Rift Valley Fever Outbreak Caused by Handling a Dead Calf: Kiruhura District, 2017-2018
Authors: Doreen Birungi1, Freda Loy Aceng1, Fred Monje1,3, Deo Ndumu3, Robert Aruho4, Paul Lumu3, Luke Nyakara-huka2, Benon Kwesiga1, Julius Lutwama2, Alex Riolexus Ario1; Affiliations:1 Uganda Public Health Fellowship Program, 2.Uganda Virus Research Institute 3 Ministry of Agriculture, Animal Industry and Fisheries 4 Uganda Wildlife Authority
Executive summary
Rift Valley fever (RVF) is a viral zoonosis that causes severe disease in animals and humans. The disease results in significant economic losses due to death and abortions among RVF-infected livestock. On 7th December 2017, the Uganda Ministry of Health received an alert of one suspected Viral Hemorrhagic Fever case-patient from Kiruhura District. Laboratory results from UVRI indicated that the case-patient was PCR- positive for Rift Valley Fever. We investigated to determine the extent, identify risk factors, and recommend control and prevention measures. All case-persons had a previous exposure to sick animals either from direct or indirect contact with the blood or organs of infected animals.
Background
Rift Valley Fever (RVF) is a zoonosis that affects animals and humans. Most of human infections result from direct or indirect contact with the blood or organs of infected animals. The virus may be transmitted to humans through handling of animal tissue during slaughtering or butchering, assisting with animal births, conducting veterinary procedures, or from the disposal of carcasses or fetuses.
Occupational groups such as herders, farmers, slaughterhouse workers, and veterinarians are therefore at higher risk of infection. RVF virus has an incubation period of 2-6 days following infection[1]. RVF symptoms and signs in persons are typically fever, myalgia, and malaise; in a minority of cases retinitis, encephalitis, hemorrhagic fever. Death may occur as a result of RVF infection with an overall mortality rate of ≈1%[2].
Lab-confirmation of RVF is by either detection of RVF nucleic acid by reverse-transcriptase polymerase reaction (RT-PCR) or demonstration of serum IgM/IgG antibodies by ELISA On 7 December, 2017, the Uganda Ministry of Health (MoH) through Public Health Emergency Operational Centre (PHEOC) received an alert of a suspected VHF from Kiruhura District. This was a 24-year-old male that presented with VHF symptoms of high grade fever, headache, blood in vomitus and bleeding from the nose. He hailed from Rushororo village, Kanyaryeru sub-county Kiruhura District. He had been admitted at Mbarara Regional Referral Hospital where a blood sample was drawn and shipped to UVRI for testing.
Laboratory results from UVRI indicated that the case patient was PCR- positive for Rift Valley Fever (RVF). Ministry of Health sent a team consisting of epidemiologists, entomologists, laboratory technicians and veterinarians to investigate the outbreak. The set out to establish the scope and identify risk factors for the outbreak and recommend evidence-based interventions.
Methods
We defined a suspected case as acute onset of fever (>37.5oC), negative malaria test result, and at least two of the following symptoms; headache, muscle or joint pain, bleeding and any gastroenteritis symptom (nausea, vomiting, abdominal pain, diarrhea) in a resident of Kanyaryeru subcounty from 1st October, 2017 to 30 January, 2018.
A confirmed case was a suspected case with a laboratory confirmation by either detection of RVF nucleic acid by reverse transcriptase polymerase reaction (RT-PCR) or demonstration of serum IgM or IgG antibodies by ELISA. We used a standard case investigation form for VHFs to collect information from the case-persons.
We conducted indepth interviews with case-persons that were infected with RVF. We conducted active community case finding and contact tracing in Kanyaryeru sub-county and developed a linelist. Blood samples from 9 suspected case-persons were collected and shipped to UVRI for testing. Blood samples from 146 cattle, 76 goats, 20 sheep from four selected farms in Kanyaryeru sub-county were transported to National Animal Disease Diagnostic and Epidemiology Centre (NADDEC) for testing
The veterinary team investigated the evidence of RVF in animals in the affected area and collected blood samples from wild animals. An environment assessment was conducted to identify possible risk factors that could be facilitating transmission of RVF. We observed physical features on affected farms in the affected sub-county.
Findings
We identified four confirmed case-persons. All affected case persons were males with a median age of 24 years (IQR: 17 31.5). There was no death reported (CFR=0%). All case persons originated from Rushororo village, Kanyaryeru sub-county Kiruhura District.
Epidemiological linkage
Case-person 1: On 25 November, 2017, a two-week-old calf on Farm X died of unknown cause. It was butchered by three farm workers and the meat consumed. After 2 days, a 24-year -old male (case-person 1) involved in butchering the dead calf presented with high grade fever and severe headache. He was admitted for one night at clinic X in Sanga town where he was treated for malaria. On 4th December, he developed nasal bleeding and was re-admitted at the same clinic. He was treated with IV Quinine, IV fluids for two days thereafter referred to Mbarara Regional Referral Hospital (MRRH).
At MRRH, the patient’s condition worsened with symptoms such as hematemesis (blood or coffee grounds in vomit and black stools (melena), extreme weakness, sore throat, hiccups, joint pains and muscle pains for 3 days. A blood sample was drawn and shipped to UVRI for testing. Laboratory results from UVRI indicated that the case-patient was PCR positive for RVF.
During contact tracing, farm workers that participated in the slaughter of the calf and had history of sickness in that period, had their blood samples drawn for testing. The following case-persons were identified after blood testing.
Case-Person 2: On 28 November, 2018, a day after butchering the dead calf, a 24 years-old male who was involved in the butchering process presented with fever and headache, however he didn’t seek medical care. The investigation team collected his blood sample and the test result indicated both antiRVF specific IgM and IgG.
Case-person 3: On 29 November, 2017, two days after butchering the calf, an 11 years-old male who assisted in carrying offals from the dead calf developed symptoms of high grade fever and headache. His blood test result indicated anti-RVF specific IgM antibodies.
Case-person 4: On 18 November, 2017, eight -days before the death of the calf, a 39 years-old male developed symptoms. This indicated that most probably he had a different exposure or source of infection. Upon testing, anti-RVF specific IgG antibodies were detected which indicated a previous exposure to RVF virus.
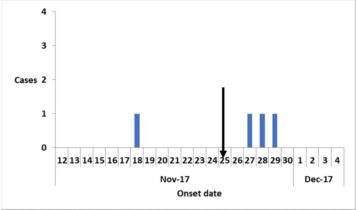
This was a point source outbreak with exposure on 25 November, 2017. The index case-patient developed symptoms on 27, the second case-patient and third case-patient developed symptoms on 28 and 29 respectively. However, the case-person that developed symptoms on 18 November, 2017 had unknown exposure.
Laboratory Investigations
We tested 9 suspected case-persons and four turned positive for RVF. To monitor viremia, subsequent blood testing from case-persons was conducted and two of the confirmed cases recovered while the other two were still positive for RVF at the time of investigation. Of the four farms
sampled, 44% (64/146) of cattle, 46% (35/76) of goats and 45% (9/20) of the sheep tested positive for RVF. Among wild life, 10% (1/10) of Zebras, 100% (1/1) of Etopi and 100% (1/1) of Impala tested positive for RVF.
Environmental/Veterinary investigations
We purposively selected one farm where the confirmed case-persons were working and the other three farms in close proximity with this farm denoted as X. Between November, 2017 and January, 2018, a total of 4 sudden deaths and 4 still births had been reported among goats while
among cattle, reports of still births and one sudden death had occurred on Farm X. Farm X shares a border with Lake Mburo National Park and it was observed that wild animals freely interacted with the domestic animals during grazing.
Discussion
In this outbreak, human infections were associated with handling dead meat or organs from infected animals. All the infected herdsmen were involved in slaughtering of the calf that had died of unknown cause and most probably had been infected with RVF virus. This is similar to other
outbreaks that have occurred in other parts of the country, where the infected persons have had a history of either handling animals that have died of unknown cause or consuming raw animal products.
It is noteworthy that RVF outbreaks are strongly linked to excessive/ heavy rainfalls and prolonged flooding, which increases habitat suitability for vector population thus influencing the risk of disease emergence, transmission and spread. The onset of RVF outbreaks appears to be also associated with dry spell events as seen in this outbreak [3].This outbreak occurred after a long dry spell and most probably domestic animals could have been exposed to Rift valley virus as they grazed in the nearby forested area around the affected farms. This is supported by studies conducted in Kenya which indicated that the highest RVFV circulation was detected after herds passed through bony forested areas[4]
Conclusion
This was an RVF outbreak in humans and animals affecting Kanyaryeru sub-county in Kiruhura District caused by interaction of domestic and wild animals from lake Mburo national game park. The index case-person was probably infected through contact with infected dead calf that was butchered on 25 November, 2017.
Recommendations
- The Ministry of Agriculture, Animal Industries and Fisheries (MAAIF) should ensure enforcement of laws prohibiting the sale and consumption of either sick or dead animals that have died of un known cause.
- Control of movement of animals from the affected areas should be considered and moreso, interaction between domestic and wild animals should be minimized through law enhancement by wild life authorities.
- Enhanced surveillance of RVF in animals and humans in Kiruhura District should continue to identify any other affected farms and persons.
- Mass education of the communities about RVF. The communities should report any usual events such as sudden deaths, abortions, still births observed on farms.
References
- Gerdes, G., Rift valley fever. Revue scientifique et technique Office International des Epizooties, 2004. 23(2): p. 613-624.
- LaBeaud, A.D., et al., Interepidemic Rift Valley fever virus seropositivity, northeastern Kenya. Emerging infectious diseases, 2008. 14(8): p. 1240.
- FAO, Rift Valley Fever (RVF): Emergency Prevention System (EMPRES) for Transboundary Animal and Plant Pests and Diseases. 2016.
- Owange, N.O., et al., Occurrence of rift valley fever in cattle in Ijara district, Kenya. Preventive veterinary medicine, 2014. 117(1): p. 121-128.

