enhanced vigilance for all PHEs during response to the COVID-19 Pandemic.
How can we maintain capacities built and vigilance to other PHEs amidst response to COVID-19?
Vigilance to all PHEs is critical and can be maintained through 1) Integrating preparedness and response activities for COVID-19 with all other emergencies; 2) Ensuring heightened surveillance and reporting in all districts; 3) Verifying all rumors and alerts and investigating all outbreaks in the country; 4) Decentralizing response mechanisms to district level to ensure efficiency; 5) Use COVID-19 as an opportunity to strengthen capacities to respond to PHEs at all administrative levels; and finally strengthen routine immunization by minimizing missed opportunities for vaccination at health facilities. Currently, Uganda National Expanded Programme on Immunization has encouraged District Health Officers to continue with static immunization at health facilities amidst COVID-19 Pandemic. However, due to the interference with immunization interventions in schools and communities (outreaches), the programme is developing a post recovery plan that will involve mass immunization of the highly affected pathogens.
Conclusion
Despite the stretched resources both human and financial, it is critical to integrate and decentralize response to other Public Health Emergencies with COVID-19. This will in turn enable quick detection and timely response which will avert deaths caused by other outbreaks aside COVID-19. The huge numbers of individuals affected will also cripple the fragile health system. Hence, it is important to be on high alert, rapidly detect, and respond to PHEs in the country.
References
- Ug_COVID-19_SitRep#119.pdf [Internet]. [cited 2020 Jun 22]. Available from: https://veoci.com/veoci/p/w/f/lz9vtf7eg84fnzkd/Ug_COVID-19_SitRep%23119.pdf
- SITREP_EVD_DRC_20200610-eng.pdf [Internet]. [cited 2020 Jun 16]. Available from: https://apps.who.int/iris/bitstream/handle/10665/332320/SITREP_EVD_DRC_20200610-eng.pdf
Read and download full pdf below;


Comments are closed.