Malaria Outbreak in Nwoya District, April 2018
Authors: Godfrey Nsereko1, Denis Okethwangu1, Joyce Nguna1, Dan Kadobera1, Alex Riolexus Ario1; Affiliation: Uganda Public Health Fellowship Program-Field Epidemiology Track
Summary
Malaria is still a major cause of ill-health and deaths globally. On 18 April 2018, the Health Officer (DHO) of Nwoya district reported an upsurge in the number of malaria cases, which exceeded action thresholds. The Ministry of Health (MoH) set up a response team to determine magnitude of the outbreak, identify risk factors for transmission, and recommend evidence-based control measures. We defined a confirmed case as a positive test result of Plasmodium falciparum by Rapid Diagnostic Test or microscopy from 1-02-2018 to 25-05-2018 in a resident or visitor of Nwoya District.
We reviewed outpatient data in all health facilities. In a case control study we compared potential exposure risk factors between 107 case-persons and 107 asymptomatic controls matched by village. We conducted entomological assessment on vector density and behavior, and assessed household environment. We line-listed 4,750 confirmed case-persons and 2 deaths. The attack rate (AR) was higher in females (69/1,000) than in males (36/1000); children ≤5 years had the highest AR (77/1000). The overall AR was 65/1000.
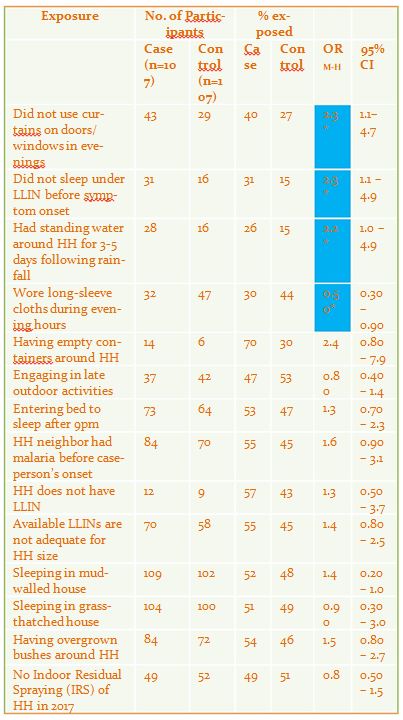
The epidemic curve showed a propagated outbreak beginning in late March after start of heavy rains. 29% (31/107) of case-persons and 15% (16/107) of controls were not sleeping under a Long Lasting Insecticide-treated Net (OR=2.3,95%CI=1.1-4.9); 40% (43/107) of case-persons and 27% (29/107) of controls did not use curtains on doors and windows during evenings (OR=2.3, 95%CI=1.1-4.7); 26% (28/107) of case-persons and 16% (16/107) of controls had standing water around households for 3-5 days following rainfall (OR=2.2, 95%CI=1.0-4.9). 30% (32/107) of case-persons compared with 44% (47/107) of controls wore long-sleeve cloths during evening hours (OR=0.54, 95% CI=0.30-0.96).
Anopheles gambiae sensu latu species was the predominant vector. Indoor resting density was 4 vectors/household/ night and the container larval density was 17%. Heavy rains that caused flooding precipitated the outbreak. Not implementing protection measures against mosquito bites were exposure risk factors. We recommended health education on protection measures against mosquito bites; larviciding active breeding sites.
Background
Uganda ranks sixth among high mortality malaria rates in Africa, and has one of the highest reported malaria transmission rates in the world. Plasmodium falciparum, which accounts for 99 % of the cases (MoH, 2014), is the dominant parasite species .Anopheles gambiae, a highly efficient vector, along with Anopheles funestus are the two main vectors. These vectors are predominantly anthropophagic (feed exclusively on humans), endophilic (rest indoor) and endophagic (feed indoor) Malaria transmission in Uganda exhibits seasonality based on the rainfall patterns. On 18 April 2018, the Health Officer of Nwoya District reported to the National Malaria Control Program an up surge in the number of malaria cases that had exceeded the action thresholds. Two sub-counties (Anaka, Koch-Goma and Anaka T/C) reported the highest number of confirmed malaria cases in the district. The Ministry of Health set up a response including officials from the Uganda Public Health Fellowship Program (PHFP), and Nwoya District Health Office to investigate this upsurge. We aimed to determine magnitude of the outbreak, identify risk factors for transmission, and recommend evidence-based control measures.
Methods
We defined a confirmed case as a positive malaria result on mRDT or microscopy from 1 February, 2018 onwards in a resident or visitor of Anaka Sub-county, Koch Goma Sub-county and Anaka Town council in Nwoya District, Uganda. We found cases by reviewing outpatient health records by reviewing outpatient health records in health facilities in the affected sub counties. In the case-control study, we compared potential exposures between 107 case-persons and 107 asymptomatic controls matched by neighborhood. We determined vector density and behavior using the Pyrethrum Spray Catch (PSC) method. PSC was done daily in randomly selected houses between 24th and 28th May 2018, from 7:00am and 12:00pm. Consent was obtained from households and the procedures explained to the house owners. We also conducted larval scooping in swamps and water-logged areas to identify both active and potential breeding sites. We examined environmental and human exposure factors that may have catalyzed the upsurge in malaria cases during the period.
Findings
We line listed 4,750 confirmed case-persons. Of all confirmed case-persons, 3115 (66%) were women. Two deaths from severe malaria were identified during the period in the district.
Among the line listed cases, females, an attack rate (AR) of 69/1,000 compared to males (AR=36/1,000). Children less than 5 years of age had an attack rate of 77/1,000 and were the most affected age group while adults above 25 years (32/1000) of age were least affected.
The overall attack rate for the 3 sub-counties was 65/1000. Anaka Sub-county was the most affected (AR = 84/1,000) followed by Anaka Town Council (AR=63/1,000) and Koch Goma Sub-county with an attack rate of 57/1,000.
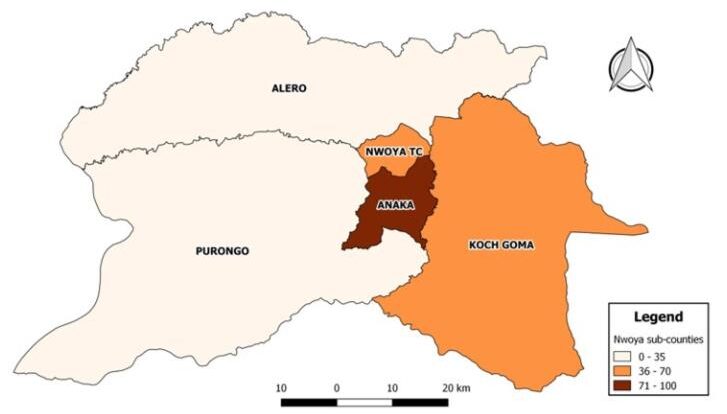
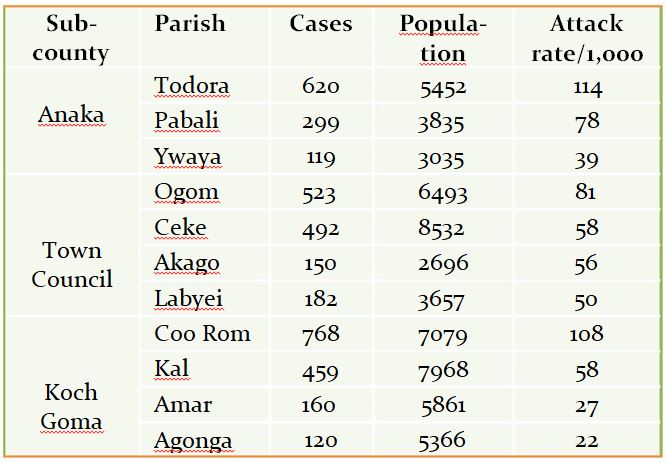
Among parishes, Todora parish in Anaka Sub-county had the highest attack rate (114/1,000), followed by Coo Rom parish (AR=108/1,000) in Koch Goma Sub-county and Ogom Parish (81/1,000) in Town Council.
Table 1: Distribution of cases by Parish
The epidemic curve is propagated and shows an increase in malaria cases from late March. The upsurge occurred about 4 weeks after the first rains occurred

Adult Vector Density, Larval Density and Indoor Resting Density
The assessment shows malaria vectors Anopheles gambie sensu lato and Anopheles funestus as the most common vectors found inside the sampled households. The average indoor resting density (IRD) of malaria vectors was found to be 4 mosquitoes per household per night. Anopheles gambiae sensu latu species had a higher indoor resting density (IRD=2.3) than Anopheles funestus species (IRD=1.4). A search for potential and active breeding sites for malaria vectors showed a container larval density of 17%.
Case-Control Study
Not sleeping under a LLIN, not drawing curtains on doors and windows, and presence of water logging areas for 3-5 days following rainfall were significantly associated with malaria infection, with the odds of >2. Wearing long clothes during evening hours was significantly protective against malaria infection.
Table 2: Exposure Status among Cases and controls
Discussion
There was a strong seasonal transmission pattern with peaks observed from late March throughout April during the heavy rainfall period. Nwoya District has over the years experienced heavy rainfalls during the period from March to May (worldweatheronline, 2018). Malaria case data reveals a corresponding increase in cases 4-5 weeks following the first episodes of rainfall. During the rainfall periods, temporary pools of water are formed in areas with swamps, open abandoned containers, ditches and potholes along the road side among others. In 2017, a lesser upsurge of malaria cases was observed during the same period following Indoor Residual Spraying (IRS) in the district. Our findings in this study point to no significant protection of IRS sprayed households and a high indoor resting density of malaria vectors. The potency of the last IRS diminished 6-9 months after spraying, thereby rendering indoor walls and surfaces of houses as convenient feeding and resting places for malaria vectors. The Uganda National Malaria Control Program, at the center of implementation of the 5 year malaria reduction strategic plan, has emphasized IVM as one of the key strategies to fast track malaria elimination (MOH, 2014, 2015). As with our findings, not sleeping under LLIN in high transmission areas is recipe for increased human-vector contact and therefore malaria disease (Srivastava and Dhariwal, 2016). Drawing of curtains on doors and windows early enough to prevent or minimize mosquito entry into the house and wearing long clothes in evening hours are simple to use and cost-effective strategies can be incorporated into routine social behavior change communication massages in the fight against malaria
Conclusion and Recommendations
Heavy rains that caused flooding precipitated the outbreak. Not implementing protection measures against mosquito bites were exposure risk factors We recommended health education on protection measures against mosquito bites; larviciding active breeding sites
References
- MoH (2014) UGANDA Malaria Indicator Survey (MIS). Available at: https://dhsprogram.com/pubs/pdf/mis21/mis21.pdf (Accessed:
3 May 2018).
- MOH, M. of H. (2014) THE UGANDA MALARIA REDUCTION STRATEGIC PLAN 2014-2020.
- MOH, M. of H. (2015) ‘Health Sector Development Plan 2015/16 – 2019/20’, RoU, (September), p. 110. doi: 10.1093/intimm/dxu005.
- Srivastava, P. and Dhariwal, A. (2016) Compendium On Entomological Surveillance & Vector Control in India. Available at: http://
nvbdcp.gov.in/Doc/Compendium-Ent.VC-DrPKS.pdf (Accessed: 7 June 2018).
- worldweatheronline (2018) Nwoya, Gulu, Uganda Weather Averages | Monthly Average High and Low Temperature | Average Precipi-
tation and Rainfall days | World Weather Online. Available at: https://www.worldweatheronline.com/nwoya-weather-averages/gulu/ug.aspx (Accessed: 7 June 2018).


Comments are closed.