Malaria Outbreak in Kisooro District, January, 2018
Authors: Joyce Nguna1, Denis Okethwangu1, Daniel Kadobera1 Affiliation: 1 Uganda Public Health Fellowship Program
Summary
Malaria is a febrile illness liable for high morbidity and mortality worldwide. Analysis of DHIS2 data revealed an upsurge in malaria cases in Kisoro District in December 2017 and January 2018. We investigated this outbreak to determine its extent, identify risk factors, and recommend control and prevention measures. We reviewed health records from June, 2017 to January, 2018 in all health facilities in the 2 most affected sub-counties. In a case control study we compared potential exposures between 145 case-persons and 145 asymptomatic controls matched by age and village. We carried out an entomological and environmental assessment in affected sub counties. Persons older than 5 years of age were the most affected. 22% (32/145) of case-persons and 15% (21/145) of control-persons reported not sleeping under a mosquito net (ORM-H=4; 95%CI=1.2-1.3) in Chibumba village; 89% (129/145) of case-persons and 73% (106/145) of control-persons were bitten by mosquitoes before bed time ORM-H=2.9; 95%CI=1.6-5.7). Anopheles gambiae sensu lato was the dominant identified species. We recommend increased sensitization and further entomological investigations to ascertain vector bionomics.
Introduction
Despite significant progress in scaling up malaria control interventions, malaria remains one of the most important global health challenges accounting for high morbidity and mortality. Malaria is highly endemic in about 95% of Uganda and is the leading cause of attendance at health facilities [8]. Transmission is unstable and epidemic-prone in extreme south-western areas around Rwenzori mountains, Mt. Elgon in the east and areas extending above 1,800 meters in altitude. Kisoro is one of the highland areas in Uganda with a low malaria prevalence of 12% [8]. A detailed investigation and understanding of the factors impacting increase in Malaria cases in Kisoro was crucial to improve well targeted malaria control strategies.
Methods
We defined a confirmed case as any positive malaria test result from mRDT or microscopy from 1st June, 2017 to 27 January, 2018 in a resident or visitor of Kisoro District. We systematically searched for malaria cases by reviewing health records in all health facilities in the 2 most affected sub-counties of Kanaba and Murora. In a case-control study we compared potential exposures between 145 case-persons and 145 asymptomatic controls matched by age and village. We carried out an entomological and environmental assessment of the affected sub counties.
Results
We line listed 2,720 malaria case-patients with a median age of 19 years (IQR 10-30).
Person characteristics
| Age Group | Frequency | Population | AR/1000 |
| <5 | 317 | 7,692 | 41 |
| 5-18 | 1023 | 15,383 | 67 |
| >18 | 1380 | 19,657 | 70 |
| Total | 2720 | 42,732 | 100 |
Table 1: Distribution of cases by age group
Persons older than 18 years old were most affected, closely followed by those between 5 and 18 years old.
| Sub county | Parishes | Cases | Population | Attack Rate/1000 |
| Kanaba | Kagezi | 832 | 8,619 | 97 |
| Muhindura | 159 | 10,148 | 16 | |
| Murora | Chahafi | 485 | 13,149 | 37 |
| Chibumba | 1211 | 10,816 | 112 |
Table 2: Distribution by Parish
Place characteristics
Chibumba Parish had the highest attack rate per 1000 population (112), followed by Kagezi (97), Chahafi (37) and Muhindura (16) parishes (Table 2). In Kagezi, Butoke had the highest attack rate (329/1000 population) followed by Mukaka and Kooga villages with 156 and 146 respectively. In Chibumba Parish, two villages; Chibumba (337/1000) and Mpundu (314/1000) were the most affected.
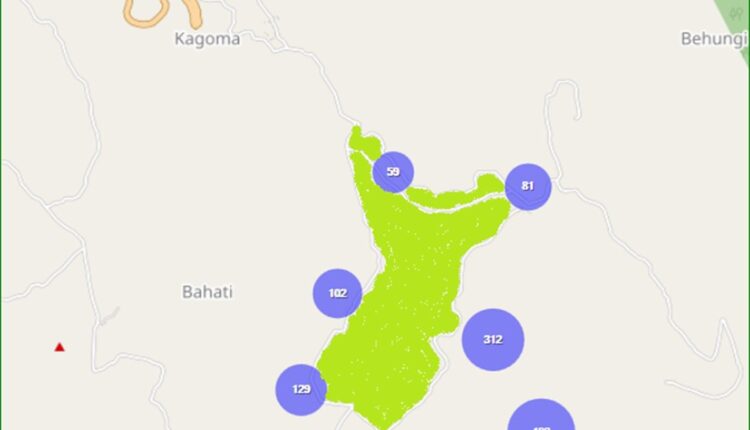
Mpundu, Chibumba, Butoke, Mukaka and Kooga villages around Sereri swamp contributed 60% of all the con- firmed cases in the 2 most affected sub-counties.
Time characteristics
There was a marked increase in the number of malaria cases in December and January (Figure 3). There has been continuous transmission since September 2017 and is bound to continue if transmission is not broken. The epicurve is indicative of a continuous common source pattern with waves of transmissions that have kept in creasing since November 2017.
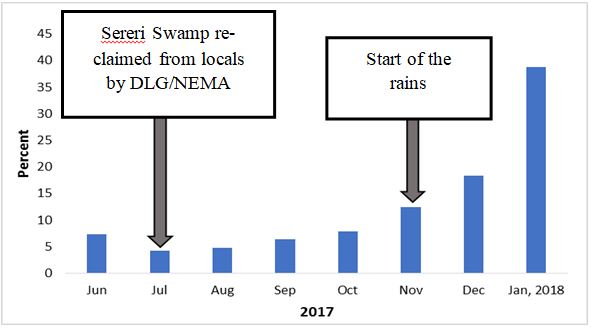
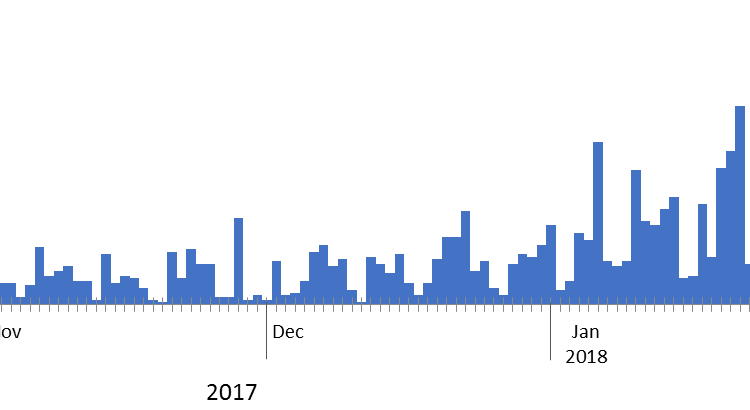
Figure 3: Epidemic curve showing cases in the most affected months of November, December 2017 and January 2018.
Environmental and entomological assessment: The villages in these sub-counties with high malaria trans- mission; Mpundu, Chibumba, Kooga, Butoke, Mukaka are located on hills around the Chibumba-Sereri wet- land. This swamp an extensive lowland into which run off water from the hilly villages affected by the outbreak drains. Communities have encroached on the wetland to carry out farming and brick activities thus creating suitable breeding sites of malaria (Appendix 1). Stagnant water in brick pits and garden trenches in the swamp were the major breeding sites of Anopheles. Temporary breeding sites which depended on continuous rains were road- side pools and tyre-tracks on feeder roads. Anopheles gambiae sensu lato was the only vector identified from the Pyrethrum Spray Catches (PSC). Low adult catches were observed by the assessment.
Case control results: Not sleeping under a mosquito net and mosquito bites before bed time were significantly associated to malaria infection. The odds for malaria infection were 3 times higher if the person was bitten by mosquitoes before bed time (ORM-H: 2.9, CI: 1.6 – 5.7) and 4 times higher if one was not sleeping under a mosquito net (ORM-H: 4, CI: 1.2 – 1.3) in Chibumba village.
| Exposure | Cases (n=145) | Control (n=145) | Cases | Controls | ORM-H |
| Not using mosquito net | 32 | 21 | 22 | 15 | 1.7 (0.94 –3.06 ) |
| Chibumba village | 14 | 05 | 39 | 14 | 3.9 (1.2-13) |
| Mosquito nets before bed time | 129 | 106 | 89 | 73 | 2.9 (1.6 –5.7) |
| History of sick in | 86 | 73 | 59 | 50 | 1.4 (0.91 –2.3) |
| household Entering bed after 9:00pm | 109 | 113 | 76 | 78 | 0.91 (0.52–1.6) |
| Travel history | 8 | 6 | 5.5 | 4.1 | 1.4 (0.45 –4.3) |
| Wearing long clothes | 38 | 39 | 26 | 27 | 0.96 (0.57– 1.6) |
| Outdoor activities | 56 | 69 | 39 | 48 | 0.69 (0.43– 1.2) |
Discussion
This investigation revealed that there is continuous transmission of malaria in Kisoro District which peaked in late 2017 and early 2018. High malaria transmission is evident among villages of Mpundu, Chibumba, Kooga, Butoke, Mukaka located at the slopes of hills around the Chibumba-Sereri wetland. It’s propagated by favorable vector breeding sites located within the affected sub-counties due to human activity in the swamp specifically brick making and agriculture. These pro- vide favorable breeding sites for the anopheles mosquito whose population has steadily increased in the affected areas over time. Homes in the affected sub-counties receive returnees for the Christmas holidays from early November till end of December, many of which are from high malaria endemic areas in Uganda. These easily provide the source for malaria parasites for the anopheles mosquito to transmit. In other areas of Uganda where Anopheles gambiae is largely endophilic, the low adult catches by PSC suggests few mosquitoes rest indoors perhaps due to hot conditions facilitated by iron sheet roofs for the houses. This points to the possibility of changes in vectors behaviors, mutation or , changes in the known vector dynamics of biting humans.
Conclusion and Recommendations
To ascertain the true vector feeding and resting behavior de- tailed bionomic studies have to be conducted using different adult collection methods. Conducting molecular characterization of the An. gambiae s.l is key. Community mass action to fill such small pools could be used by environmental health officers through initiating and promoting participation of area residents. Larviciding can be effective in the garden trench pools.
References
- O’Meara, P., et al., Changes in the burden of malaria in sub-Saharan Africa. The Lancet infectious diseases, 2010. 10(8): p. 545-555.
- Protopopoff, N., et al., Ranking malaria risk factors to guide malaria control efforts in African PLoS One, 2009. 4(11): p. e8022.
- Lindsay, S. and W. Martens, Malaria in the African high- lands: past, present and future. Bulletin of the World Health Organization, 76(1): p. 33.
- Koram, , et al., Socio-economic risk factors for malaria in a peri-urban area of The Gambia. Transactions of the royal soci- ety of tropical medicine and hygiene, 1995. 89(2): p. 146-150.
- Lindblade, K.A., et al., Highland malaria in Uganda: prospective analysis of an epidemic associated with El Nino. Transac-tions of the Royal Society of Tropical Medicine and Hygiene, 1999. 93(5): p. 480-487.
- Lindblade, K.A., et al., Land use change alters malaria transmission parameters by modifying temperature in a highland area of Uganda. Tropical Medicine & International Health, 2000. 5(4): p. 263-274.
- Okello, P.E., et al., Variation in malaria transmission intensity in seven sites throughout Uganda. The American journal of tropical medicine and hygiene, 2006. 75(2): p. 219-225.
- Yeka, A., et al., Malaria in Uganda: challenges to control on the long road to elimination: I. Epidemiology and current control efforts. Acta tropica, 2012. 121(3): p. 184-195.

