Measles outbreak and associated risk factors for measles transmission in Kamuli district, July 2016
Authors: Lydia Nakiire1,2, Paul Okello1, Fred Nsubuga1,4, Issa Makumbi2, Joan Kalyango5, Alex R. Ario1; Affiliations: 1Public Health Fellowship Program, Field Epidemiology Track, Kampala, Uganda, 2 Public Health Emergency Operation Center, 3Centers for Disease Prevention and Control , 4Uganda National Expanded Program on Immunization, 5Makerere University college of Health sciences
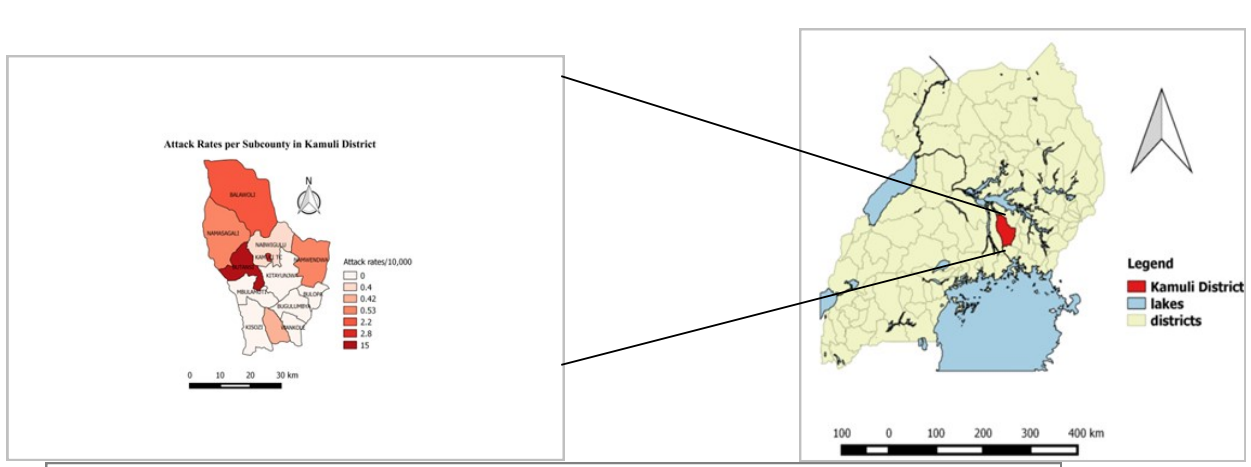
Summary: The Ministry of Health was notified of a measles outbreak in Kamuli district on 11th July, 2016. We conducted an investigation to establish the scope of and risk factors for the outbreak, estimate district measles vaccine effectiveness and vaccine coverage. We estimated the vaccine efficiency and measles coverage and in a case control study we compared exposures of 25 cases individually matched by age and village of residence with 100 asymptomatic controls. Children under 5years had the highest attack rates (5.3/ 10,000) compared to those 5 years and above (1.1/10,000). Butansi Sub County was the most affected (15cases/10,000 population). Lack of prior measles vaccination was associated with measles cases (ORMH= 6.8, CI: 1.8- 25). The estimated vaccine effectiveness was 82% and district immunization coverage was 58%. Lack of prior measles vaccination caused the measles outbreak. Measles vaccination coverage was lower than the recommended 90% national coverage. We recommend intensification of measles vaccination in the district.
Introduction: Measles has been targeted for elimination due its high public health impact on families. Measles can lead to hospitalization and loss of work hours. In Uganda, Measles control has been implemented through routine vaccination which begun in early 1980’s, three year measles supplemental immunization since 2003 and case based surveillance (MOH 2015). Despite all these efforts there have been outbreaks reported in western and central districts in the country. In the recent past, the outbreak has spread to other parts of the country including Eastern Uganda. Analysis of Kamuli district measles data showed that there were reported 1-2 cases per month since January 2016 but in May 2016 there was an increasing trend of 3-4 cases per month. The alert to Ministry of Health on 5th July 2015 indicated that the suspected cases mainly presented with fever, generalized skin rash, red eyes and cough. On 11th July, 2016, the PHEOC was notified of a measles outbreak in Kamuli District located in Eastern Uganda. The outbreak was con- firmed when 5 out of 8 samples taken to the Uganda Virus Research Institute tested positive for measles IgM antibodies. We investigated the outbreak in order
to establish the scope of the measles outbreak, determine risk factors for transmission, control
Methods: We defined a suspected case as any resident of Kamuli with fever and generalized skin rash lasting for 3 or more days with at least one of the following: cough, coryza and conjunctivitis since 1st June, 2016; and a confirmed case as any suspected case with positive measles IgM antibodies laboratory test. A control was any person who did not have signs and symptoms of measles and not living in the same household with a case patient. We conducted active case finding by records review at health and schools.
With the help of Village Health Teams, we conducted community case finding.We line listed 72 case patients with no deaths. We interviewed 31 suspected cases for hypothesis generation.
We conducted a case control study among 25 cases and 100 controls individually matched by age and village of residence.
We conducted a case control study among 25 cases and 100 controls individually matched by age and village of residence. We estimated the vaccine effectiveness
Results: Children under 5 were most affected. No adults were affected in the outbreak. Males and females were equally affected with the attack rate of males slightly higher than that of females. ( table 1). Butansi sub-county was the most affected rate of 15/10000, followed by Kamuli Municipal Council with attack rate of 2.8/10000 as shown in figure 1.

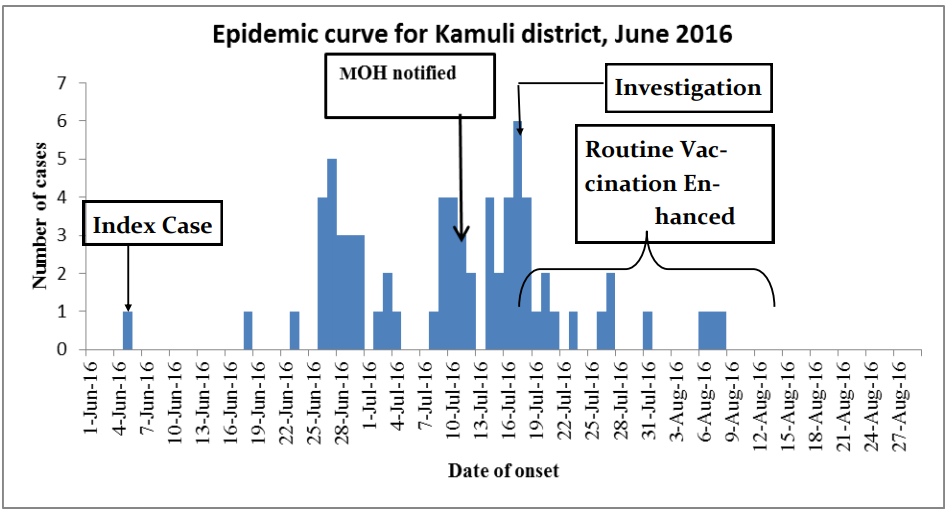
The epidemic curve shows a propagated outbreak with the index case occurring on 5th June 2016. (figure 2). The probable index case was a 3 year old male from Buleta village, Bugeywa parish in Butansi subcounty. Successive peaks are observed on 27/06/16 and 17/07/16 with higher prevalence in each successive cluster.
Case control study findings: A case control study among 25 cases and 100 controls , ratio 1:4, revealed that not being vaccinated was associated with the measles. 21/25 (84 %) of case- patients and 51/100 (51%) of controls having measles, ORMH = 6.8, 95% 1.8-25) as shown in table 2: Visiting a school or church during the effective exposure period was associated with the diseases though this was not statistically significant.
Vaccination coverage: The proportion of cases line listed who were vaccinated was 12/71 (17 %). We computed the proportion of population vaccinated (PPV) using population of cases vaccinated (PCV) and assumed vaccine efficacy (VE) 85%.
PPV = PCV/(1-PCV) * VE
Assumptions made: the vaccination rate in case patients with unknown vaccination history was the same as in case patients with known vaccination history, ii) the case patients with un- known vaccination status were not vaccinated. The Proportion of population vaccinated (PPV) was 58%. This low vaccination coverage compared to the recommended target of 90%.
Vaccine effectiveness (VE) = (1-RR)* 100
ORMH (odds of vaccinated/ odds of unvaccinated in rare disease) ≈ RR
VE = (1-0.18 )* 100 = 82%
*Fishers exact 95% Confidence Intervals, MH-Mantel Henzel

Discussion: Children under-five years were the most affected in this outbreak. This is consistent with results from studies done in India (Bhuniya 2013, Sudipta 2015) . The reasons for the highest attack rate in this age group could be because of the diminishing maternal antibodies in children between 6 – 9 months. Children above 9 months could have missed getting vaccinated during the routine EPI scheduled vaccination at 9 months. These contribute to a pool of susceptible children who reduce the heard immunity of the population and thus out breaks. (Bhuniya 2013, Sudipta 2015). There was low vaccination coverage in this study compared to the target for Kamuli District at 90%. This is consistent with several studies done in developing countries which often show vaccine coverage computed during outbreaks being lower and probably more accurate than the administrative coverage. The very low vaccination coverage means there is no herd immunity in this population thus the out- break .
Conclusion and recommendations: Lack of prior measles vaccination, low vaccination coverage and low vaccine effectiveness propagated this outbreak. The vaccination coverage is too low to confer any protection to the population. Intensify routine immunization services at the health facility and community outreaches. All health facilities should offer vaccination daily. Pay more attention to the quality of data used in calculating administrative coverage in the district
References:
Bhuniya, e. a. (2013). "Measles outbreak among the Dukpa [17]tribe of Buxa hills in West Bengal, India: epidemiology and vaccine efficacy. Indian Journal of Public Health. ." Indian Journal of P ublic Health 57: 272-275. MOH (2015). Measles supplemental immunization activities, rollout of human Papilloma virus vaccine and introduction of inactivated polio vaccine. UNEPI, MOH. Sudipta, E. A. B. (2015). "Root-Cause Analytical Survey for Measles Outbreak: Vaccination or Vaccine?- A Study From Madhepura District, Bihar, India." Journal of Clinical and Diagnostic Research : JCDR 9(6): SC04-SC07.


Comments are closed.