Investigation of Suspected Guinea Worm Outbreak, Isingiro district, 2016
Authors: Allen Eva Okullo1, Susan Nakubulwa1, Alex R. Ario1; Affiliations: 1Uganda Public Health Fellowship Program
Background
On 30th May 2016, a suspected case of guinea worm was reported from Nakivale HCIII in Isingiro district. The suspected case was reported to have come from Nakivale refugee settlement in Isingiro district. It was believed that many more cases could be within the community. Two residents of the Uganda Public Health Fellowship Program –Field Epidemiology Track supervised by the Field Coordinator set out to conduct an epidemiological investigation to confirm the outbreak, determine the extent of the out- break; establish the source and risk factors for transmission. Findings from the study would inform evidence based interventions.
Meeting DHT and Health Facility Staff
The team met the District Health Officer, District Surveillance Focal Person and the Vector Control Officer of Isingiro District and obtained the following information: The initial suspected case, a male, had an incision performed to remove the ‘worm’ suspected to be in the position of the lesion but no worm was seen; the second suspected case was a female whose worm-like lesion on the foot was noted to shift in position (1-2cm). The Nakivale HC III clinicians corroborated the report by DHO.
The initial suspected case reported to Nakivale HCIII on 30th May. Incision was done but no worm seen. Albendazole was prescribed and administered. The Clinical Officer reported having seen 4 cases within the past 2 months with similar skin lesions mainly on the lower foot. Incisions were done on all 4 cases and no worms seen. All 4 cases did not report other related symptoms.
Case Investigation
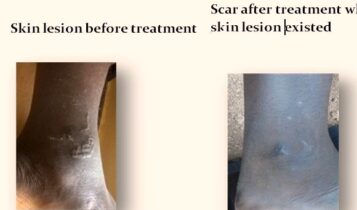
We interviewed two suspected cases (adults) and the parent of the third suspected case (9month baby) at Nakivale Refugee Settlement where all the reported cases were. First suspected case: a 21yr old male farmer living in Kabazana village; was not wearing shoes at the time prior to when he developed the skin lesion, now wears gumboots. Prior to the lesion appearing, he experienced a jigger like itch on the lower leg on 25th May which made him scratch the area affected. The ‘worm-like’ lesion appeared on 27th May and as he continued to scratch the area, the lesion moved in position by about 1-2cm. He had no other symptoms such as diarrhea, nausea and abdominal pain. He visited Nakivale HCIII on 30th May, three days after the appearance of the lesion. The clinical staff made an incision on the affected area and failed to identify any worm. He was given albendazole at the facility, skin lesion dried up 3days after visiting the facility. A scar remains in the area that previously had the lesion.
Second suspected case: a 38yr old female peasant living in Kabazana Village, was not consistently wearing shoes at the time prior to when she developed the skin lesion, itching on the toes of the right leg started about 3 months ago soon after a ‘worm-like’ lesion appeared on the toes along with an ulcer, the lesion kept migrating from the toes to an area close to the ankle, itching persisted.
She had no other symptoms such as nausea, diarrhea and abdominal pain. She made an incision on the lesion but did not see anything. A scar remains in the area that previously had the lesion. Third suspected case: a 9 month old female living in Kankingi village; usually left to sit and play on the bare ground (sandy soils), lesion developed on the buttocks about 2 months ago, itching of the affected area reported. No other symptoms such as nausea, diarrhea and abdominal pain reported. The child was put on albendazole on the day of investigations.

Possible cause and risk factors
Based on clinical presentation of the third case and description of the first two cases the probable cause was thought to be a soil helminth. A number of dogs and cats, risk factors for the transmission of parasitic worm infestations mentioned above, were seen around the villages of the suspected cases.
Blood samples were obtained from a random sample of 30 persons from the affected villages including the three suspected cases for a full blood count test. The results showed basophilia in 80% of samples, about 50% samples showed lymphocytosis and less than 10% showed eosinophilia.
Stool samples were obtained from the same 30 persons that provided blood in order to identify and confirm the causative agent. The results did not yield any soil helminthes. Additional 20 fresh stool samples that were taken from residents of Nakivale Camp who reported to the health facility all turned out negative for parasites at the reference microbiology laboratories.
Conclusion
Guinea Worm Disease was ruled out. The causative agent was not identified and no further studies were conducted to establish the risk factors. However, from the description of the signs and laboratory results, the following are still probable: Larva currens – More samples need to be taken from those who will be spotted with the lesions still evident. The parasite load in stronyloidiasis is very low and they are very erratic in shedding larva hence very difficult to get in stool; Loa Loa common in Western Uganda and Congo Border with Bundibugyo – blood needs to be taken and microfilaria looked for inpatients with skin lesions; Cutaneous Larva Mi- grans – need to take stool samples from dogs and cats from Nakivale Refugee Settlement and look for all parasites known in literature. It could be the first documented case in Uganda since epidemiology does not support it’s occurrence.


Comments are closed.