Effect of Seasonal Malaria Chemoprevention on Incidence of Malaria Among Children Under Five Years in Kotido and Moroto Districts, Uganda, 2021: Time Series Analysis
Authors: Andrew Kwiringira1,2*, Benon Kwesiga1,2, Richard Migisha1,2, Lilian Bulage1,2, Daniel Kadobera1,2, Damian Rutaazana3, Julius Ssempiira3, and Alex R. Ario1,2, Institutional affiliations: 1Uganda Public Health Fellowship Program, Kampala, Uganda 2Uganda National Institute of Public Health, Kampala, Uganda 3National Malaria Control Division, Ministry of Health, Kampala, Uganda *Correspondence: Email: akwiringira@musph.ac.ug,Tel: +256-775-997-741
Abstract
Background: Seasonal malaria chemoprevention (SMC) refers to monthly administration of full treatment courses of antimalarial medicine to children <5 years during high malaria transmission season. SMC has demonstrated effectiveness in Sahel and sub-Sahel countries in Africa but had never been implemented in Uganda until April 2021, when Uganda began SMC in Kotido and Moroto Districts. We assessed the effect of SMC on malaria incidence among children <5 years of age in Kotido and Moroto Districts.
Methods: We conducted an interrupted time-series analysis using monthly national health data from the Uganda Ministry of Health District Health Information System-2.
We extracted monthly data of outpatient (uncomplicated) malaria among children <5 years, 52 months before SMC (Jan 2017-Apr 2021), and 8 months during SMC implementation (May-Dec 2021). We computed monthly incidence per 1,000 children <5 years. We checked for seasonality, and stationarity in the data. We evaluated the incidence of uncomplicated malaria among children <5 years before and during SMC implementation.
Results: In Kotido District, malaria incidence was 693/1,000 during SMC implementation period, compared to an expected 1,216/1,000 if SMC had not been implemented. The mean monthly malaria incidence was 87/1,000, compared to an expected mean of 152/1,000 if SMC had not been implemented. This represents a statistically significant mean monthly change of -65.4 [-104.6, -26.2] malaria cases/1,000 during SMC implementation.
In Moroto District, malaria incidence was 713/1,000 during SMC implementation period, compared to an expected 905/1,000 if SMC had not been implemented. The mean monthly malaria incidence was 89/1,000, compared to an expected 113/1,000 if SMC had not been deployed. This represents a statistically significant mean monthly change of -24.0 [-41.1, -6.8] malaria cases/1,000 during SMC implementation.
Conclusion: Implementation of SMC substantially reduced incidence of uncomplicated malaria among children <5 years in Moroto and Kotido Districts. The government should consider scaling up SMC in other districts with high malaria transmission.
Introduction
Malaria is the leading cause of death and illness in Uganda and accounts for close to 30% of all inpatient deaths among children under five years of age (1). Inte rventions to reduce the transmission and burden of malaria have intensified over the past 10 years with increasing coverage of malaria control interventions such as long-lasting insecticidal nets (LLINs), indoor residual spraying (IRS), and treatment of malaria cases with artemisinin-based combination therapy (ACTs). However, malaria prevalence in some areas, such as the Karamoja region, remains well above the Uganda Malaria Reduction strategic plan (UMRSP) target of 7% (2). To reduce the burden of malaria in children <5 years, Malaria Consortium supported Ministry of Health to roll out Seasonal Malaria Chemoprevention (SMC) in Kotido and Moroto Districts in April 2021.
Seasonal Malaria Chemoprevention is defined as the intermittent administration of full treatment courses of an antimalarial medicine during the malaria season. The World Health Organization (WHO) recommends administering four monthly courses of two antimalarial drugs to children aged between 3-59 months: sulfadoxine-pyrimethamine (SP) and amodiaquine (AQ) (3). Each monthly SMC course involves one dose of SP and three daily doses of AQ, with SP and the first dose of AQ given under the supervision of the community distributor, and the remaining two doses of AQ given by the caregiver over the following two days.
Malaria data is collected from paper registers sourced from outpatient departments (OPD), inpatient units, laboratories, pharmacies, and village health teams. Collected data are aggregated at health facilities and submitted, as paper reports, to the district level where information is entered into the web-based District Health Information Software version 2 (DHIS2) (4).
In 2018, SMC was implemented in 12 countries of the Sahel and demonstrated effectiveness in this region (5). Evidence that shows that SMC is a promising intervention largely comes from randomized control trials and modelling studies(6, 7), but evidence from routine implementation is limited. This study evaluated the effect of SMC on incidence of uncomplicated malaria among children <5years, when SMC is delivered through routine programmes by community health workers in Kotido and Moroto districts, Uganda.
Methods
Implementation of seasonal malaria chemoprevention in Uganda
Malaria Consortium, in partnership with the National Malaria Control and Elimination programme implemented the SMC in Uganda. District led planning meetings were held before implementation and the meetings involved enumeration of households and the number of children under five years. Training of Village health teams (VHTs) and their supervisors were held a few days prior to the start of SMC implementation — so that knowledge is retained — and three levels of supervision took place; at the district, parish, and village level. After the training, VHTs administered monthly therapeutic courses of antimalarial drugs sulfadoxine-pyrimethamine and amodiaquine (SP+AQ) to about 65,000 children in Moroto and Kotido districts in the Karamoja region. Village health teams are volunteers, but they received special duty allowanceper diem for every day they worked during the campaign. Children who were sick during the time of implementation of SMC were advised to seek clinical care from existing healthcare facilities within their catchment area and records were captured in the health management information system. Whereas SMC is implemented in the Sahel region and western Africa under a 4-month cycle (5), in Karamoja it was implemented under a 5-month cycle—in one rainy season from May to October 2021, when the region records the highest malaria cases (8). Seasonal Malaria Chemoprevention was also implemented during the COVID-19 pandemic in Uganda.
Data source
We obtained monthly data of outpatient (uncomplicated) malaria among children <5 years from the Uganda Ministry of Health District Health Information System 2 (DHIS2), 52 months before SMC (January 2017-March 2021), and 8 months during SMC implementation
(April-December 2021). The DHIS-2 is an open-source platform where each licensed health facility reports monthly data on priority indicators. The platform allows for aggregation of these facility-level data across different administrative levels of the health system, i.e., from sub-location through national level. It does not cover care received in unlicensed facilities or in private pharmacies. We used district-level data because aggregated data smooths out random variations in health service use that occur at health facility-level.
Statistical analysis
We employed an interrupted time series analysis (ITSA) model to compare trends in incidence of uncomplicated malaria among children < 5 years before and during SMC implementation. We computed monthly incidence per 1,000 children <5 years.
Interrupted Time Series Analysis and other time series models assume that preintervention trends, seasonal variations, and levels would remain unchanged in the post-intervention period under a non-intervention counterfactual state(9). The estimated intervention impact is the difference between the forecasted counterfactual-state and observed data during the post-period. The validity of these approaches depends on accounting for any competing processes that could affect these pre-intervention trends and levels – concomitant policies, changes in data recording/measurement, or population composition – thereby biasing the post-intervention counterfactual trend estimates.
We assume that there were no other competing events (structural breaks) other than SMC implementation, that could drive the results. We checked this assumption using Supremum Wald tests for unknown structural breaks, and Wald tests for known structural breaks in the data.
We first conducted descriptive analyses; assessed distributions and outliers of the outcome; decomposed the data to check for seasonality, trends, and random noise; and checked for autocorrelation and partial autocorrelation. We then conducted unit root tests to estimate the number of lags required to make the data stationary.
The ITSA model was specified as follows(10):
𝑌𝑡 = 𝛽0 + 𝛽1𝑡 + 𝛽2D𝑡 + 𝛽3[t-T1] D𝑡 + 𝜀𝑡
where 𝑌𝑡 represents the outcome. TI represents the interruption (SMC implementation) time. Dt is a dummy variable where 1 represents the post-intervention period. t is time from the start of the series. Note that under this formulation [t−TI] will be zero for the pre-intervention period, and 1, 2, …., n for the post-intervention in equal time intervals. The error term, 𝜀𝑡, uses Newey-West standard errors to account for serial 𝜀𝑡 correlation(11)
The interpretation of the estimates is as follows:
𝛽0 is the intercept
𝛽1 is the pre-intervention trajectory
𝛽2 is the immediate intervention effect
𝛽3 is the effect of the intervention over time i.e., the difference in the pre-shock and post-shock trajectories
The number of lags in this formulation is calculated for using the following formula (12):
m=0.75T1/3
We compared the forecasts against the actual observed values in the dataset.
Ethical approval and consent of participants
We obtained permission from the Ministry of Health (MOH) to conduct this evaluation. The Office of Science, U.S. Centers for Disease Control and Prevention, determined that the primary intent of this evaluation was public health practice. The study was conducted by using open access aggregate data in Uganda Ministry of Health DHIS2 and therefore consent to participate in this study is not applicable.
Results
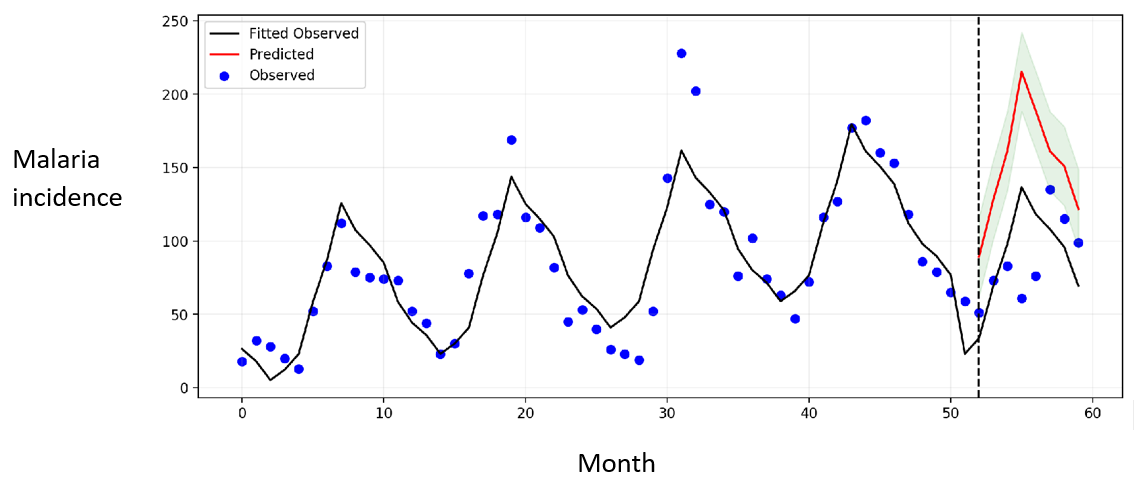
Effect of seasonal malaria chemo-prevention on malaria incidence among children under five years, Kotido District
In Kotido District, malaria incidence was 693 per 1,000 population of children under 5 years during SMC implementation period, compare to an expected 1,216 per 1,000 population if SMC had not been implemented. The mean monthly malaria incidence was 87 per 1,000 population compared to an expected mean of 152 per 1,000 population if SMC had not been implemented (Figure 1). This represents a statistically significant mean monthly change of -65.4 [-104.6, -26.2] malaria cases per 1,000 population during SMC implementation.
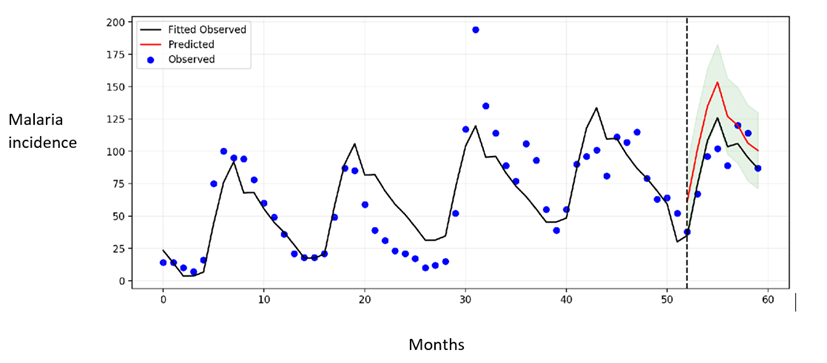
Effect of seasonal malaria chemoprevention on malaria incidence among children under five years, Moroto District
In Moroto District, incidence of uncomplicated malaria was 713 per 1,000 population of children <5 years during SMC implementation period, compared to an expected 905 per 1,000 if SMC had not been implemented. The mean monthly malaria incidence was 89/1,000, compared to an expected 113 per 1,000 if SMC had not been deployed (Figure 2). This represents a statistically significant mean monthly change of -24.0 [-41.1, -6.8] malaria cases per 1,000 during SMC implementation.
Discussion
In our evaluation of effect of SMC on incidence of uncomplicated malaria in Moroto and Kotido districts in Uganda, we found that SMC implementation substantially reduced incidence of uncomplicated malaria among children <5 years in both districts. Our findings are consistent with results from Mali and Burkina Faso where SMC was delivered by community health teams like the case of Uganda (13, 14).
Although SMC reduced malaria incidence by 43% and 21% in Kotido and Moroto district respectively. This is lower than what was observed when SMC was delivered by a similar approach using community health workers; in Burkina Faso, SMC reduced malaria incidence by 69% (14). The observed difference may be partly since SMC was implemented during COVID-19 pandemic in Uganda. A report of lessons learnt from supporting SMC during COVID-19 showed that support supervision was minimised and was less physical (15). More so, there are reports of disruptions of other routine malaria interventions like supply of long-lasting insecticide treated nets (LLINs) at health facilities that could have negatively impacted malaria control (16).
The reduction in malaria incidence in Moroto District was half the reduction observed in Kotido District following SMC implementation. Since SMC was implemented at the same time (during high transmission season) and given that the two neighbouring districts have similar local epidemiological conditions (8), possible explanation for the observed lower reduction in malaria incidence in Moroto may be internal factors like political will. Indeed, lack of political will has been shown to be an obstacle to implementation of public health programs (17). We did not explore reasons for the observed difference in malaria incidence reduction in the two districts following SMC implementation.
This study has limitations. First, DHIS2 data are often incomplete and subject to recording error. Second, aggregated data can mask significant data quality variations in policy impact. These results should not be extrapolated beyond the analysis timeframe as it is unclear if the effects will persist, dissipate, or evolve with time. Future studies can also assess differences in outcomes between facilities known to have higher quality data and compare the results against national aggregate
Conclusion
Implementation of SMC substantially reduced incidence of uncomplicated malaria among children <5 years in Moroto and Kotido district. The government should consider scaling up SMC in other districts with high malaria transmission.
Acknowledgments
We acknowledge Malaria consortium and NMCD for implementing SMC, and Uganda Ministry of Health for the giving us permission to access the data. The authors are grateful to the districts and VHTs that participated in implementation of SMC and for the technical and administrative support provided by the Uganda Public Health Fellowship Program, National Institute of Public Health, and the US Centers for Disease Control and Prevention.
References
- Ministry of Health. Uganda Malaria Reduction Strategic Plan (UMRSP) 2014-2020. Ministry of Health; 2020.
- Nambuusi BB, Ssempiira J, Makumbi FE, Kasasa S, Vounatsou P. Associations and contribution of childhood diseases to fever risk among children less than five years in Uganda. Journal of Global Health Reports. 2020;4:e2020052.
- World Health Organization. Policy recommendation: seasonal malaria chemoprevention (SMC) for plasmodium falciparum malaria control in highly seasonal transmission areas of the Sahel sub-region in Africa. World Health Organisation; 2012.
- Kiberu VM, Matovu JK, Makumbi F, Kyozira C, Mukooyo E, Wanyenze RK. Strengthening district-based health reporting through the district health management information software system: the Ugandan experience. BMC medical informatics and decision making. 2014;14(1):1-9.
- Baba E, Hamade P, Kivumbi H, Marasciulo M, Maxwell K, Moroso D, et al. Effectiveness of seasonal malaria chemoprevention at scale in west and central Africa: an observational study. The Lancet. 2020;396(10265):1829-40.
- Griffin JT, Bhatt S, Sinka ME, Gething PW, Lynch M, Patouillard E, et al. Potential for reduction of burden and local elimination of malaria by reducing Plasmodium falciparum malaria transmission: a mathematical modelling study. The Lancet Infectious Diseases. 2016;16(4):465-72.
- Noor AM, Kibuchi E, Mitto B, Coulibaly D, Doumbo OK, Snow RW. Sub-national targeting of seasonal malaria chemoprevention in the Sahelian countries of the Nouakchott Initiative. Plos one. 2015;10(8):e0136919.
- Kigozi SP, Kigozi RN, Sebuguzi CM, Cano J, Rutazaana D, Opigo J, et al. Spatial-temporal patterns of malaria incidence in Uganda using HMIS data from 2015 to 2019. BMC public health. 2020;20(1):1-14.
- Linden A. Conducting interrupted time-series analysis for single-and multiple-group comparisons. The Stata Journal. 2015;15(2):480-500.
- Huitema BE, McKean JW. Identifying autocorrelation generated by various error processes in interrupted time-series regression designs: A comparison of AR1 and portmanteau tests. Educational and psychological measurement. 2007;67(3):447-59.
- Linden A. Persistent threats to validity in single-group interrupted time series analysis with a cross over design. Journal of evaluation in clinical practice. 2017;23(2):419-25.
- Stock JH, Watson M. Forecasting in dynamic factor models subject to structural instability. The Methodology and Practice of Econometrics A Festschrift in Honour of David F Hendry. 2009;173:205.
- Diawara F, Steinhardt LC, Mahamar A, Traore T, Kone DT, Diawara H, et al. Measuring the impact of seasonal malaria chemoprevention as part of routine malaria control in Kita, Mali. Malaria journal. 2017;16(1):1-12.
- Kirakoya-Samadoulougou F, De Brouwere V, Fokam AF, Ouédraogo M, Yé Y. Assessing the effect of seasonal malaria chemoprevention on malaria burden among children under 5 years in Burkina Faso. Malaria Journal. 2022;21(1):143.
- MC. Implementing seasonal malaria chemoprevention during pandemic. Malaria consortium; 2021.
- IGC. The COVID-19 impact on Ugandan supply chains 2020.
- Zalmanovitch Y, Cohen N. The pursuit of political will: politicians’ motivation and health promotion. The International Journal of Health Planning and Management. 2015;30(1):31-44.

