Risk factors associated with typhoid intestinal perforations during a large outbreak of typhoid, Kampala Uganda, 2015
Summary
Between January-June, 2015, a large typhoid outbreak occurred in Kampala, causing 10,230 suspected infections. An increase in the number of intestinal perforations (TIP) was observed by surgeons during the 2015 outbreak period. In this study, we ascertained if there was an increase in the number of TIP and identified risk factors associated with TIPs during a large outbreak of typhoid fever that occurred in Kampala in 2015. A sharp increase in the number of both TIPs and other IPs was observed between January to March 2015. Delay in seeking treatment, self medication, not having heard of typhoid before and not being aware of the typhoid outbreak increased the risk of TIPs. We recommended active community case finding for early and appropriate treatment, health education about typhoid fever and TIPs, and raising awareness among physicians about the risk of perforations during future typhoid outbreaks.
INTRODUCTION
Typhoid Intestinal Perforation (TIP) is one of the life-threatening complications of typhoid fever.
Typhoid intestinal perforation refers to non traumatic intestinal perforation in the terminal ileum diagnosed as due to typhoid fever.
Although typhoid fever remains a serious public health problem in developing countries, it is poorly understood com- pared to other regions (1).
There is limited information about modifiable risk factors for TIPs in Uganda and Africa at large.
METHODS
We defined TIP case as a physician-diagnosed typhoid patient with non-traumatic terminal ileum perforation. We reviewed medical records from Jan 2013-Dec 2015 at 5 major hospitals in Kampala which performed surgeries. In a case- control study, we compared potential risk factors for TIP among cases and controls; controls were those with typhoid diagnosis by TUBEX, culture, or physician but with no TIP, matched to cases by age, sex and residence. We used conditional logistic regression to assess risk factors and control for confounding
Results
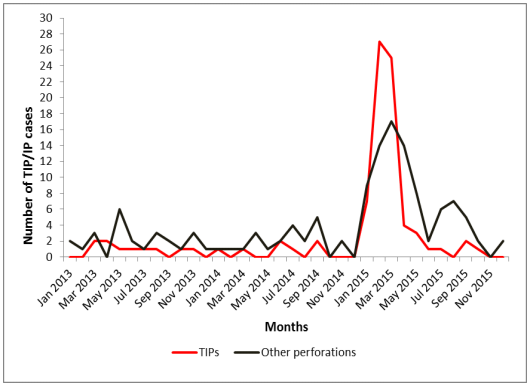
Of the 88 TIP cases identified, 77% (68/88) occurred during the outbreak period. Both TIPs and other IPs sharply increased in January and peaked in March, coinciding with the outbreak period (Figure 1). The prevalence of TIPs and other IPs during the outbreak period was each estimated to be 5
TIPs/100,000 population (68 TIPs, 70 other IPs/1,516,210). The case fatality rate for TIPs was 10% (7/68). Compared with 29% (13/45) of cases and 63% (86/137) of controls who sought treatment with- in 3 days of onset, 42% (19/45) of TIP cases and 32% (44/137) of controls sought treatment after 4-9 days (ORadj=3.0, 95% CI=1.3-6.3); 29% (13/45) of cases and 5.1% (7/137) of controls sought treatment after ≥10 days (ORadj=12, 95%CI=4.1-37). Additionally, 57% (26/46) of cases and 31% (43/137) of controls had self-medication (ORadj=2.9, 95%CI=1.4-6.2); 36% (25/39) of cases and 18% (116/142) of controls had not heard about ty- phoid (ORadj=2.5, 95%CI=1.1-5.5); and 59% (23/39) of cases and 25% (35/142) of controls had not heard about the typhoid outbreak in Kampala (ORadj=4.9, 95%CI=2.0-12).
DISCUSSION
In this study conducted to ascertain if there was an increase in the number of TIPs and identify risk factors associated with TIPs during the 2015 typhoid outbreak in Kampala, we found that an outbreak of perforations (both TIPs and other perforations) occurred and an association was observed between TIP and duration of before seeking treatment. The risk of developing TIPs increased with increasing duration before formal treatment. Self medication, not having heard about typhoid infection before, and not having heard about the typhoid out- break in Kampala City were also strongly associated with developing TIPs. The sharp increase in the number of cases observed in this study coincides with the 2015 typhoid outbreak period in Kampala. The observed increase in the number of IPs in other areas of the gut (and around the same period of time as the TIP) implies that these perforations might have been as a result of typhoid fever. Intestinal perforations in other sites of the gut such as
upper ileum, caecum and jejunum have been re- ported in other studies (2, 3). One of the major findings in our study was a highly significant association of TIPs and longer duration before seeking medical care. Up to 60% of patients with TIP were hospitalized after seven days since onset of symptoms. This is in agreement with findings of studies mainly conducted outside Africa (4, 5). Self medication, which involves the use of medicinal products to treat self recognized disorders or symptoms without a medical prescription (6) is a common practice in developing countries and it was significantly associated with TIP in our study. Self medication may lead to potential risks such as incorrect self-diagnosis, , inappropriate choice of therapy and inadequate dosing of antibiotics (6).
It is possible that being on inappropriate therapy may have contributed to delay in seeking medical care from qualified medical professionals which in turn increased the risk developing TIP.
In conclusion,
A sharp increase in the number of both TIPs and other IPs was observed between January 2015 and March 2015. Delay in seeking treatment, self medication, not having heard of typhoid before, not being aware of the typhoid outbreak increased the risk of TIPs.
Recommendation
We recommended active community case finding for early and appropriate treatment, health education about typhoid fever and TIPs, and raising awareness among physicians about the risk of perforations during future typhoid outbreaks.
The study presents two public health implications. As noted above, limited information about typhoid fever and the typhoid outbreak, and delay in seeking health care were strongly associated with TIPs. This suggests that we have an opportunity to reduce the burden of TIPs if only we improve access to care and management by ensuring appropriate and prompt antibiotic use and putting in place better surgical facilities.
References
1. Wain J, Hendriksen RS, Mikoleit ML, Keddy KH, Ochiai RL. Typhoid fever. Lancet (London, England). 2015;385(9973):1136 -45.
2. Ekenze SO, Ikefuna AN. Typhoid intestinal perforation under 5 years of age. Annals of tropical paediatrics. 2008;28(1):53-8.
3. Van der Werf TS, Cameron FS. Typhoid perforations of the ileum. A review of 59 cases, seen at Agogo Hospital, Ghana, between 1982 and 1987. Tropical and geographical medicine. 1990;42(4):330-6.
4. Butler T, Knight J, Nath SK, Speelman P, Roy SK, Azad MA. Typhoid fever complicated by intestinal perforation: a persisting fatal disease requiring surgical management. Rev Infect Dis. 1985;7(2):244-56.
5. Van Basten JP, Stockenbrugger R. Typhoid perforation. A review of the literature since 1960. Trop Geogr Med. 1994;46(6):336-9.
6. WHO Guidelines for the regulatory assessment of Medicinal Products for use in self-medication. 2000

