The first ever reported anthrax outbreak in Bududa District, Eastern Uganda, February – May 2022
Authors: Zainah Kabami1*, Brenda Simbwa1, Brian Agaba1, Helen Nelly Naiga1, Saudah Namubiru Kizito1, Robert Zavuga1, Joshua Kayiwa2, Lilian Bulage1, Fred Monje3 Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda, National Public Health Emergency Operations Centre, Kampala, Uganda, 3Department of Animal Health, Ministry of Agriculture, Animal Industry and Fisheries, Entebbe, Uganda. *Correspondence: Tel: +256758630580, Email: zkabami@musph.ac.ug, zkabami@uniph.go.ug
Summary
Background: In Uganda, anthrax is one of the highest-ranking priority zoonotic diseases, based on a systematic assessment of epidemic potential and socioeconomic impact. Since 2018, anthrax outbreaks have been reported in new districts in Eastern Uganda and for the first time ever, human anthrax was confirmed in Bududa District on May 20, 2022 by the Uganda Virus Research Institute. We investigated to determine the outbreak scope, identify risk factors, and inform control and prevention measures.
Methods: We defined suspected cutaneous anthrax as onset of eschars/skin vesicles; suspected gastrointestinal anthrax was onset of abdominal pain and ≥1 of: diarrhea, vomiting, lymphadenopathy, pharyngitis, or oropharyngeal lesions among Bududa residents in January-May 2022; confirmed anthrax was PCR-positivity for Bacillus anthracis from a swab from skin lesions or blood. We identified cases through active community search and medical records review at health facilities serving the affected villages. We conducted a retrospective cohort study among all household members in affected villages to identify risk factors.
Results: Among 216 study participants, we identified 21 case-patients (15 suspected, 6 confirmed) and 1 death (Case Fatality Rate: 5%) with onsets ranging February-May 2022. Sixteen (76%) were male; mean age was 29 years (range: 5-72). Twelve (57%) had cutaneous anthrax, four (19%) had gastrointestinal anthrax, and five (24%) had both. Bunatsami sub-county was the most affected (Attack Rate: 6/1,000). Cooking (aRR: 122.5, 95% CI: 34.3-439) and eating meat from an animal that died suddenly (aRR: 84, 95% CI: 18-388) increased risk of anthrax.
Conclusion: This outbreak was characterized by both cutaneous and gastrointestinal forms and was associated with cooking and eating meat from cattle that died suddenly. The spread to new regions underscores a need for widespread risk communication about anthrax, and consideration of broad vaccination of animals in this region.
Introduction
Anthrax is a zoonotic disease caused by a gram-positive, endospore-forming bacterium named Bacillus anthracis and is transmitted to humans through contact with or handling infected animals or their products [1]. In humans, it manifests itself in four forms; cutaneous, gastrointestinal, inhalational, and injection anthrax depending on the route of exposure. The cutaneous form affects the skin, the gastrointestinal form affects the digestive system, the inhalational form affects the lungs, and the injection form affects the skin or other body parts [2]. The cutaneous form, with an average incubation period of up to 7 days, accounts for 95% of anthrax cases reported globally and mostly occurs in Africa [2, 3].
Worldwide, approximately 20,000-100,000 cases of human anthrax are reported annually [4] and while the global burden in animals is poorly documented, it has been estimated that a total of 1 billion livestock live in high-risk areas [5]. In Uganda and the neighboring East African countries, anthrax is recognized as one of the highest-ranking priority zoonotic diseases, based on a systematic assessment of socioeconomic impact, epidemic potential, and severity of disease [6-10]. Despite this, sporadic outbreaks continue to occur and are generally poorly documented leading to underestimation of the actual morbidity and mortality of the disease [11].
The first documented occurrence of anthrax in Uganda is at least 1918 [12]. According to the outbreak inventory housed at the National Public Health Emergency Operations Center (NPHEOC), a total of 13 outbreaks were reported in humans and 16 in animals between 2013 and 2022 (Figure 1). In 2018, anthrax appeared for the first time in Eastern Uganda, particularly Kween District [13], and since then, there have been recurrent outbreaks reported in that region. Worse still, there is no policy in place regarding routine vaccination against anthrax in animals, meaning costs of vaccination are privately met [11].
On May 16, 2022, the District Health Officer (DHO) of Bududa District informed the Uganda Ministry of Health (MoH) of cows that died suddenly and suspected cases of human anthrax in neighboring villages. Samples were collected and shipped to the Uganda Virus Research Institute (UVRI), which confirmed the outbreak on May 20, 2022. Bududa District had previously never reported anthrax but is adjacent to districts in Eastern Uganda which have been reporting outbreaks since 2018. We investigated to determine the scope and magnitude of the outbreak in humans and to identify exposures leading to infection in humans.
Methods
Outbreak area
Bududa District is located in Eastern Uganda on the slopes of Mt. Elgon, approximately 257 kilometres from the capital city, Kampala. The district is bordered by the republic of Kenya in the east; the district of Sironko in the north; Mbale in the west; Kween in the northeast and Manafwa in the south. It has an estimated population of 210,173 with an annual growth rate of 4.5% [14]. The district is agriculture-based where the majority of the farmers area small holders who grow both perennial and annual crops [15].
Case definitions and case finding
We defined a suspected cutaneous anthrax case as onset of skin lesions (papule, vesicle or eschar) in a person residing in Bududa District from January – May 2022. A suspected gastrointestinal anthrax case was onset of abdominal pain and at least one of the following: diarrhea, vomiting, lymphadenopathy, pharyngitis, and oropharyngeal lesions in a person residing in Bududa District from January – May 2022. A confirmed human anthrax case was defined as a suspected case that is laboratory-confirmed by isolation of Bacillus anthracis from an affected tissue or site; or any other laboratory evidence of Bacillus anthracis infection based on at least two supportive laboratory tests.
We defined a suspected animal anthrax case as sudden death of an animal in Bududa district from January – May 2022. A probable animal anthrax case was defined as a suspected case with unclotted blood emerging from body orifices in Bududa district from January – May 2022. A confirmed animal anthrax case was defined as demonstration of gram-positive rod-shaped Bacillus anthracis from blood or tissue.
We reviewed medical records at two health facilities serving the affected villages: Bunamono Heathcentre III and Namaitsu Heathcentre II in order to identify human cases. Additionally, with the help of Bududa District Health Officials, District Veterinary Officers, and village health teams (community health workers), we conducted active community search in the villages to identify human and animal cases. We modified the Uganda Ministry of Health human anthrax case investigation form [16] to include relevant demographic characteristics and exposures, and accommodate our case definition. Following this, we generated a line list of case-patients.
Descriptive epidemiology
We described case-patients by person, place, time, and clinical characteristics. Using population data obtained from the Uganda Bureau of Statistics (UBOS) and community health workersof the affected villages, we computed attack rates by sex, village, and sub county. We used QGIS version 3.2.2 to draw maps to present the distribution of cases by place.
Hypothesis generation
We interviewed all 21 case-patients and asked about various exposures to animals from January to May 2022 in Bududa District. These included eating meat from an animal that died suddenly, cooking it and participation in butchering (touched meat/body fluids, carried sick/dead animal, removed animal organs, touched skin/hides, slaughtered animal, had wound, found dead animal remains in garden and did soil related work)
Retrospective cohort study
We conducted a retrospective cohort study in villages located in the more affected sub- county, Bunatsami, where 90% of the cases occurred. We chose to do a cohort study because the affected villages had small populations and all households were easily accessible. We used a structured questionnaire to gather data on demographic characteristics and potential exposures (touching meat/body fluids, carrying sick animal, removing animal organs, touching skin/hides, slaughtering, skinning, presence of a wound at time of contact, doing soil related work, cooking meat from a sick animal and, eating meat). We collected data using KoboToolbox, an open source electronic platform [17]. For respondents below 7 years, we spoke to the parent on their behalf. To measure the associations between exposure variables and illness status, we estimated risk ratios (RR) and their 95% confidence intervals. We conducted additional common reference group analysis for the factors that were statistically significant.
Environmental assessment
We observed the affected areas for any factors that could be associated with introduction of anthrax in the area and its further transmission.
Laboratory investigations
We collected 30 human samples, four animal samples, and two soil samples for laboratory analysis by the Uganda Virus Research Institute and the National Animal Disease Diagnostics and Epidemiology Centre (NADDEC), respectively.
Ethical considerations
This investigation was in response to a public health emergency and was, therefore, determined to be non-research. The MoH through the office of the Director General of Health Services gave the directive and approval to investigate this outbreak.
Additionally, the US Centers for Disease Control and Prevention (CDC) determined that this activity was not human subjects’ research, and its primary intent was public health practice or a disease control activity. We obtained informed consent and assent from respondents accordingly. They were informed that their participation was voluntary and refusal to participate would not result in any negative consequences. Unique identifiers were used to ensure confidentiality.
Results
Descriptive epidemiology
We identified a total of 21 case- patients, 15 (71%) of whom were suspected and six (29%) confirmed (Overall AR:10/100,000) including one death in a 55year-old-male (CFR: 5%). The case-patients presented with signs and symptoms suggestive of either cutaneous only (12, 57%), GIT only (4, 19%), and a combination of both forms of anthrax infection (5, 24%). Fourteen (67%) case-patients’ occupation was related to livestock.
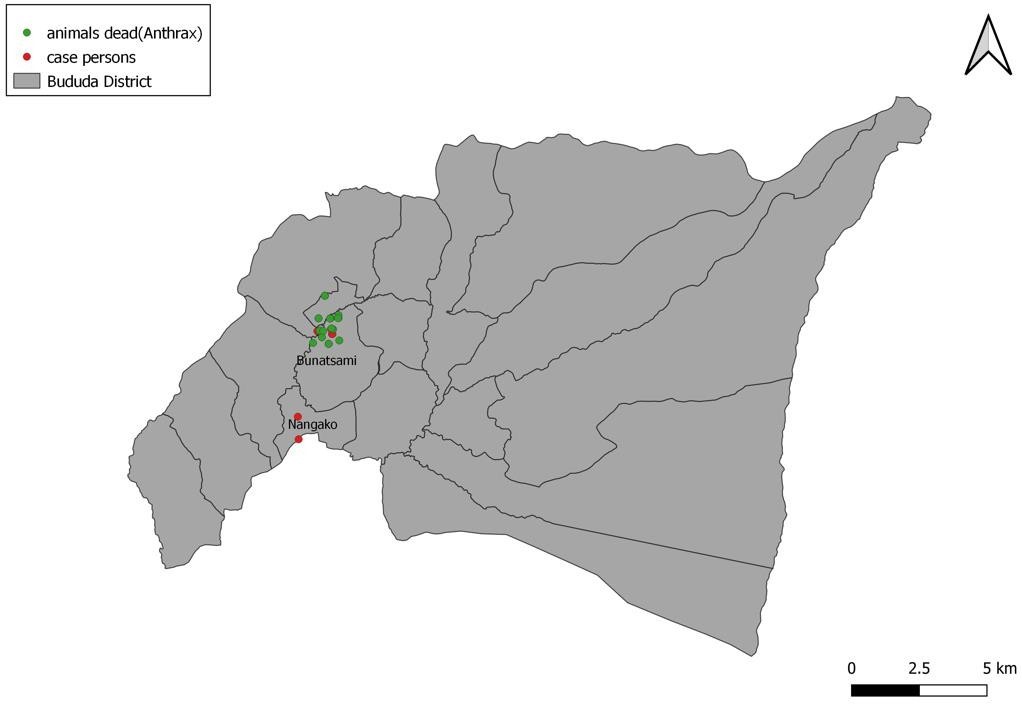
The median age was 26 years (range: 5-72), 16 (76%) were male and were more affected (3 per 1,000) than females. Bunatsami sub county was more affected (6 per 1,000) than Nangako town council (0.3 per 1,000) (Table 1). All case-patients had history of either contact or eating meat from an animal that died suddenly.
Table 1: Attack rates by sex, village, and subcounty during an anthrax outbreak in Bududa District, Uganda, February – May 2022
| Characteristic | Frequency (N=21) | Percentage (%) | Population | Attack Rate/1,000 |
| Sex | ||||
| Male | 16 | 76 | 5,115 | 3 |
| Female | 5 | 24 | 5,102 | 1 |
| Bunatsami subcounty | 19 | 90 | 3,263 | 6 |
| Bumabala lower | 6 | 29 | 77 | 5 |
| Bunalakala | 4 | 19 | 108 | 4 |
| Bumalakala | 4 | 19 | 87 | 3 |
| Bumabala upper | 4 | 19 | 71 | 3 |
| Muririnyi | 1 | 5 | 98 | 1 |
| Nangako Town Council | 2 | 10 | 6,954 | 0.3 |
| Bunamasongo | 1 | 5 | 79 | 1 |
| Bunabunyu | 1 | 5 | 145 | 1 |
Clinical manifestations of human case-patients
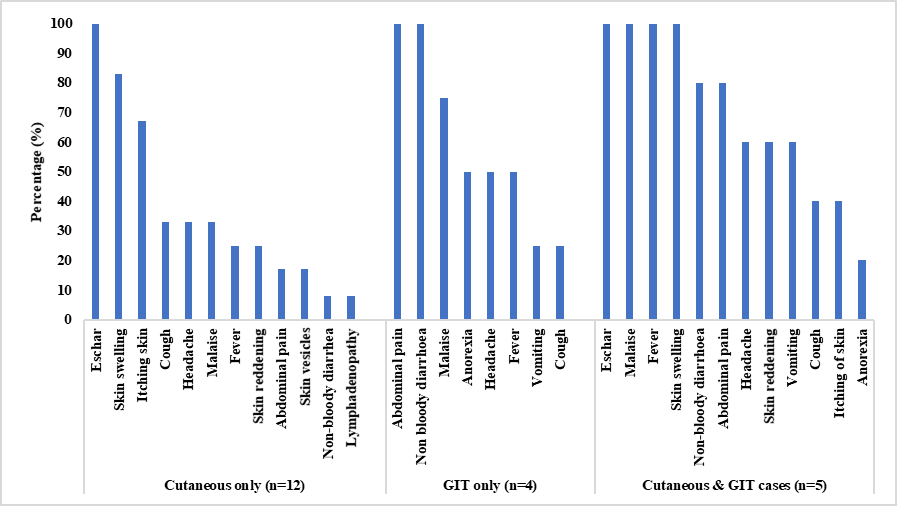
Overall, an eschar (21, 100%), skin swelling (15, 71%), itching of skin, abdominal pain, fever (each at 10, 47%) were the most common symptoms. Upon stratification, an eschar (12, 100%) and skin swelling (10, 83%) were the most common symptom among the 12 cutaneous-only case-patients. All the four GIT-only case-patients presented with abdominal pain and non-bloody diarrhoea (4, 100%), and malaise (3, 75%). All case- patients that had both forms of anthrax presented with fever, malaise, and skin swelling (5, 100%); followed by abdominal pain and non-bloody diarrhoea (each at 4, 80%)
(Figure 3).
Clinical manifestations of animal cases
We identified a total of 17 suspected animal anthrax cases from seven villages in the two sub counties reporting human cases; Bunatsami (16, 94%) and Nangako town council (1, 6%). Two out of the 17 were subsequently confirmed positive by NADDEC; All 17 (100%) animal died within a day of onset of illness while 8 (47%) had blood oozing from orifices; 7 (41%) had difficulty in breathing and rapid bloating.
Deaths among animals occurred from February 14 – May 22, 2022 while onset among case-patients occurred from March 10 – May 27, 2022 (Figure 4). Death among animals precedes onset of disease among humans; all 21 case-patients reported exposure to animals that died suddenly. The first two case-patients with onsets on March 10 and 13 respectively, are a skinner and butcher who both worked at an abattoir in Bushika market and routinely handle meat.

The outbreak in both humans and animals occurred in Bunatsami subcounty and Nangako Town Council (Figure 5).
Hypothesis generation findings
Of the 21 case-patients interviewed, 18 (86%) ate meat from an animal that died suddenly, 12 (57%) had participated in butchering (which included touching meat/body fluids, carrying sick animal, removing animal organs, touching skin/hides, slaughtering, skinning, presence of a wound at time of contact and doing soil related work); 10 (48%) cooked the meat.
Based on the descriptive epidemiology and the hypothesis generation interview findings, we hypothesized that handling and eating meat from an animal that died suddenly was associated with an increased risk of anthrax infection (Table 2).
Table 2: Exposures for anthrax, Bududa District, Uganda, February – May 2022
| Exposures | N | % |
| Participation in butchering
Touched meat/body fluids of animal that died suddenly |
12 |
(57) |
| Carried sick animal/one that died suddenly | 6 | (29) |
| Removed animal organs | 6 | (29) |
| Touched skin or hides | 6 | (29) |
| Slaughtered animal that died suddenly | 5 | (24) |
| Skinned animal that died suddenly | 4 | (19) |
| Did you have a wound/ cut at time of contact | 3 | (14) |
| Found dead animal remains in garden | 1 | (5) |
| Did soil related work | 0 | (0) |
| Ate meat from animal that died suddenly | 18 | (86) |
| Cooked meat of animal that died suddenly | 10 | (48) |
Retrospective study findings
The villages where we conducted the cohort study had a total population of 441. However, we reached 216 persons who were present in the area at the time of the outbreak.
Participating in butchering, preparing and eating meat of an animal that died suddenly was associated with an increased risk of developing anthrax infection (Table 3).
Table 3: Risk factors of anthrax, Bududa District, Uganda, February – May 2022
| Exposure | RR | 95% CI |
| Age category
10 – 19 (reference) <10 20 – 30 31 – 40 ≥ 41 |
0.3 1.7 1.6 0.8 |
0.0 – 2.2 0.3 – 8.4 0.4 – 6.4 0.2 – 2.6 |
| Sex (Female) | 0.3 | 0.1 – 0.7 |
| Participation in butchering, preparation/eating meat
Touched meat/body fluids of animal that died suddenly |
15.3 |
7.7 – 30.4 |
| Carried sick animal/one that died suddenly | 9.3 | 4.4 – 19.4 |
| Slaughtered animal that died suddenly | 13.3 | 8.3 – 21.3 |
| Skinned animal that died suddenly | 12.6 | 8.0 – 19.9 |
| Removed animal organs | 14.1 | 8.7 – 23.0 |
| Touched skin or hides | 14.1 | 8.7 – 23.0 |
| Did you have a wound/ cut at time of contact | 13.3 | 8.3 – 21.3 |
| Found dead animal remains in garden | 12.0 | 7.7 – 18.6 |
| Cooked meat of animal that died suddenly | 16.0 | 7.8 – 33.0 |
| Ate meat from animal that died suddenly | 116.1 | 16.1 – 835.8 |
At multivariate level (common group reference analysis), females were less likely to develop anthrax in comparison to men. People that did not cook but ate meat were 84 times more likely to develop anthrax in comparison to those that did not cook or eat; while people that cooked and ate meat were 122 times more likely to develop anthrax than those that did not cook or eat (Table 4).
Table 2: Factors associated with human anthrax outbreak based on common group analysis, Bududa District, Uganda, February – May 2022
| Exposure | RR | 95% CI |
| Age category | ||
| 10 – 19 (ref) | ||
| <10 | 0.3 | 0.0 – 2.3 |
| 20 – 30 | 1.7 | 0.3 – 8.4 |
| 31 – 40 | 1.6 | 0.4 – 6.4 |
| ≥ 41 | 0.8 | 0.2 – 2.6 |
| Sex | ||
| Male (ref) Female | 0.4 | 0.2 – 0.9 |
| Education level | ||
| Primary (ref) | ||
| None | 1.5 | 0.9 – 2.7 |
| ≥ Secondary | 0.5 | 0.1 – 1.7 |
| Cooking/eating meat | ||
| Did not cook or eat (ref) | ||
| Ate but did not cook | 84.4 | 18.4 – 388.0 |
| Cooked and ate | 122.5 | 34.3 – 437.9 |
| Participated in butchering | ||
| Did not butcher (ref) | ||
| Butchered | 1.4 | 0.9 – 2.6 |
Discussion
This outbreak investigation documented the occurrence of cutaneous and gastrointestinal forms among people who either consumed beef or handled the meat ofa cow suspected to have died of anthrax in Bunatsami and Nangako sub-counties. The clinical manifestations including eschar and skin swelling are evidence of the cutaneous form of anthrax while abdominal pain and vomiting are suggestive of the GIT form.
Males were more affected than females. The index case was a skinner and butcher who routinely participates in butchering and skinning of carcasses from several sources.
In Uganda, anthrax has been occurring among animals with occasional leakage to humans. For humans, the major sources of exposure to B. anthracis are direct or indirect contact with infected animals or contaminated animal product [18]. This particular outbreak among humans occurred after reports of sudden animal deaths; subsequent laboratory testing confirmed anthrax among animals. Butchering anthrax- infected animals, combined with limited vaccination enables further environmental contamination with B. anthracis spores and propagation of the outbreak in both animals and humans [18]. Findings from this investigation are consistent with what has been found in other outbreaks [19].
Anthrax is typically associated with four forms of presentations: cutaneous, gastrointestinal, inhalation, and injection. Our findings suggested that the cutaneous form of anthrax was the most common form in this outbreak. This finding is consistent with other studies where anthrax has been reported both locally and within the African region [20].
The major cause of anthrax in humans is direct or indirect exposure to infected animal products, whereas the risk factors of anthrax among the animal population are host susceptibility, droughts followed by heavy rains, and low levels of pastures hence animals graze close to the ground [5]. These factors were present most likely influencing the anthrax outbreak in both animals and humans. Previous investigations of outbreaks in Uganda that have been done recently also found the association of anthrax to handling of meat from animals that died suddenly [20]. All cases reported in this outbreak were known to have had contact with animals or their products before symptom onset. Contact with animals included any form of participation in butchering.
Butchering is a largely male-dominated role which explains why males were usually the most affected sub-population during anthrax outbreaks [21] and why adults were more affected than children.
Study limitations
Surveillance of anthrax in humans and animals is challenging due to a lack of awareness and identification of cases. Some individuals may have experienced mild, non-specific signs and symptoms of anthrax hence they were likely missed during case- finding. This may have contributed to an underestimation of the scope of the outbreak.
Conclusion
This outbreak was characterized by both cutaneous and gastrointestinal forms and was associated with handling and eating meat from cattle that died suddenly. The spread to new regions underscores a need for widespread risk communication about anthrax, and consideration of broad vaccination of animals in this region.
Conflict of interest
The authors declare that they had no conflict of interest.
Author contribution
Zainah Kabami: led the conception, design, analysis, interpretation of the study and wrote the draft bulletin; Zainah Kabami, Brian Agaba, Helen Nelly Naiga, and Robert Zavuga, participated in the investigation and data collection; Brenda Simbwa, Joshua Kayiwa and Sauda Namubiru supported data analysis; Lilian Bulage and Fred Monje reviewed the report and bulletin.
Acknowledgements
The authors thank the staff of the Uganda Public Health Fellowship Program for the technical support and guidance offered during this study. The authors also extend their appreciation to the National Public Health Emergency Operations Centre (NPHEOC) and the Bududa District Health Office for their contribution during the investigation and response to the outbreak.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as preprint, it should be referenced in the original form.
References
- Anthrax. 2023 [cited 2023 February 20, 2023].
- Types of Anthrax. 2020 [cited 2023 February 20].
- Hicks, C.W., et al., An overview of anthrax infection including the recently identified form of disease in injection drug users. Intensive care medicine, 2012. 38: 1092-1104.
- WHO-EMRO. Anthrax. 2023 [cited 2023 February 20, 2023].
- Carlson, C.J., et al., The global distribution of Bacillus anthracis and associated anthrax risk to humans, livestock and wildlife. Nature microbiology, 2019. 4(8): p. 1337-1343.
- Munyua, P., et al., Prioritization of zoonotic diseases in Kenya, 2015. PloS one, 11(8): p. e0161576.
- Pieracci, E.G., et al., Prioritizing zoonotic diseases in Ethiopia using a one health One Health, 2016. 2: p. 131-135.
- Rist, C.L., C.S. Arriola, and C. Rubin, Prioritizing zoonoses: a proposed one health tool for collaborative decision-making. PloS one, 9(10): p. e109986.
- Salyer, S.J., et al., Prioritizing zoonoses for global health capacity building— themes from One Health zoonotic disease workshops in 7 countries, 2014–2016. Emerging infectious diseases, 23(Suppl 1): p. S55.
- Sekamatte, M., et al., Multisectoral prioritization of zoonotic diseases in Uganda, 2017: A One Health PloS one, 2018. 13(5): p. e0196799.
- Monje, , et al., Anthrax Outbreaks among Domestic Ruminants Associated with Butchering Infected Livestock and Improper Carcass Disposal in Three Districts of Uganda, 2016-2018. 2020.
- Taylor, J., Anthrax in Ankole, Uganda. Transactions of the Royal Society of Tropical Medicine and Hygiene, 1923. 17(1-2): p. 51-54.
- Kisaakye, E., et al., Outbreak of anthrax associated with handling and eating meat from a cow, Uganda, 2018. Emerging Infectious Diseases, 2020. 26(12): p.
- Statistics, B.o. National Population and Housing Census 2014, Area Specific Profiles. 2014 [cited 2023 February 21].
- Statistics, U.B.o. National population and housing census 2014 area specific profiles mubende district. 2017 [cited 2022 November 29 2022].
- Health, o. National Technical Guidelines for Integrated Disease Surveillance and Response, 3rd edition. 2021 [cited 2023 Febraury 21].
- What is Kobotoolbox. 2022 [cited 2023 February 21].
- Rume, F.I., Epidemiology of Anthrax in Domestic Animals of Bangladesh. 2018, University of
- Gombe, , et al., Risk factors for contracting anthrax in Kuwirirana ward, Gokwe North, Zimbabwe. African health sciences, 2010. 10(2): p. 159-164.
- Migisha, , et al., Risk factors for human anthrax outbreak in Kiruhura District, Southwestern Uganda: a population-based case control study. 2021.
- Ntono, V., et al., Cutaneous anthrax outbreak associated with handling dead animals, Rhino Camp sub-county: Arua District, Uganda, January–May 2018. One Health Outlook, 2021. 3(1): 1-7.


Comments are closed.