Organoph osphate poisoning distribution, temporal and spatial trends, Uganda, 2017─2022
Authors: Robert Zavuga*1, Mercy Wendy Wanyana1, Gorrete Zalwango1, Patrick King1, Richard Migisha1, Daniel Kadobera1, Benon Kwesiga1, Peter Edward Okello1, Lilian Bulage1, Freda Loy Aceng2, Joshua Kayiwa3, Issa Makumbi3, Alex Riolexus Ario1 Institutional affiliations: 1Uganda Public Health Fellowship Program-Uganda National Institute of Public Health, Kampala, Uganda 2Department of Integrated Epidemiology, Surveillance and Public Health Emergencies, Ministry of Health, Kampala, Uganda 3Public Health Emergency Operations Centre, Ministry of Health, Kampala, Uganda *Correspondence: Email: rzavuga@musph.ac.ug, Tel: +256772655723
Summary
Introduction: Organophosphates (OP) are toxic chemical agents used as agricultural pesticides and insecticides and are one of the commonest agents of poisoning worldwide, responsible for >3,000,000 poisonings and 300,000 deaths globally per year. As a country with an agriculture-based economy, Uganda has widespread use of pesticides, creating an elevated risk for OP poisoning. We assessed the distribution and temporal and spatial trends of OP poisoning admissions in Uganda during 2017─2022 to guide control and prevention interventions.
Methods: We analysed OP poisoning surveillance data from the District Health Information System version 2 (DHIS2). As per DHIS2, OP poisoning admissions were defined as a hospital stay due to suspected OP poisoning while deaths were defined as inpatient deaths with OP poisoning listed as the cause of death. We calculated annual incidence of OP poisoning admissions per 100,000 population and case-fatality rates per patient admitted with OP at national, regional, and facility levels. We used the Mann-Kendall (MK) test to determine the strength and direction of the trend.
Results: Overall, a total of 37,883 (average: 6,314 per year) OP admissions and 1,599 (average: 267 per year) deaths were reported (case-fatality rate [CFR]=4.2%) during 2017-2020. Males (incidence=18/100,000), children <5 years (incidence=20/100,000), and residents of Ankole Region (incidence=26/100,000) were the most affected. CFRs increased with increasing healthcare level of the admitting health facility. The incidence of OP declined by over 3-fold over the study period (MK=-13, p=0.02). Kiruhura and Bukwo districts had consistent high incidences (>50/100,000) throughout the study period.
Conclusion: There was a significant reduction in incidence of OP poisonings in Uganda during 2017-2020. Males, children <5 years, and residents in Ankole Region were the most affected. Strengthening sensitization among agricultural and livestock farming communities about the risks of pesticide poisoning and building capacity of health workers and equipping lower-level health facilities to effectively manage medical emergencies including OP poisoning could reduce the OP burden and mortality in Uganda.
Introduction
Organophosphates are a group of highly toxic chemical compounds that are commonly used as agricultural pesticides and insecticides[1]. They are one of the main agents of poisoning, responsible for over 3,000,000 poisonings and an estimated 300,000 deaths per year worldwide [2]. These poisonings, which lead to substantial morbidity and mortality among the exposed, may occur due to occupational or accidental exposure, deliberate ingestion in cases of suicide, or during chemical warfare [3, 4].
Most organophosphate poisonings have involved exposures to agricultural pesticides [5]. The major routes of exposure for organophosphates are the respiratory tract, gastrointestinal tract, skin, and eyes [6].The clinical features of organophosphate poisoning are based in the central nervous system and include salivation, lacrimation, urination, defecation, abdominal pain, general body weakness, vomiting, loss of consciousness, anxiety, tremors, and convulsions [7]. Once exposed, symptoms occur within minutes to hours depending on the type of organophosphate poison, route of exposure, and dose [8].
In low and middle-income countries (LMIC), the significant reliance on pesticides for agricultural production results in an elevated risk of exposure to organophosphates [4]. The widespread availability and indiscriminate use of pesticides in such settings, coupled with poor storage and handling practices and lack of awareness about the consequences of poisoning make LMIC particularly vulnerable [9].
Uganda has a largely agricultural economy [10] and a development strategy hinged on rapid industrialization in agriculture [11], which results in the widespread use of pesticides among agricultural farmers [12]. In Uganda, pesticides, including organophosphates, are widely available in animal drug shops and shops that sell general merchandise, and can be found on farms and in homes [13]. There have been previous reports of organophosphate poisoning in Uganda linked to both intentional and unintentional pesticide exposures. [12-14].
Prevention efforts for pesticide poisoning in Uganda have included health education and sensitization on proper use of pesticides among farming communities [15]. There are other measures which the limit the availability and toxicity of pesticides, such as regulation to limit sales to trained and licensed vendors [16]. Additionally, the replacement of highly toxic pesticides with less toxic and equally potent ones has also been implemented [17].
Despite the risk potential, little is known about the burden of organophosphate poisoning in Uganda. We assessed the distribution, temporal, and spatial trends of organophosphate poisoning in Uganda 2017─2022, to guide targeted control and prevention interventions.
Methods
Study design and data Source
We analysed organophosphate poisoning surveillance data captured in the District Health Information System version 2 (DHIS2). The DHSI2 is an open-source web based platform that is used to collect, report, and analyse aggregate data that is routinely generated across health facilities in Uganda[18]. Uganda has 146 districts which are distributed across the 15 regions as designated by the Ministry of Health.
The healthcare system comprises government and privately owned health facilities which are organized in a hierarchical order [19] from Health Centre (HC) II (found at parish level), HCIII (found at sub-county level), HCIV (found at county/health sub-district level), district hospital (found at district level), regional referral hospital found at regional level), and the national referral hospital (found at national level).
The DHIS2 collects data on priority diseases, conditions, and events of public health importance including organophosphate poisoning from the Health Management Information system (HMIS). All cases suspected of organophosphate poisoning are recorded in HMIS as admissions/in-patient occurrences. The HMIS is a paper-based system in which health facilities record patient data on conditions of interest. These data are later entered into the electronic DHIS2 and aggregated from all health centres in the country.
Study variables, data abstraction, management, and analysis
We abstracted aggregate data on organophosphate poisoning admissions and
deaths from the inpatient monthly reports in the Health Management Information System (HMIS) from 2017 to 2022. As per HMIS, organophosphate poisoning admissions were defined as a hospital stay due to suspected organophosphate poisoning as a primary diagnosis. Organophosphate poisoning deaths were defined as inpatient deaths with organophosphate poisoning listed as the cause of death in DHIS2.
Data were imported into STATA version 16 software for analysis. We calculated the annual incidence of OP poisoning as annual admissions due to OP poisoning per 100,000 population. Population data was obtained from the Uganda Bureau of Statistics population estimates[20]. Additionally, we calculated the case fatality rate (CFR) of OP poisoning as a percentage of number of deaths due to OP poisoning divided by the number of OP admissions.
We calculated annual incidence of organophosphate poisoning and the overall case fatality rates at national, regional, and health facility level. We used line graphs to describe national trends of OP admissions and CFR. The Mann-Kendall test was used to determine the significancy of the trends. Choropleth maps were drawn using QGIS software to show the spatial distribution of organophosphate incidence in the country.
To further contextualize the findings, we also abstracted data on reporting rates, calculated as the percentage of complete submitted monthly reports over the study period divided by the number of expected reports.
Ethical considerations
The DHIS2 data are aggregated without individual identifiers. We sought permission to use the data from the Uganda Ministry of Health. The US Centres for Disease Control and Prevention (CDC) determined that the work did not fit the definition of public health research and was aimed at improving public health programming. Data were only accessed by the study team.
Results
Incidence and case fatality rate of organophosphate poisoning, Uganda, 2017-2022
Overall, a total of 37,883 (average: 6,314 per year) organophosphate poisoning cases.
The overall average incidence was 15 organophosphate admissions per 100,000 persons. Residents of Ankole Region were more affected while those in Lango Region were least affected. (Incidence: 26/100,000 vs 7/100,000 persons). (Table 1). Males had a higher incidence of organophosphate poisoning than females (18 vs 13/100,000, p=0.03). Children <5 years had a higher incidence than persons ≥5 years (20 vs 14/100,000, p=0.01). Overall, 1,599 (average: 267 per year) deaths were reported (CFR)= 4.2% during 2017-2022. Residents in Kampala Region had the highest overall CFR while those in Teso Region had the lowest (CFR: 8.5% vs 2.2%) (Table 1).
Table 1: Incidence and case fatality rate of organophosphate poisoning, Uganda, 2017─2022
| Cases | Average population | Incidence /100,000 | Deaths | Case fatality
rate (%) |
|
| Sex | |||||
| Female | 2,772 | 20,951,652 | 13 | 75 | 2.7 |
| Male | 3,542 | 20,100,565 | 18 | 192 | 5.4 |
| Age group | |||||
| <5 yrs | 1,570 | 7,715,064 | 20 | 48 | 3.1 |
| ≥5 yrs | 4,744 | 33,337,153 | 14 | 219 | 4.6 |
| *Health facility level | |||||
| HC III | 1,253 | – | – | 29 | 2.3 |
| HC IV | 1,374 | – | – | 37 | 2.7 |
| District Hospital | 2,911 | – | – | 141 | 4.8 |
| Regional Referral | 684 | – | – | 52 | 7.6 |
| National Referral | 92 | – | – | 9 | 9.7 |
| *Ownership | |||||
| Govt | 3,769 | – | – | 163 | 4.3 |
| Private | 2,545 | – | – | 104 | 4.0 |
| Region | |||||
| Ankole | 871 | 3,308,524 | 26 | 38 | 4.4 |
| Bukedi | 511 | 2,269,307 | 23 | 12 | 2.3 |
| Tooro | 677 | 3,030,632 | 22 | 33 | 4.8 |
| Teso | 613 | 2,877,800 | 21 | 14 | 2.2 |
| Bugisu | 431 | 2,124,113 | 20 | 15 | 3.4 |
| Acholi | 332 | 1,890,706 | 18 | 22 | 6.6 |
| Kigezi | 290 | 1,637,823 | 18 | 17 | 5.8 |
| North Central | 624 | 4,869,437 | 13 | 32 | 5.1 |
| Bunyoro | 327 | 2,638,612 | 12 | 15 | 4.6 |
| Kampala | 222 | 1,848,566 | 12 | 19 | 8.5 |
| Karamoja | 118 | 1,168,481 | 10 | 4 | 3.3 |
| South Central | 536 | 5,782,964 | 9 | 20 | 3.7 |
| West Nile | 278 | 3,202,789 | 9 | 10 | 3.8 |
| Busoga | 323 | 4,227,008 | 8 | 12 | 3.7 |
| Lango | 162 | 2,444,762 | 7 | 7 | 4.3 |
| Total | 6,314 | 41,052,217 | 15 | 267 | 4.2 |
*Population data for health facility level and ownership was not available to calculate incidence
There was no difference between in CFR by age or sex. CFRs increased with increasing admitting health care level of the health facility. Lower-level health facilities like HCIII had low CFR and compared to high level health facilities-the National Referral Hospitals (CFR: 2.3% Vs 9.7%) (Table 1).
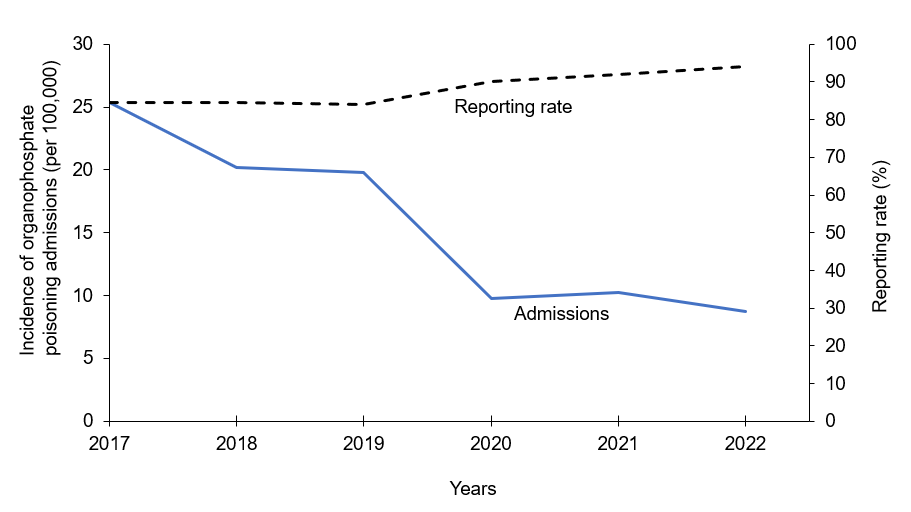
Overall trend of incidence of organophosphate poisoning admissions, Uganda 2017─2022
There was a 350% (more than 3-fold) decline (MK=-13, p=0.02) in incidence of OP poisoning admissions per 100,000 population from 2017─2022. The greatest decline was between 2019 and 2020 (Figure 1). Reporting rates were high and stable over the study period (Range: 86%–94%).
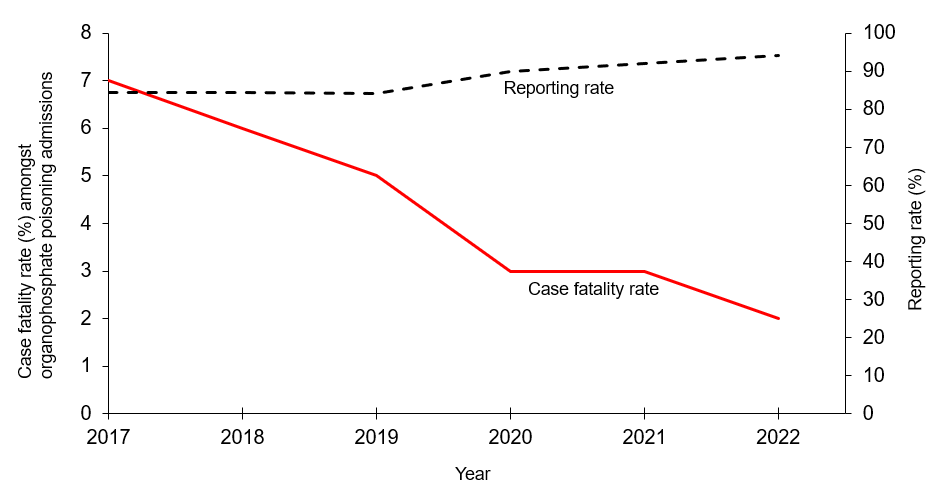
Trend of case fatality rate of organophosphate poisoning, Uganda 2017─2022.
There was no significant change (MK=-9, p=0.13) in the case fatality rate of organophosphate poisoning, 2017─2022 (Figure 2). The greatest decline was between 2018 and 2019 (Figure 2). Reporting rates were high and stable over the study period (Range: 86%–94%).
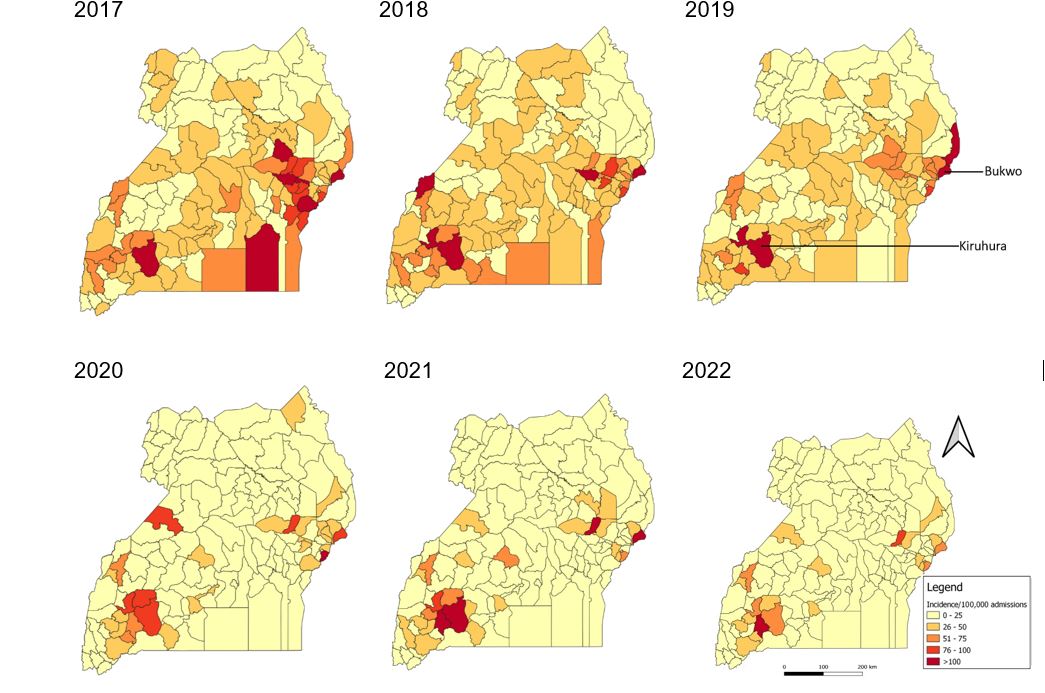
Spatial distribution of organophosphate poisoning admission incidence, district level, Uganda, 2017─2022
Overall, the incidence of organophosphate poisoning admissions declined across all districts. The number of districts reporting >100 cases per 100,000 admissions reduced from seven districts in 2017 to one district in 2022. Spatial clustering of high-incidence districts was observed in the east and south-western parts of the country. The incidences in Kiruhura and Bukwo districts remained high every year over the study period (Figure 3).
Discussion
We assessed the trends and spatial distribution of organophosphate poisoning admissions incidence and deaths in Uganda, 2017─2022. The incidence of organophosphate poisoning admissions declined over the study period with an overall CFR of4.2%. Males, children <5 years, and residents of Ankole Region were the most affected. Two districts (Kiruhura and Bukwo) had the highest incidences throughout the study period.
The incidence of organophosphate poisoning admissions declined throughout the study period. Since 2014, Uganda has implemented periodic public awareness campaigns about safe use of pesticides for small-holder farmers and pesticide dealers [21]. These campaigns have included sensitization about responsible handling to reduce risk of poisoning and environmental pollution. Additional campaigns targeting government pesticide regulators, non-governmental organisations, and media have also been implemented to address the dangers of organophosphate poisoning [22].
These have included information about safe handling and use of pesticides and sensitization about banned and counterfeit pesticides. Similar health education and hazard assessment programs have been shown to have contributed to a reduction in organophosphate incidences amongst livestock farmers in Zambia [23]. Additionally, in 2008, Uganda ratified the Rotterdam Convention, which banned the importation and use of highly toxic pesticides [24]; Uganda has also implemented the Agricultural Chemical Control Act to use less toxic pesticides [25]. Together, these may be contributing to the reduction in the incidence of organophosphate poisonings. To continue this decline, it is important to monitor and strengthen these interventions.
The overall CFR was 4.2%. This is lower than the CFR in two other Uganda studies on organophosphate poisonings done in hospital emergency centres in Uganda in 2022 (18%; 11/61) and 2018 (7.3%; 7/96) [26, 27]. Mortality in organophosphate poisoning depends on the route of administration, the exposure dose, obtaining early diagnosis, and availability of appropriate medical care [28, 29]. It is possible that since patients included in this study were inpatients, they may have had access to appropriate treatment, including activated charcoal and atropine, which are known to decrease mortality after organophosphate ingestion [3, 30].
High CFRs were reported in a retrospective study; CFR=7.8% (51/656) and a prospective study CFR=5.6% (13/230) conducted in Tanzania[31]. This was attributed to challenges in clinical management of patients due to lack of specific details on the OP chemicals responsible for poisoning during hospital care. Ensuring that hospitals are stocked with equipment and antidotes for organophosphate could help further reduce the mortality associated with this exposure.
Males in our study were more affected than females. In Uganda, men are more involved than women in agricultural activities which involve spraying of pesticides and these put them at high risk of occupational exposure [32-34]. Occupational exposures can occur through unintentional ingestion, inhalation, and skin and eye contact [35]. Studies in India have similarly identified higher incidence of organophosphate poisoning among men than women [36, 37]. There is need to sensitize the public, especially men involved in agricultural work, about the importance of wearing personal protective gear like gloves, boots, and gloves during pesticide application.
Children below 5 years were more affected by organophosphate poisoning than persons who were above 5 years. Studies in Uganda and China in 2017 also found that children were more affected than adults [38-40]. Globally, most organophosphate poisoning cases in children are accidental and occur after they ingest pesticide that was poorly stored in households [41, 42]. In Uganda, there is often poor storage practices of pesticides in the households [38], leading to easy access by children.
The exploratory and inquisitive behaviour together with frequent hand-mouth movements puts children at a risk of pesticide poisoning through the oral route [43]. Interventions that facilitate further reduction in the incidence of organophosphate poisoning amongst children are advisable. For instance, care takers to safely keep pesticides away from reach of children and packaging pesticides in containers that cannot easily be breached by children.
Residents in Ankole Region were the most affected by organophosphate poisonings. Additionally, the incidences of Kiruhura and Bukwo districts remained high every year during the study period. Ankole Region (which includes Kiruhura District) is one of several regions engaged in both agriculture and livestock farming [44]. This region implements the intensive mixed farming model of growing of crops (banana-coffee) and rearing of cattle unlike other regions which exclusively apply either the crops (banana, coffee, millet, tea, cotton, millet, maize and cassava) or rearing animals (cattle-goats) only models[45].
This may lead to increased circulation of organophosphate agro-chemicals in Ankole Region as opposed to other regions. Additionally, poor handling likely plays a role. A study in Ankole Region about the usage of pesticides amongst dairy livestock farmers revealed that most farmers handled highly toxic agrochemicals without following proper instructions or having personal protective equipment [46].
However, similar data are not available for other regions. Like Kiruhura District, Bukwo District is also heavily involved in agriculture and livestock farming [47, 48]. Further investigation is needed to understand the reason for persistently elevated levels of organophosphate poisoning in these districts, compared to other districts with similarly agricultural and livestock-based economies.
Higher-level admitting health facilities recorded a higher CFR compared to lower-level health facilities. Lower-level health facilities (which act as the first point of care) may not have the staff, stock, or equipment to handle emergency poisoning cases [49, 50] and often refer cases to higher-level facilities, which can incur treatment delays.
In addition, more severe cases may be more likely to attend the higher-level facilities as their first point of care. Together, these may contribute to the higher CFRs in higher-level facilities. These findings are consistent with those in the Tanzanian study which showed that higher level health level facilities had a higher CFR than lower level primary health facilities [31].
This was attributed to lack of clinical capacity amongst healthcare workers to diagnose and treat such cases at primary healthcare level. It is important that rapid referrals are done from lower-level health facilities to higher level health facilities. In areas in which organophosphate poisonings comprise a high proportion of patient visits, it may be worthwhile to stock antidotes and train staff to manage such cases until they can reach higher-level facilities. Higher-level health facilities should additionally be equipped to handle organophosphate poisoning emergencies.
Limitation
Our study only utilized secondary data from the DHIS2, which are limited in terms of variables available for analysis. Secondly, the study utilized information of only admitted patients, and thus outpatients and persons who did not seek care from the health facilities were excluded, resulting in an under-estimation of the incidence of organophosphate poisoning in Uganda. Community-level studies using primary data to determine the factors associated with organophosphate poisoning may be beneficial in understanding the trends of organophosphate poisoning in Uganda.
Conclusion
There was a reduction in both incidence and mortality of organophosphate poisoning among admitted persons in Uganda during 2017-2022. Males, children < 5 years, and residents of highly agricultural districts were most affected. CFRs increased with increasing administrative level of the health facility.
A detailed study into the reasons for the decline and strengthening interventions that can be directly linked to the decline nationally could facilitate continued reductions in organophosphate poisoning burden in Uganda. It is also important to build the capacity of health workers and equip lower-level health facilities to appropriately manage organophosphate poisoning incidents.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
The authors appreciate the bio-statisticians and surveillance officers who ensure that reporting of surveillance data is routinely done at their respective districts and as well as the DHIS team at the Ministry of Health for managing the DHSIS2 platform. We also appreciate Public Health Fellowship Program and the Ministry of Health, Public Health Emergency Operations Centre for the technical support and guidance offered during this study. Finally, we thank the US-CDC for supporting the activities of the Uganda Public Health Fellowship Program.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Kushwaha M, Verma S, Chatterjee S: Profenofos, an Acetylcholinesterase‐Inhibiting Organophosphorus Pesticide: A Short Review of Its Usage, Toxicity, and Biodegradation. Journal of environmental quality 2016, 45(5):1478-1489.
- Gunnell D, Eddleston M, Phillips M, Konradsen F: Worldwide patterns of fatal pesticide self-poisoning. BMC Public Health 2007, 7:357.
- Robb EL, Baker MB: Organophosphate toxicity. 2017.
- Litchfield MH: Estimates of acute pesticide poisoning in agricultural workers in less developed countries. Toxicological reviews 2005, 24(4):271-278.
- Peshin SS, Srivastava A, Halder N, Gupta YK: Pesticide poisoning trend analysis of 13 years: a retrospective study based on telephone calls at the National Poisons Information Centre, All India Institute of Medical Sciences, New Delhi. Journal of forensic and legal medicine 2014, 22:57-61.
- Ngowi AV, Maeda DN, Partanen TJ: Assessment of the ability of health care providers to treat and prevent adverse health effects of pesticides in agricultural areas of Tanzania. International Journal of Occupational Medicine and Environmental Health 2001, 14(4):349-356.
- Peter JV, Sudarsan TI, Moran JL: Clinical features of organophosphate poisoning: A review of different classification systems and approaches. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine 2014, 18(11):735.
- Malangu N: Acute poisoning at two hospitals in Kampala–Uganda. Journal of forensic and legal medicine 2008, 15(8):489-492.
- Razwiedani L, Rautenbach P: Epidemiology of organophosphate poisoning in the Tshwane District of South Africa. Environmental health insights 2017, 11:1178630217694149.
- Ecuru J, Kawooya D: Effective innovation policies for development: Uganda. 2015.
- Fowler M, Rauschendorfer J: Agro-industrialisation in Uganda. 2019.
- Ssemugabo C, Halage AA, Neebye RM, Nabankema V, Kasule MM, Ssekimpi D, Jørs E: Prevalence, circumstances, and management of acute pesticide poisoning in hospitals in Kampala City, Uganda. Environmental health insights 2017, 11:1178630217728924.
- Kwesiga B, Ario AR, Bulage L, Harris J, Zhu B-P: Fatal cases associated with eating chapatti contaminated with organophosphate in Tororo District, Eastern Uganda, 2015: case series. BMC Public Health 2019, 19:1-7.
- Pedersen B, Ssemugabo C, Nabankema V, Jørs E: Characteristics of pesticide poisoning in rural and urban settings in Uganda. Environmental health insights 2017, 11:1178630217713015.
- Sibani C, Jessen KK, Tekin B, Nabankema V, Jørs E: Effects of teaching health care workers on diagnosis and treatment of pesticide poisonings in Uganda. Environmental health insights 2017, 11:1178630217726778.
- Weerasinghe M, Konradsen F, Eddleston M, Pearson M, Jayamanne S, Gunnell D, Hawton K, Agampodi S: Vendor-based restrictions on pesticide sales to prevent pesticide self-poisoning – a pilot study. BMC Public Health 2018, 18(1):272.
- Hmouda H, Salem CB, Bouraoui K: Management of acute organophosphorus pesticide poisoning. The Lancet 2008, 371(9631):2169-2170.
- Nansikombi HT, Kwesiga B, Aceng FL, Ario AR, Bulage L, Arinaitwe ES: Timeliness and completeness of weekly surveillance data reporting on epidemic prone diseases in Uganda, 2020–2021. BMC Public Health 2023, 23(1):1-12.
- Ssempiira J, Kasirye I, Kissa J, Nambuusi B, Mukooyo E, Opigo J, Makumbi F, Kasasa S, Vounatsou P: Measuring health facility readiness and its effects on severe malaria outcomes in Uganda. Scientific reports 2018, 8(1):17928.
- UBOS: Uganda Bureau of Statistics (UBOS); Uganda National Household Survery 2014/2015. Kampala, Uganda. 2016.
- Oesterlund AH, Thomsen JF, Sekimpi DK, Maziina J, Racheal A, Jørs E: Pesticide knowledge, practice and attitude and how it affects the health of small-scale farmers in Uganda: a cross-sectional study. African health sciences 2014, 14(2):420-433.
- AUPWAE: Association of Uganda Professional Women in Agriculture and Environment:; Country Situation Report on Highly Hazardous Pesticides (HHPs) in Uganda: IPEN Toxics-free Sustainable Development Goals (SDGs). . 2021.
- Laing G, Aragrande M, Canali M, Savic S, De Meneghi D: Control of cattle ticks and tick-borne diseases by acaricide in Southern Province of Zambia: a retrospective evaluation of animal health measures according to current one health concepts. Frontiers in public health 2018, 6:45.
- Ogada DL: The power of poison: pesticide poisoning of Africa’s wildlife. Annals of the New York Academy of Sciences 2014, 1322(1):1-20.
- Loha KM, Lamoree M, Weiss JM, de Boer J: Import, disposal, and health impacts of pesticides in the East Africa Rift (EAR) zone: A review on management and policy analysis. Crop protection 2018, 112:322-331.
- Odakha JA, Harborne D, Chen H: Predictors of mortality in emergency centre patients with acute pesticide poisoning in Uganda. African journal of emergency medicine 2022, 12(3):242-245.
- Dissanayake V, Dalka ET, Koh C, Bisanzo M, Brandt RS, Erickson TB, Chamberlain S: A pilot study on the management and outcomes of self-poisoning in a rural Ugandan Emergency Centre. African journal of emergency medicine 2018, 8(1):25-28.
- Amir A, Raza A, Qureshi T, Mahesar GB, Jafferi S, Haleem F, Khan MA, Khan MA: Organophosphate poisoning: demographics, severity scores and outcomes from National Poisoning Control Centre, Karachi. Cureus 2020, 12(5).
- Farooqui WA, Uddin M, Qadeer R, Shafique K: Trajectories of vital status parameters and risk of mortality among acute organophosphorus poisoning patients–a latent class growth analysis. BMC public health 2020, 20:1-9.
- Ssemugabo C, Halage AA, Neebye RM, Nabankema V, Kasule MM, Ssekimpi D, Jørs E: Prevalence, Circumstances, and Management of Acute Pesticide Poisoning in Hospitals in Kampala City, Uganda. Environ Health Insights 2017, 11:1178630217728924.
- Lekei E, Ngowi AV, London L: Hospital-based surveillance for acute pesticide poisoning caused by neurotoxic and other pesticides in Tanzania. Neurotoxicology 2014, 45:318-326.
- UBo S: The national population and housing census 2014–main report. Uganda Bureau of statistics Kampala 2016.
- Jaga K, Dharmani C: Sources of exposure to and public health implications of organophosphate pesticides. Revista panamericana de salud pública 2003, 14:171-185.
- Muñoz-Quezada MT, Lucero B, Iglesias V, Levy K, Muñoz MP, Achú E, Cornejo C, Concha C, Brito AM, Villalobos M: Exposure to organophosphate (OP) pesticides and health conditions in agricultural and non-agricultural workers from Maule, Chile. International journal of environmental health research 2017, 27(1):82-93.
- Kumar A, Margekar SL, Margekar P, Margekar V: Recent advances in management of organophosphate & carbamate poisoning. Indian Journal of Medical Specialities 2018, 9(3):154-159.
- Geetha K, Tejas J, Vishwanathan K: Pattern of Organophosphate Poisoning in Bapuji Hospital, Davangere (2011-2013). Medico-Legal Update 2019, 19(2).
- Patil G, Murthy N, Nikhil M: Contributing factors for morbidity and mortality in patients with organophosphate poisoning on mechanical ventilation: a retrospective study in a teaching hospital. Journal of Clinical and Diagnostic Research: JCDR 2016, 10(12):UC18.
- Sekabojja D, Atuhaire A, Nabankema V, Sekimpi D, Bainomugisa C, Jørs E: Acute Pesticide Poisoning Case Registration in Uganda’s Health Care Facilities. Journal of Environmental & Analytical Toxicology 2020, 10(2).
- Yimaer A, Chen G, Zhang M, Zhou L, Fang X, Jiang W: Childhood pesticide poisoning in Zhejiang, China: a retrospective analysis from 2006 to 2015. BMC Public Health 2017, 17(1):602.
- Dayasiri KC, Jayamanne SF, Jayasinghe CY: Patterns of acute poisoning with pesticides in the paediatric age group. International Journal of Emergency Medicine 2017, 10(1):22.
- Sharma N, Nin-Gonzalez R: Organophosphate poisoning in a young child: a case report. Oxford medical case reports 2021, 2021(2):omaa137.
- Lekei E, Ngowi AV, London L: Acute pesticide poisoning in children: hospital review in selected hospitals of Tanzania. Journal of toxicology 2017, 2017.
- Roberts JR, Karr CJ, Health CoE, Paulson JA, Brock-Utne AC, Brumberg HL, Campbell CC, Lanphear BP, Osterhoudt KC, Sandel MT: Pesticide exposure in children. Pediatrics 2012, 130(6):e1765-e1788.
- Roschinsky R, Mulindwa H, Galukande E, Wurzinger M, Mpairwe D, Okeyo A, Sölkner J: Pasture use and management strategies in the Ankole pastoral system in Uganda. Grass and Forage Science 2012, 67(2):199-209.
- Mayanja S, Akello B, Horton D, Kisauzi D, Magala D: Value Chain Development in Uganda: Lessons Learned from the Application of the Participatory Market Chain Approach. BANWA 2013, 9:64-96.
- Lunner-Kolstrup C, Ssali TK: Awareness and need for knowledge of health and safety among dairy farmers interviewed in Uganda. Frontiers in public health 2016, 4:137.
- Bawuyo N: A report of industrial training carried out in Kortek sub-county, Bukwo district local government. 2019.
- Cheptoyek H: Knowledge, attitude and practices on pesticide use and safety among smallholder farmers in Chemwabit parish, Bukwo district. Makerere University; 2019.
- Namazzi G, Waiswa P, Nakakeeto M, Nakibuuka VK, Namutamba S, Najjemba M, Namusaabi R, Tagoola A, Nakate G, Ajeani J: Strengthening health facilities for maternal and newborn care: experiences from rural eastern Uganda. Global health action 2015, 8(1):24271.
- Ningwa A, Muni K, Oporia F, Kalanzi J, Zziwa EB, Biribawa C, Kobusingye O: The state of emergency medical services and acute health facility care in Uganda: findings from a National Cross-Sectional Survey. BMC Health Services Research 2020, 20(1):1-10.

