Incidence and Spatial Distribution of Bacterial Meningitis, Uganda, 2014-2018
Authors: Doreen N. Gonahasa1* | Institutional affiliation: 1Uganda Public Health Fellowship Program, Kampala, Uganda | Email: mailto:doryengona@musph.ac.ug: Tel: +256 779398990
Summary
Uganda is one of the countries with highest rates of meningitis and the risk of incidence is attributable to the fact that it lies within the extended meningitis belt of Sub-Saharan Africa. The most susceptible regions include West Nile, Bunyoro, Acholi, Lango, Teso, and Karamoja regions because they lie within the meningitis belt. Although there have been efforts to vaccinate against meningitis sporadic cases still occur. We characterised bacterial meningitis incidence in Uganda to inform programming. We analysed routinely collected meningitis data from the District Health Information System (DHIS2),2014- 2018. We included all bacterial meningitis patients reported in DHIS2. Overall, there was an increase in the incidence of meningitis from 0.005/100,000 in 2014 to 5.31/100,000 population in 2017; and a slight decline in 2018. The incidence of bacterial meningitis was higher among under-five population ranging between 6.5-10.6/ 100,000 compared to those aged five and above (2.5-4.2/100,000). Karamoja region was most affected compared to the other 14 regions in the country. Sporadic cases of meningitis still occur across the country increasing from 2014 to 2017 with a slight decline in 2018. Children under five and Karamoja region were most affected. Regardless of efforts to vaccinate meningitis remains a disease of public health concern. We recommend that MoH introduces the meningitis vaccine in routine immunisation.
Introduction
Meningitis is an illness caused by inflammation of the meninges (1), the membranes that surround the brain and spinal cord and protect the central nervous system (CNS), together with the cerebrospinal fluid. It is a serious condition that can be life threatening (2). It can be caused by a variety of organisms that include bacteria, fungi, or viruses. As such, different forms exist: viral, non-pyogenic, bacterial, meningococcal, hemophilus, pneumococcal and neonatal meningitis. Of these, the bacterial form is the most severe and most common (3,4) Bacterial meningitis is very serious and can be fatal, with death occurring in a few hours. Most people recover from meningitis; However, permanent disabilities (such as brain damage, hearing loss, and learning disabilities) can result from the infection (5). Meningitis cases typically present with stiff neck, high fever, and sensitivity to light, confusion, headaches, and vomiting (4,5). Other symptoms include weakness, irritability and poor feeding. Even when the disease is diagnosed early, and adequate treatment is started, 5 to 10% of patients die, typically within 24 to 48 hours after the onset of symptoms. If left untreated, up to 50% of cases may die. Bacterial meningitis may also result in brain damage, hearing loss or a learning disability in 10 to 20% of survivors(6).
While bacterial meningitis can happen at any age, infants are susceptible (5). The age groups most at risk of infection are; infants 6 to 18 months of age, children under the age of 5 years, adolescents and young adults, elderly people (due to their declining immune function), and people with illnesses which affect the immune system (1,7,8). It occurs sporadically and in small outbreaks worldwide (10), except in the African Meningitis Belt where large outbreaks are common. Uganda is one of the countries with highest rates of the meningitis A disease and also one of the 26 countries that lie within the extended meningitis belt of Sub-Saharan Africa, which stretches from Senegal in the West Africa to Ethiopia in the East Africa. We determined the incidence and described the spatial distribution of bacterial meningitis using surveillance data, Uganda, 2014-2018 to inform targeted interventions.
Methods
Study area
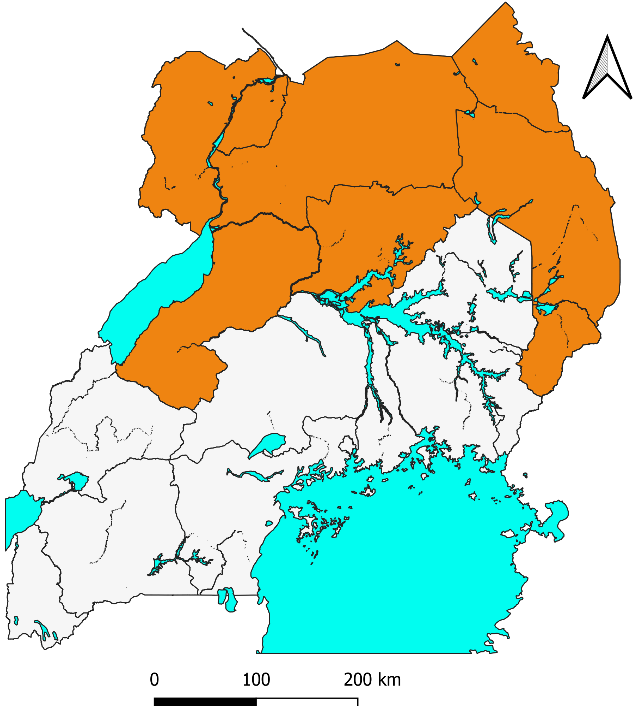
Data utilized in this study was collected nationwide. Uganda has an estimated population of 44m people and is divided into 15 sub regions; Kampala, North Central, South Central, Busoga, Bukedi, Bugisu, Teso, Karamoja, Lango, Acholi, West Nile, Bunyoro, Toro. Some regions of the country lie within the meningitis belt of Sub Saharan Africa, which has experienced frequent outbreaks of meningitis(12). These regions include West Nile, Bunyoro, Acholi, Lango, Teso, and Karamoja regions (shown in orange in Figure 1).
Study design and data source
We abstracted meningitis surveillance data collected by healthcare facilities in all the districts in Uganda from the District Health Information System v2 (DHIS2). The DHIS2 is an open source software used for reporting, analysing, and disseminating health data as part of the Health Management Information System (HMIS).
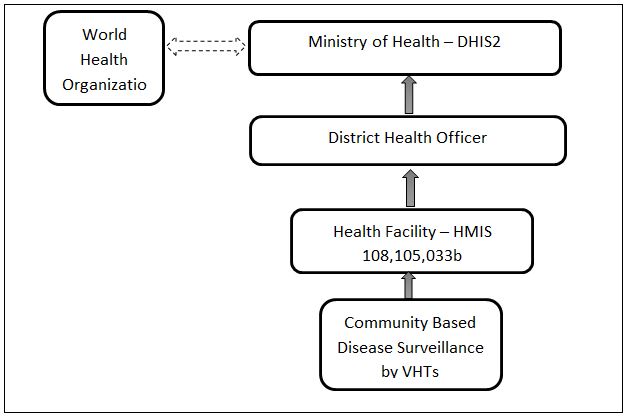
We considered all records of bacterial meningitis patients that reported to the outpatient department (OPD) of health facilities. According to IDSR guidelines, a suspected bacterial meningitis case is any person with sudden onset of fever (> 38.5 °C rectal or 38.0 °C axillary) and one of the following signs: neck stiffness, altered consciousness or other meningeal sign while a confirmed case is a suspected case confirmed by isolation of Neisseria meningitidis from cerebrospinal fluid or blood (11). At the facility, individual patient records are captured using an appropriate medical form and then entered into the OPD register. There are three reporting forms for bacterial meningitis; weekly report (HMIS 033b), monthly summary reports for outpatients (HMIS 105), and inpatients (HMIS 108) (Figure 2). It is from the summaries that data are entered in to the DHIS2. For this analysis we used data submitted through HMIS 105 monthly report.
Data abstraction and analysis
We abstracted data on bacterial meningitis for the period, 2014-2018 from the DHIS2. For each case, we abstracted data on age, sex, and district. We used population data from the Uganda National Census 2014, extrapolating populations for consequent years using an annual population growth estimated of 3% (1).
We used Epi Info 7.2.0 for data analysis. Descriptive data were analyzed using frequencies, means, and dispersion. We calculated disease incidence per 1,000 with the number of bacterial meningitis cases as numerator and the population per affected area as the denominator. We calculated the incidence of bacterial meningitis during the study period and disaggregated it by, age-group, sex, and district. We used quantum geographic information system (QGIS) version 3.2.2 to generate choropleth maps of incidence per year.
Ethical considerations
This analysis used routine surveillance data reported by health facilities for the Uganda Ministry of Health. This data is also aggregated with no individual patient identifiers. However, we sought and obtained permission from MoH to use the data. The US Centers for Disease Control and Prevention (CDC) also provided the non-research determination for non-human subjects. Data were only accessed by the study team.
Results
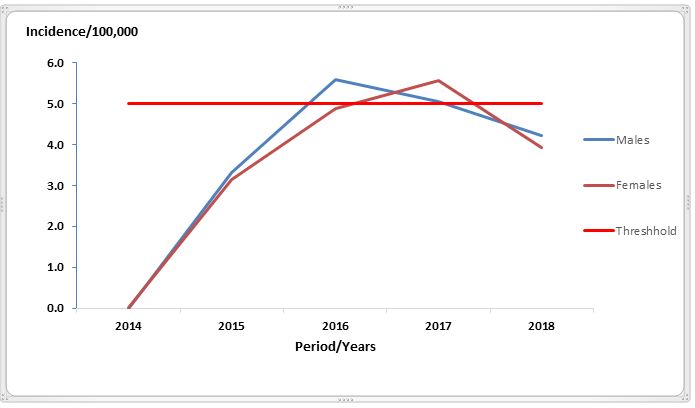
There was an increase in the incidence of meningitis from 0.005/100,000 in 2014 to 5.31/100,000 population in 2017; and a slight decline in 2018. On average, males (3.6/100,000) and females (3.5/100,000) were similarly affected across the period of consideration (Figure 3). The incidence in 2016 and 2017 was slightly higher than the threshold of 5/100,000
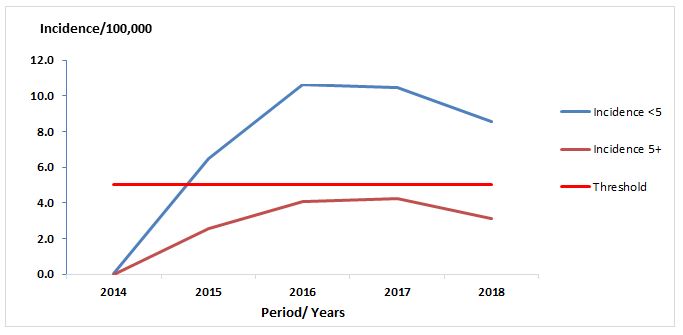
Across the period of review, a general increase in the incidence of meningitis from 2014 to 2016 in both age groups (under 5 and 5+) (Figure 4) was observed. There was a slight decline between 2016 and 2017 and a more remarkable decline between 2017 and 2018. Generally, the incidence was higher in the population under five years of age (6.5-10.6/ 100,00) compared to that aged five and above (2.5-4.2/ 100,000).
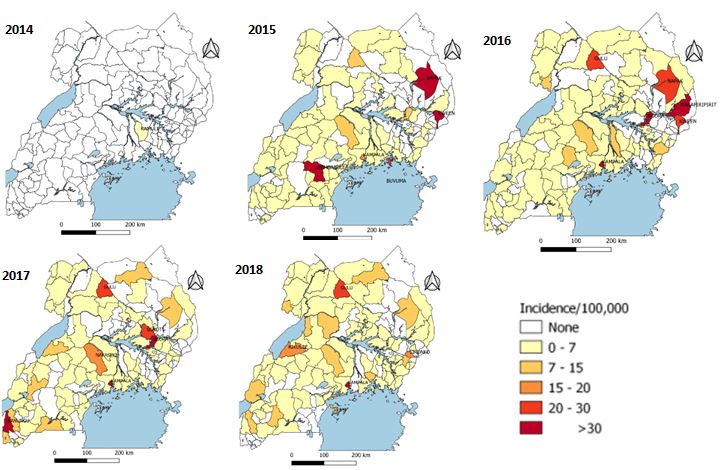
The highest incidence of meningitis cases (shown in deep red) was reported in Kampala over the five-year period, Napak and Nakapiripirit, districts in Karamoja region, and Gulu in the Northern region while central and western regions reported the lowest incidences (Figure 5).
Discussion
For the period between 2014 and 2017, incidence of bacterial meningitis increased. Kampala, Karamoja, and northern regions were the most affected. The illnesses affected mainly children under five years of age.
The incidence of meningitis increased from 2014 to 2017 and there was a slight decline in 2018 following a mass meningitis immunization campaign in 39 high-risk districts across the country in January 2017 (13). This drive was conducted by the Ministry of Health in collaboration with WHO and the United Nations International Children’s Fund (UNICEF). The campaign was targeted to immunize the population in the age group 1 -29 years, strengthen surveillance, and routine immunization service delivery in the districts, and achieve at least 80% coverage for vaccination in the 39 high risk districts. The area targeted, as reflected in the results of this analysis has been prone to meningitis. The preventive immunization campaign focused on the greater Northern Uganda and parts of Western Uganda, because they lie in the meningitis belt of Sub Saharan Africa, which has experienced frequent outbreaks of meningococcal meningitis This is because the dusty winds and cold nights which characterize the period between December and June in the meningitis belt increase the risk of meningitis (14). Transmission of meningitis is further facilitated by overcrowded housing(15) and large population displacements (16).
This analysis showed that children under five were most affected. It is reported that bacterial meningitis is life-threatening and mostly affects children and adolescents, and may be the cause of severe neurological sequelae (1). Documentation has highlighted similar findings (18). These findings could be attributed to poor prognosis(17) and the fact that children have an under developed immune system especially in the central nervous system (CNS) to prevent infection from crossing to the brain. Also, children are prone to numerous bacterial infections resulting into septicaemias that later affect the CNS(19). Therefore, there is need to vaccinate children which is an effort that has proven to work in reducing the incidence of meningitis (20,21)
Study limitations
Data analysed for this study was collected from a passive surveillance system hence the results are subject to reporting biases like under reporting caused by delays and failure to submit monthly reports by the health facilities. Some patients do not seek care at the health facilities leading to lower reported numbers and eventual underestimation in the burden of disease.
Conclusions
Between 2014 and 2018, data abstracted from the DHIS2 showed that incidence of bacterial meningitis was higher among the under-five population compared to that aged five and above. Males were slightly more affected and spatial incidence was higher in the north eastern region of the country. While there have been efforts by the government to carry out vaccination against meningitis there are still sporadic cases that may need to be intentionally targeted particularly in the northern region where although a mass vaccination was carried out in 2017 and a decline noted, cases continue to occur. The country remains at risk owing to proximity to the DRC where there has been a recent outbreak. We recommend that the MoH includes meningitis in the routine immunization schedule.
Acknowledgement
We would like to acknowledge the responsible departments: Integrated Epidemiology, Surveillance and Public Health (IES&PH) and Division of Health Information (DHI) of the MoH for allowing us to use the routinely generated surveillance data.
References
- Meningitis | Home | CDC [Internet]. 2020 [cited 2020 Jul 15]. Available from: https://www.cdc.gov/meningitis/index.html
- Dickinson FO, Pérez AE. Bacterial Meningitis in children and adolescents: an observational study based on the national surveillance system. BMC Infect Dis. 2005 Nov 15; 5:103.
- Kisakye A, Makumbi I, Nansera D, Lewis R, Braka F, Wobudeya E, et al. Surveillance for Streptococcus pneumoniae Meningitis in Children Aged <5 Years: Implications for Immunization in Uganda. Clin Infect Dis. 2009 Mar;48(s2):S153–61.
- David H. Control of communicable diseases manual. American public health association; 2015.
- Meningitis | About Bacterial Meningitis Infection | CDC [Internet]. 2019 [cited 2020 Jan 9]. Available from: https://www.cdc.gov/meningitis/bacterial.html
- WHO | Number of suspected meningitis cases and deaths reported [Internet]. WHO. [cited 2020 Jan 9]. Available from: https://www.who.int/gho/epidemic_diseases/meningitis/suspected_cases_deaths_text/en/
- Meningitis | About Bacterial Meningitis Infection | CDC [Internet]. 2019 [cited 2020 Jul 15]. Available from: https://www.cdc.gov/meningitis/bacterial.html
- Meningitis: Symptoms, Causes, Types, Treatment, Risks, & More [Internet]. [cited 2020 Jul 15]. Available from: https://www.healthline.com/health/meningitis#vaccine
- Meningococcal meningitis [Internet]. [cited 2020 Jul 15]. Available from: https://www.who.int/news-room/fact-sheets/detail/meningococcal-meningitis
- Meningitis [Internet]. [cited 2020 Jul 15]. Available from: https://www.who.int/westernpacific/health-topics/meningitis
- IDSR NTG for Integrated Disease Suveillance (2).pdf.
- Molesworth AM, Cuevas LE, Connor SJ, Morse AP, Thomson MC. Environmental Risk and Meningitis Epidemics in Africa – Volume 9, Number 10—October 2003 – Emerging Infectious Diseases journal – CDC. [cited 2021 Sep 20]; Available from: https://wwwnc.cdc.gov/eid/article/9/10/03-0182_article]
- Uganda vaccinates against Meningitis type A in the 39 high-risk districts [Internet]. WHO | Regional Office for Africa. [cited 2021 Jun 14]. Available from: https://www.afro.who.int/news/uganda-vaccinates-against-meningitis-type-39-high-risk-districts
- Garc ía-PCP, Stanton MC, Diggle PJ, Trzaska S, Miller RL, Perlwitz JP, et al. Soil Dust Aerosols and Wind as Predictors of Seasonal Meningitis Incidence in Niger. Environ Health Perspect. 2014 Jul 1;122(7):679–86.
- Sultan B, Labadi K, Guégan J-F, Janicot S. Climate Drives the Meningitis Epidemics Onset in West Africa. PLOS Med. 2005 Jan 25;2(1): e6.
- Sabatini C, Bosis S, Semino M, Senatore L, Principi N, Esposito S. Clinical presentation of meningococcal disease in childhood. Meningococcal Dis. :4.
- Dickinson FO, Pérez AE. Bacterial Meningitis in children and adolescents: an observational study based on the national surveillance system. BMC Infect Dis. 2005 Nov 15; 5:103.
- Defeating meningitis by 2030: a global road map. 2020;37.
- JAROUSHA AMA, AFIFI AhmedA. Epidemiology and Risk Factors Associated with Developing Bacterial Meningitis among Children in Gaza Strip. Iran J Public Health. 2014 Sep;43(9):1176–83.
- Makwana N, Riordan FAI. Bacterial meningitis: the impact of vaccination. CNS Drugs. 2007;21(5):355–66.
- Stefanelli P, Rezza G. Impact of vaccination on meningococcal epidemiology. Hum Vaccines Immunother. 2015 Oct 29;12(4):1051–5.
Reference this page as below
Doreen N. Gonahasa1* . Incidence and Spatial Distribution of Bacterial Meningitis, Uganda, 2014-2018, Kampala, Uganda National Institute of Public Health. 2021 September 30th. Available from:https://uniph.go.ug/incidence-and-spatial-distribution-of-bacterial-meningitis-uganda-2014-2018.

