Cholera Outbreak in Kyangwali Refugee Settlement in Hoima, Uganda, 2018
Authors: Fred Monje1, Kenneth Bainomugisha1, Daniel Kadobera1, and Benon Kwesiga1; Affiliations: 1Uganda Public Health Fellowship Program, Kampala, Uganda
Summary
On 15 February 2018, Uganda Ministry of Health (MoH) was notified of 3 suspected cholera deaths in Kyangwali refugee settlement, Hoima District, Western Uganda. Following the alert, the MOH confirmed Vibrio cholerae by culture and declared a cholera outbreak on 23 February 2018. On 24 February, 2018, we conducted an investigation to determine the scope of cholera outbreak; identify possible exposures; and recommend evidence-based control measures. The case fatality rate was 2.2% and Kyangwali sub-county was the most affected with attack rate of 16/1,000 case-patients. We conducted a frequency matched case-control study and found that stream water was associated with cholera outbreak. We recommended increased access to safe water in all affected communities.
Introduction
Cholera is a preventable acute diarrhoeal disease caused by infection of the intestine with the bacterium Vibrio cholerae serogroup O1 or O139. Cholera is usually transmitted through consumption of water or food contaminated by feaces bearing the cholera causing organism. About 20% of those who are infected develop acute, watery diarrhoea and 10–20% of these individuals develop severe watery diarrhoea. The incubation period is very short (2 hours to 5 days) and thus the number of cases can rise quickly. If these patients are not promptly and adequately treated, the loss of such large amounts of fluid and salts can lead to severe dehydration and death within hours (Pande et al., 2018, Ali et al., 2017).
On 15 February 2018, Uganda Ministry of Health was notified of 3 suspected cholera deaths in Kyangwali refugee settlement, Hoima District. The signs and symptoms presented before death were vomiting, fever and acute watery diarrhea. 70% (7/10) of stool samples from the patients tested positive for Vibrio cholerae by culture. We conducted an investigation to determine the scope of cholera outbreak; identify possible exposures; and recommend evidence-based control measures.
Methods
We defined a community case as onset of watery diarrhoea in a person in Hoima District since 1 February, 2018; suspected case as onset of watery diarrhoea in a person aged ≥2 years in the Hoima District since 1 February, 2018; a confirmed case had Vibrio cholerae serogroup O1 or O139 isolated by culture from the stool sample. We found cases by vising affected communities, reviewing and updating line lists at cholera treatment centres. We conducted a descriptive epidemiology by person, place and time. We then conducted a case control study where we compared exposure factors among cases and
controls. We interviewed case-persons about their water sources. We also conducted environmental assessment of the refugee settlement regarding water sources, and sanitation, and tested water samples for pathogen identification.
Results
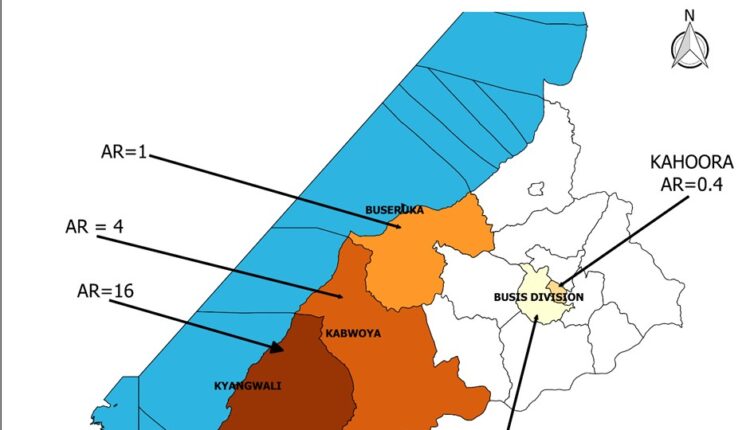
Person: We line listed 1,625 case-patients, with a case fatality rate of 2.2% (36/1625) as of 12 March 2018. The attack rates per 1000 persons by sex in Maratatu village in Kyangwali sub-county were 1.9 for males and 2.2 for females. The age-specific attack rates (/1000) for 0-9 years was 1.5; 10-19 years was 2.5; 20-39 years was 0.86; 40-59 years was 6.3; and >60 years was 0.21. Place: The attack rate per sub-county was 16 per 1000 persons in Kyangwali; 4 in Kabwoya and 1 in Buseruka (see
figure 1).
Time:
The first case-patient occurred on 11th February, 2018 and progressed to a peak on 17th February, 2018 before declining down to a minimum on day 20th. Thereafter, the case- patients picked up until another peak on 22nd and later declined to its minimum on day, 23rd. Other peaks were observed on day 25th and day, 28th as shown on the epi- curve.
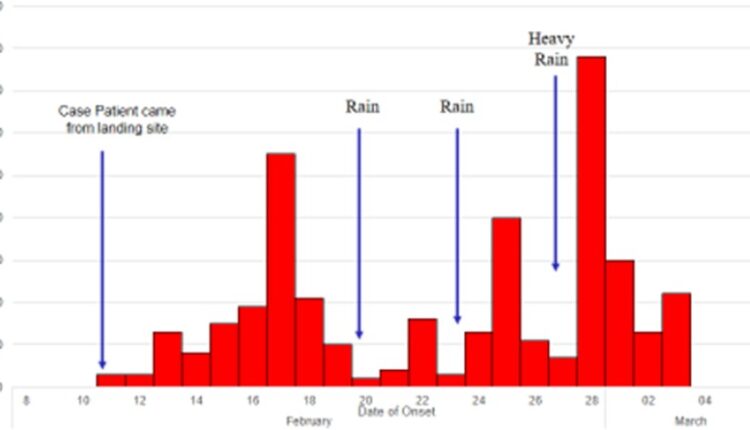
The epidemic curve indicates a continuous common source outbreak sustained by rains that washed fecal matter into the stream water.
Environmental assessment: There was evidence of open defecation near the stream water during environmental assessment in Maratatu (Figure 3). Stream water testing revealed presence of faecal coliforms. In hypothesis generation, we considered the known facts about the outbreak such as mode of transmission of cholera, the incubation period, case-patients, the areas most affected, the duration of the outbreak and the pattern of the outbreak. On conducting hypothesis generation interviews of 14 case-patients in Maratu B and C, we found out that 71% (10/14) case-patients drank stream water.
Case control study: In a case control study, 63% (46/73) case- households drank stream water compared to 43% (46/107) con- trol-households (matched odds ratio [MOR] = 2.5; CI: 1.2 – 4.9). 1.4% (1/73) case-households drank spring water compared to 13% (14/107) control-households (matched odds ratio [MOR] = 0.13; CI: 0.016 – 1.).
Discussions
The cholera outbreak we investigated was the fifth such out- break in Hoima District and the third in Kyangwali Sub-county since 2012. As of 12 March, 2018, 1625 case-patients had been identified with 36 deaths (CFR=2.2%). Our epidemiologic and laboratory investigation and environmental assessment revealed that the outbreak was caused by drinking contaminated stream water. The influx of refugees on 5 February, 2018 from the neighboring Democratic Republic of Congo (DRC) constrained water and latrine resource utilization in Kyangwali Sub-county.
Consequently, open defecation was evident along the stream and easily washed by the rains thereby intermittently contaminating the water source. This rendered stream water unsafe for direct drinking. Cholera outbreaks had occurred multiple times in Hoima District since 2012. Our findings could shed light on why cholera outbreaks repeatedly occurred in this fishing community and provide evidence based solutions. The first case-person was a refugee from DRC (where a cholera outbreak was reportedly on- going) suggesting that he might have contracted the disease from DRC.
After cholera was introduced into the refugee com- munity, open defecation, unsafe drinking water, poor hygiene, and rains likely aided the spread of cholera in the refugee com- munity. In previous outbreaks, unsafe water and cross-border activities were also listed as possible exposures. These risk factors still exist in the area; hence new outbreaks could again occur in the future if they are not attended to. After the first refugee case was confirmed, the refugees have continued coming to Uganda thereby posing further threats. During this outbreak, even though cholera outbreaks were occurring on both sides of the border, there was no information exchange between Uganda and DRC geared towards joint control efforts of the Outbreak.
Enhanced coordination from both countries is necessary for future preparedness, early detection, and response to disease out-breaks along the albertine border districts.
Conclusions and Recommendations
Our investigation revealed that the refugee influx might have introduced cholera into the Kyangwali refugee community. Consequently, drinking unsafe stream water (not treated or boiled) contaminated by feaces that was washed by the rains, aided transmission of Cholera, resulting into a prolonged cholera out- break. We recommended to the district and ministry of health to increase access to safe water supply in all affected communities. We also conducted health education of the communities to effect behavioral change towards latrine usage.
References
- Bwire, , et al. (2017). “Identifying cholera “hotspots” in Uganda: An analysis of cholera surveillance data from 2011 to 2016.” PLoS Negl Trop Dis 11(12): e0006118.
- Kwesiga, , et al. (2018). “A prolonged, community-wide cholera outbreak associated with drinking water contaminated by sewage in Kasese District, western Uganda.” BMC public health 18(1): 30.
- Wright J, Gundry S, Conroy R. Household drinking water in developing countries: a systematic review of microbiological contamination between source and point-of-use. Tropical Med Int 2004;9(1):106–17.
- Pons W, Young I, Truong J, Jones-Bitton A, McEwen S, Pintar K, Papadopoulos A. A systematic review of waterborne disease outbreaks associated with small non-community drinking wa- ter Systems in Canada and the United PLoS One. 2015;10(10):e0141646.
- Taylor DL, Kahawita TM, Cairncross S, Ensink JHJ. The im- pact of water, sanitation & hygiene interventions to control cholera: a systematic review. PLoS One. 2015;10(8):e0135676.

