
Rift Valley Fever Outbreak, Kiruhura District, Uganda, June 2021
Authors: Hildah Tendo Nansikombi1*, Alex Ndyabakira1, Irene Kyamwine1, Benon Kwesiga1, Fred Monje2, Luke Nyakahurura3, Julie Harris4; Institutional affiliations: 1Uganda Public Health Fellowship Program, Kampala Uganda, 2 Ministry of Agriculture, Animal industry and Fisheries, Entebbe, Uganda, 3Uganda Virus Research Institute, Entebbe, Uganda, 4 US Centers for Disease Control and Prevention, Kampala, Uganda; *Corresponding author: Email: hnansikombi@musph.ac.ug, Tel: +256777570470
Summary
Rift valley fever (RVF) is an endemic viral zoonosis in Uganda, where there are sporadic outbreaks. On May 14, 2021, a 19-year-old female from Kasaana village, Kiruhura District died; reverse-transcriptase polymerase chain reaction (RT-PCR) was positive for RVF. We investigated to determine the magnitude of the outbreak, source of infection, and recommend evidence-based control measures.
A confirmed case was defined as detection of RVF virus nucleic acid by RT-PCR or serum IgM/IgG antibodies by enzyme-linked immunosorbent assay (ELISA) in a resident of/visitor to Kasaana village from April 24-June 24, 2021. We tested blood samples from 25 persons (3 with RVF symptoms, 2 neighbors of the index case, and 20 randomly-selected villagers) using RT-PCR or ELISA, and 57 livestock (33 randomly-selected cows and 24 goats) from 4 village farms reporting any animals with RVF symptoms) by ELISA. We collected data on demographics, history of RVF symptoms, and animal-related activities. We characterized cases epidemiologically.
We identified 9 confirmed human cases in Kasaana village (2 RT-PCR-positive, 2 IgM/IgG-positive, 2 IgM-positive; 3 IgG-positive). One died (case fatality rate=11%). Five (56%) were female; median age was 20 years (range, 15–60 years). All cases kept cows and goats. Two case-patients reported headache, fever, and hemorrhage. The index case-patient, who milked cows on her family farm, had hemorrhagic symptoms consistent with RVF starting 1 week before death. She presented to five health facilities during that week but was only diagnosed after death. Three (9%) cows and five (21%) goats were IgM-seropositive for RVF.
This RVF outbreak likely resulted from contact with infected animal products. Earlier diagnosis might have prevented the index case-patient’s death. We conducted health education among Kasaana villagers, and recommended training of health workers at facilities within the region to emphasize the importance of early diagnosis of haemorrhagic fevers
Background
Rift Valley Fever (RVF) is a zoonotic disease that primarily affects animals but can also affect humans. Human infections result from contact with the blood organs, products of infected animals, and mosquito bites [1]. To date, no human-to-human transmission of RVF virus has been documented. The incubation period for RVF varies from 2 to 6 days [2]. Interepidemic virus maintenance is thought to occur either transovarially in Aedes species mosquitoes or through cycling of low-level transmission between domestic livestock or wild ungulates [3]. After periods of heavy rainfall, Aedes mosquitoes rapidly emerge, resulting in extensive amplification of the virus through infection of livestock [2, 4].
Presentation of RVF in animals can vary among species with a range of clinical severity. Livestock particularly cattle, sheep, and goats are highly susceptible to RVF and present with symptoms of fever, loss of appetite, weakness, low milk production, nasal discharge, vomiting, and diarrhea [5, 6]. During large epizootics, “abortion storms”, particularly in goats and cattle, have been reported. High newborn mortality (80–100%) and adult mortality (5–20%) may also be observed in animals [7].
Humans infected with RVF usually have non-specific symptoms. Majority of cases typically have mild, self-limited febrile illness (4). Severe disease occurs in about 2% of the cases and manifests as ocular, meningoencephalitis or hemorrhagic fever with severe jaundice, rhinitis and encephalitis [2]. Among those infected, case fatality rate is about 50% mainly among case-patients who develop hemorrhagic symptoms [5].
Outbreaks of RVF have been reported frequently in East Africa, especially Kenya and Tanzania [2]. The emergence of RVF virus in East Africa resulted in widespread livestock morbidity and mortality, with hundreds of laboratory-confirmed human cases, and likely thousands of asymptomatic human infections going undetected [8]. In Uganda, Rift Valley fever virus was first detected in mosquitos collected in Semliki forest, Western Uganda, in 1944, and has since been detected several times by the Uganda Virus Research Institute (UVRI)[8, 9].
On May 14 2021, UVRI notified the Uganda Ministry of Health (MoH) of a rift valley fever case confirmed by reverse transcriptase polymerase chain reaction (RT-PCR). The case person was a 19-year-old female who had been involved in milking her father’s cows. She presented to six health facilities with bleeding, high grade fever and acute kidney injury for one week. At the sixth facility, a viral hemorrhagic fever was suspected, a blood sample was taken and sent to the UVRI viral hemorrhagic fever (VHF) laboratory for testing. The patient died and later, the blood sample tested positive for RVF virus. We investigated to determine the magnitude of the outbreak, source of infection, and recommend evidence-based control measures.
Methods
Outbreak area
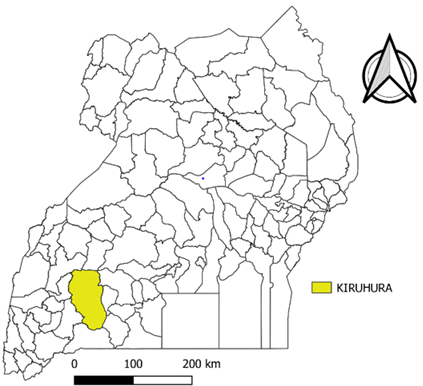
The outbreak was reported in Kiruhura District, located in South western Uganda and part of the Ankole sub region (Figure 1). Animal keeping is the main economic activity in Kiruhura District; every household owns at least a cow or goat. Milk and meat are important food and trade products in this area. However, by the time of the RVF outbreak, there was an ongoing foot and mouth disease outbreak that caused a ban on animal movements and trade of animal products in Kiruhura District from late January 2021.
The outbreak occurred in Kasaana Village, Kinoni Sub-county, Kiruhura District. Kinoni Sub-county had a total of 26 villages and a population of 26,097. Kasaana village, where the study was conducted has a population of 1,157 persons.
Case definition, finding, and environmental assessment
We defined a suspected case as onset of fever with a negative malaria test and at least 2 of any of the following symptoms: headache, muscle pain, dizziness, blurred vision, nausea, vomiting, abdominal pain, diarrhea, unexplained bleeding symptoms in a resident or visitor of Kasaana village from April 24, 2021 to June 24, 2021. A confirmed case was a suspected case plus laboratory confirmation of RFV by either detection of RVF virus nucleic acid by reverse-transcriptase polymerase reaction (RT-PCR), or serum IgM or IgG antibodies by enzyme linked immunosorbent assay (ELISA)
Upon notification regarding the death of a confirmed RVF case from Kiruhura District, we collected additional information on the first case patient from attending clinicians and close family members. We identified more cases through active case finding in Kasaana village. We interviewed cases on their demographics, history of RVF symptoms, and history of interaction with animals.
Laboratory testing
We conducted laboratory testing on both humans and animals using RT-PCR, or enzyme linked immunosorbent assay (ELISA).
We collected blood samples from twenty-five case patients; three were symptomatic, two were neighbours to the index case patient and the other 20 were randomly selected Kasaana villagers. Three case patients were tested using RT-PCR while the other 22 were tested for serum IgM and IgG antibodies for RVF virus by ELISA.
We collected blood samples from 57 animals; 33 cows and 24 goats randomly selected from four village farms reporting animals with RVF symptoms. The animals were tested for IgM antibodies by ELISA.
Environmental assessment
We observed the animals at the village farms and nearby water ponds at the farms. We assessed for the presence of dead animals in Kasaana village, animal/meat transport mechanisms, selling of grilled meat and how meat was prepared before it was sold. We also assessed selling points for milk and meat, asked about animal movement, and trading in the area.
Data analysis
We conducted descriptive analysis. We generated an epidemic curve to describe the outbreak over time, described the characteristics of the affected persons by age, sex and RVF symptoms, and their geographical location.
Ethical considerations
This investigation was in response to a public health emergency and was therefore determined to be non-research. The MoH Uganda through the office of the Director General of Health Services gave the directive and approval to investigate this outbreak. The Office of the Associate Director for Science, CDC/Uganda, also determined that this activity was not human subject research, and its primary intent was public health practice or a disease control activity (specifically, epidemic or endemic disease control activity). We obtained verbal informed consent from case-persons during this investigation and other interviewed community members that were above 18 years, as well as the owners of the animals that were tested. For participants below 18 years of age, we sought verbal assent from their parents or guardians. We ensured confidentiality by conducting interviews in privacy ensuring that no one could follow proceedings of the interview. The questionnaires were kept under lock and key to avoid disclosure of personal information of the respondents to members who were not part of the investigation.
Results
We identified nine case-patients from Kasaana village, Kinoni Subcounty, Kiruhura District; 2 RT-PCR-positive, 2 IgM/IgG-positive, 2 IgM-positive; 3 IgG-positive. Five (56%) were female. Participants’ median age was 20 years (range: 15 – 60 years). Of the nine case patients, one died (CFR= 11%).
Two of the confirmed case persons had symptoms consistent with those of RVF; fever, headache, and vomiting while the others were asymptomatic. Apart from the reported death, the other symptomatic case patients were followed up to recovery.
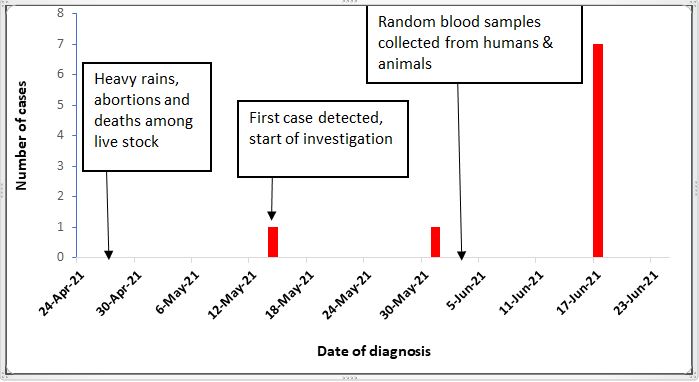
The rift valley fever outbreak began in early May and went on till June 2021. The outbreak began following heavy rainfall in April 2021 (Figure 2). There was evidence of heavy rains due to the many water-filled ponds at the village farms.
Of the 57 animals tested from Kiruhura District, eight (14%) were IgM sero-positive for RVF virus; three (9%) cows and five (21%) goats.
All case persons kept cows and goats; they milked and grazed them. None of the case patients ate meat of any dead animal. Farmers reported that their animals had been having abortions, and young animals on their farms died. Carcasses were disposed in the bushes for dogs to eat. Animal movements and sale of animal products were prohibited in Kiruhura District. There was already an ongoing outbreak of Foot and Mouth Disease in Kiruhura District so there was a ban on animal movement and trade of animal products. The ban had been on since late January 2021.
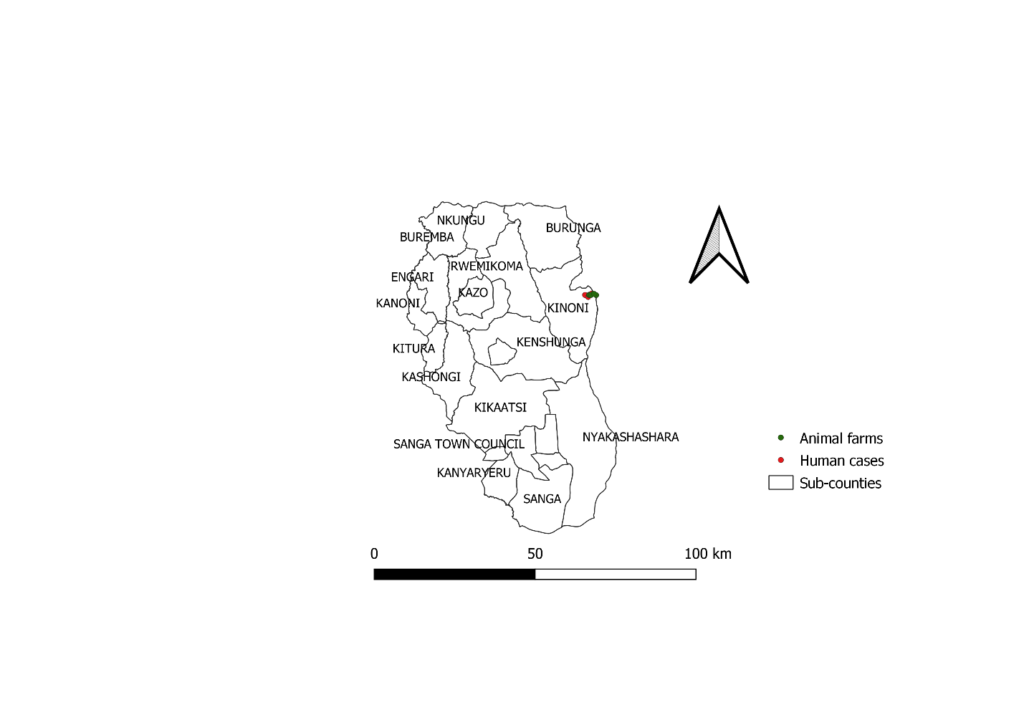
Case-patients were living near each other and the farms with infected animals (Figure 3).
Discussion
The investigation found that nine persons and eight animals were infected with RVF virus in Kasaana village, Kinoni sub-county in Kiruhura District. While most of the human cases were asymptomatic, two had symptoms consistent with RVF including, fever, headache and haemorrhage. In addition, the animal cases at the village farms had typical signs and symptoms of RVF such as abortions and deaths among young ones. Given that all cases kept animals, person, and place descriptive data showed that caring for livestock and living near infected animals are potential risk factors for RVF.
Although symptoms of RVF are usually mild and non-specific, two case persons in this outbreak had typical haemorrhagic symptoms with vomiting blood and bleeding from body orifices, consistent with RVF virus infection as in previous similar studies [2, 7, 10]. These hemorrhagic symptoms should have raised suspicion of a haemorrhagic fever. However, despite these symptoms, the index case patient presented to five health facilities without any health care worker suspecting a hemorrhagic fever until she got to the sixth facility where a blood sample was collected for viral haemorrhagic fever testing before her death. Had the patient had a more virulent and transmissible hemorrhagic fever virus like Ebola, the implication of delayed diagnosis would probably have been worse.
Death among RVF cases is said to occur in about 50% of cases mainly among those who get hemorrhagic symptoms[5]. The index case patient, who died during this outbreak had bleeding from all body openings as it is reported in similar studies [2, 11, 12]. Had the case patient been diagnosed early and provided with supportive care, organ damage and death could have been prevented.
The study reported that all cases were farmers keeping at least a cow or goat which indicates the occupational nature of the disease. Several previous studies have reported high-risk occupations for RVF infection including: abattoir workers, veterinary personnel, and farmers[10, 12, 13]. It was found that farm workers/farmers, animal health workers and abattoir workers or butchers were most affected during an outbreak in South Africa[14]. In Northern Africa, the RVF
outbreak affected shepherds, animal breeders, farmers, and veterinarians which shows the occupational nature of the infection [15].
The environmental assessment revealed that the RVF outbreak occurred shortly after a rainy season. There were many water-filled ponds lying close to homes and farms but without Aedes mosquito larvae. Elsewhere, other countries have reported that majority of RVF outbreaks occur during or immediately after a rainy season because Aedes mosquitoes breed during the rainy seasons [3, 6]. After multiplication in bigger numbers, the mosquitoes transmit RVF virus infection in livestock and sometimes in humans [3, 4].
Findings suggest that RVF infections among animals preceded human infections as noted in previous studies. Establishment of an active animal health surveillance system to detect new cases is essential in providing early warning for veterinary and human public health authorities [5, 6, 11, 12].
Study Limitations
We may have underestimated of the magnitude of the outbreak. Many of the RVF cases never exhibited any signs or symptoms and were less likely to even realize that they were sick. This implies that many cases could have been missed by the healthcare system. In addition, some cases were identified through random testing; we could have missed out on many more.
Conclusion
There was active infection of RVF among residents of Kasaana village although most of them were asymptomatic. Contact with products of infected animals could have been the source of human infection. Early diagnosis and supportive therapy could have prevented the index case patient’s death. This investigation highlights the need for continuous clinician education on the importance of early diagnosis and continuous awareness about viral haemorrhagic fevers in areas where they are endemic.
Public health actions
Mass testing of both animals and humans was conducted in Kasaana and other villages to determine the magnitude of infection. Health education and community sensitization was done extensively in Kasaana village with emphasis on the prevention and control of rift valley fever. Use of insecticide treated mosquito bed nets was encouraged among community members. Animal quarantine was strengthened as the district was already facing foot and mouth disease outbreak.
Recommendations
We recommend training of health workers to improve their alertness about viral haemorrhagic fevers. Animal vaccination against RVF virus should also be conducted.
Acknowledgements
We thank the family of the deceased, the Kiruhura District health team and the residents of Kasaana village for their willingness to support this investigation. We appreciate the Uganda Virus Research Institute and Ministry of Agriculture, Animal Industry and Fisheries for testing all samples and the timely release of results. We acknowledge the Uganda Public Health Fellowship Program for the technical guidance towards making the investigation a success.
References
- WHO, Rift Valley Fever. 2021.
- Mohamed, M., et al., Epidemiologic and clinical aspects of a Rift Valley fever outbreak in humans in Tanzania, 2007. Am J Trop Med Hyg, 2010. 83(2 Suppl): p. 22-7.
- Manore, C. and B. Beechler, Inter-Epidemic and Between-Season Persistence of Rift Valley Fever: Vertical Transmission or Cryptic Cycling? Transboundary and emerging diseases, 2013. 62.
- Rodrigue Simonet, P.N., et al., Diversity and Abundance of Potential Vectors of Rift Valley Fever Virus in the North Region of Cameroon. Insects, 2020. 11(11): p. 814.
- Gerdes, G., Rift Valley fever. Revue scientifique et technique (International Office of Epizootics), 2004. 23(2): p. 613-623.
- Boussini, H., et al., Prevalence of Rift Valley fever in domestic ruminants in the central and northern regions of Burkina Faso. Rev Sci Tech, 2014. 33(3): p. 893-901.
- Boushab, B.M., et al. Severe Human Illness Caused by Rift Valley Fever Virus in Mauritania, 2015. in Open forum infectious diseases. 2016.
- Shoemaker, T.R., et al., First Laboratory-Confirmed Outbreak of Human and Animal Rift Valley Fever Virus in Uganda in 48 Years. Am J Trop Med Hyg. 2019; 100(3):659-671, 2019. 100(3).
- Nyakarahuka, L., et al., Prevalence and risk factors of Rift Valley fever in humans and animals from Kabale district in Southwestern Uganda, 2016. PLoS neglected tropical diseases, 2018. 12(5): p. e0006412-e0006412.
- Ng’ang’a, C.M., S.A. Bukachi, and B.K. Bett, Lay perceptions of risk factors for Rift Valley fever in a pastoral community in northeastern Kenya. BMC Public Health, 2016. 16(1): p. 32.
- Ikegami, T. and S. Makino, The pathogenesis of Rift Valley fever. Viruses, 2011. 3(5): p. 493-519.
- Hassan, A., et al., Epidemiological Investigation of a Rift Valley Fever Outbreak in Humans and Livestock in Kenya, 2018. The American Journal of Tropical Medicine and Hygiene, 2020. 103(4): p. 1649-1655.
- Macdonald, L.E., et al., A systematic review and meta-analysis of the effects of pasteurization on milk vitamins, and evidence for raw milk consumption and other health-related outcomes. J Food Prot, 2011. 74(11): p. 1814-32.
- van den Bergh, C., et al., High seroconversion rate to Rift Valley fever virus in cattle and goats in far northern KwaZulu-Natal, South Africa, in the absence of reported outbreaks. PLOS Neglected Tropical Diseases, 2019. 13(5): p. e0007296.
- Arsevska, E., et al., Identifying Areas Suitable for the Occurrence of Rift Valley Fever in North Africa: Implications for Surveillance. Transbound Emerg Dis, 2016. 63(6): p. 658-674.
[Rift Valley Fever Outbreak, Kiruhura District, Uganda, June 2021 pdf]
Download Article as PDF below;
Reference this page as below
Hildah Tendo Nansikombi1*, Alex Ndyabakira1, Irene Kyamwine1, Benon Kwesiga1, Fred Monje2, Luke Nyakahurura3, Julie Harris4. Rift Valley Fever Outbreak, Kiruhura District, Uganda, June 2021, Kampala, Uganda National Institute of Public Health, 2021 September 30th. Available from:https://uniph.go.ug/rift-valley-fever-outbreak-kiruhura-district-uganda-june-2021.

Comments are closed.