Yellow Fever Outbreaks in Buliisa, Moyo, and Maracha Districts, Uganda, November 2019-February 2020
Quarterly Epidemiological Bulletin : July to September 2020 Volume 5 Issue 3 Article No. 6 | Authors: 1Peter Muwereza, 1Maureen Nabatanzi, 1Gerald Rukundo, 1Lilian Bulage | Affiliation: 1Uganda Public Health Fellowship Program, Kampala, Uganda
Summary
On 10 December 2019, the Ministry of Health received an alert from the Uganda Virus Research Institute (UVRI) of a PCR confirmed case of Yellow fever from Buliisa District, Mid-Eastern Uganda. During January and February 2020, UVRI confirmed more yellow fever cases in Moyo and Maracha Districts, both located in West Nile. We investigated to determine the scope of the outbreak, identify exposures for transmission, and recommend evidence-based control and prevention measures. We line listed 13 case-patients, 7 confirmed, and 6 probable.
The median age of case-patients was 32 years with a range of 3 to 59 years. Moyo District had the highest attack rate of 5.7(9/158,600), followed by Buliisa, 2(3/149,300), and Maracha, 0.48 (1/208,300). The overall case fatality rate was 54%. Men had the highest attack rate of 3.9/100,000 compared to women 1.2/100,000. Common symptoms reported were fever (100%), headache (77%), unexplained bleeding (54%), and jaundice, vomiting, joint pain, chest pain each at 31%. Majority (92%) lived or worked within 500 metres of a forested area with monkeys and standing water.
All case-patients had not been vaccinated against Yellow Fever. There was very close interaction of humans with sylvatic monkeys in 54% of the case-patients who lived within 10 meters of monkey inhabited forested areas and hunted them for food. These outbreaks were possibly sylvatic, affecting unvaccinated individuals. We recommended mass vaccination campaigns in the affected districts and subsequent inclusion of Yellow Fever Vaccine in Uganda’s routine vaccination schedule. We also recommended controlled interaction of humans with wild animals and their habitats and removal of potential mosquito breeding sites.
Background
Yellow fever is an acute viral hemorrhagic disease caused by the yellow fever virus. The virus is a single-stranded RNA virus that be- longs to the genus Flavivirus, Flaviviridae family. It is transmitted from humans to humans or from animals to humans or humans to animals primarily by the Aedes aegypti, a type of mosquito found throughout the tropics and subtropics. The disease is endemic in tropical areas; in Africa, South America, and Central America. The virus is transmitted when humans go to the jungle (1). Yellow fever virus has three transmission cycles: jungle (sylvatic), inter-mediate (savannah), and urban(2). The incubation period for yellow fever is 3 to 6 days. However, many people do not experience symptoms.
When the symptoms occur, in most cases, they disappear after 3 to 4 days. The clinical disease varies from mild febrile illness to severe disease with jaundice and un-explained bleeding. About 15% of patients get severe disease within 24 hours of recovering from initial symptoms. Several body systems are affected in this phase, usually the liver and the kidneys. Death occurs in 20- 50% of those with severe disease within 7 – 10 days (2,3). Worldwide, the number of yellow fever cases has increased over the past 20 years. This might be attributable to multiple factors, including declining population immunity to infection, increased human activities such as deforestation, urbanization, population movements, low vaccination cover- age, and climate change which increases habitats for mosquitoes(4).
According to the World Health Organization, Uganda is one of the 32 countries in Africa with a high potential for Yellow Fever trans- mission; also located within the Yellow Fever belt. Since the identification of the first outbreak in 1941, several outbreaks have occurred in Uganda, the largest of which affected 181 people and resulted in 45 deaths in northern Uganda in 2010. On 10 December 2019, the Minis- try of Health received an alert from the Uganda Virus Research Institute (UVRI) of a PCR confirmed case of Yellow fever from Buliisa District, Mid-Eastern Uganda.
During January and February 2020, UVRI confirmed more yellow fever cases in Moyo and Maracha Districts, both located in West Nile. We investigated to determine the scope of the outbreak, identify exposures for transmission, and recommend evidence-based control and prevention measures.
Methods
We defined a suspected case as onset of fever (negative for malaria, non-responsive to malaria treatment, and not explained by any other known reasons) in a resident or visitor of Buliisa, Moyo or Mara- cha Districts from 1 October 2019 to March 2020, plus two or more of the following symptoms that are not explained by other causes: abdominal pain, diarrhoea and headache.
A probable case was onset of unexplained fever, plus one or more of the following unexplained symptoms: jaundice, unexplained bleeding, or liver function abnormalities (e.g., elevated levels of transaminases). A confirmed case was a suspected or probable case with positive IgM or PCR tests for yellow fever. We conducted active case-finding to generate a line list at health facilities and in the affected.
We collected and took blood specimens to UVRI for laboratory testing. Three techniques were used to confirm Yellow fever at UVRI; 1) A screening test for IgM antibodies for presumptive diagnosis, 2) Plaque Reduction Neutralization Test (PRNT); employed when IgM is positive, as a confirmatory test; and 3) Polymerase Chain Reaction (PCR), a confirmatory test.
We developed a line-list of case-patients with data on age, sex, residence, exposure information, presenting symptoms, date of onset of symptoms, laboratory tests and results, treatment received, and the disease outcomes. We also conduced environmental assessment to observe for possible exposures to Yellow Fever.
Results
We line listed 13 case-patients, of which seven were confirmed, and six were probable. The mean age of the case-patients was 32 years with a range of 3 to 59 years. Moyo District was the most affected (attack rate [AR=5.7(9/158,600)], followed by Buliisa, [AR=2(3/149,300)], and Maracha [AR=0.48(1/208,300)]. The overall case fatality rate was 54%. Males were more affected (AR=3.9/100,000) compare to females (AR=3/100,000). All case-patients had fever and fatigue.
Other symptoms included; headache (80%), abdominal pain (70%), joint pains (70%), Jaundice (70%), vomiting (60%) vomiting blood (50%), nose bleeding (40%), diarrhea (30%), confusion (20%), Difficulty in Breathing (30%), Cheat pain (20%), convulsions (10%). All case-patients had not been vaccinated against Yellow Fever.
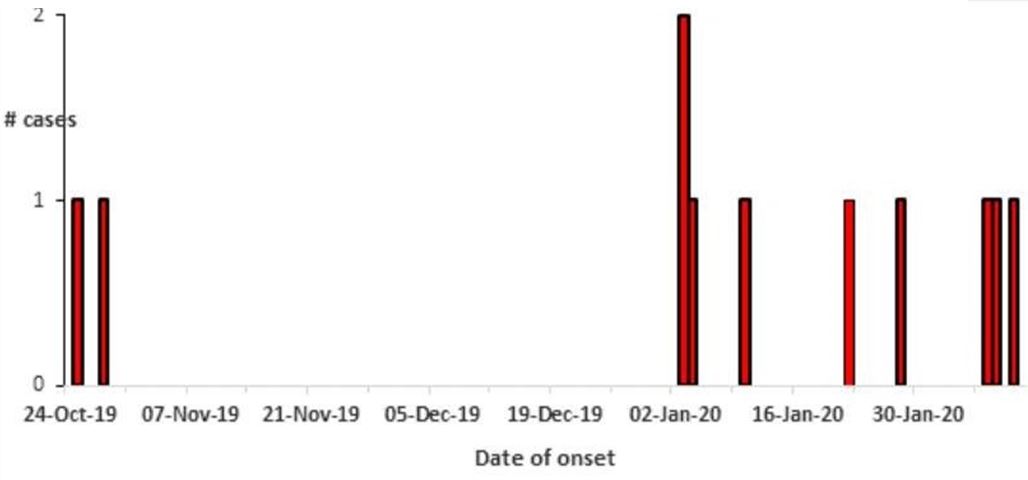
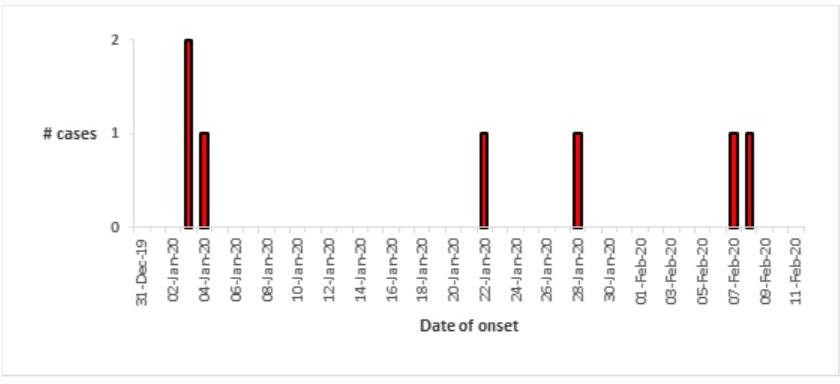
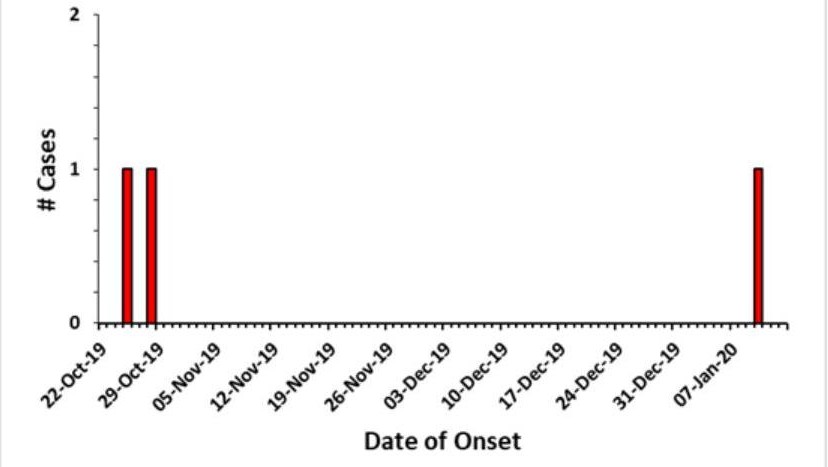
The first case was registered on the 25th of October. More cases were reported thereafter from both Buliisa, Moyo, and Maracha districts until the 11th of February 2020 (Figure 1, 2, and 3).
Majority (92%) of the case-patients lived or worked within 500 metres of a forested area inhabited by monkeys and with standing water. Sylvatic monkeys were frequently seen around the homes and agriculture fields where the case-observed massive deforestation. There was a massive encroachment on the forests where monkeys lived through agricultural activities and deforestation in the affected sub-counties patients lived or worked.
There was a very close interaction of humans with sylvatic monkeys in 54% of the cases who lived within 10 metres of monkeys and hunted them for food. We also observed massive deforestation. There was massive encroachments on the forests where monkeys lived through agricultural activities and deforestation in the affected sub-counties.

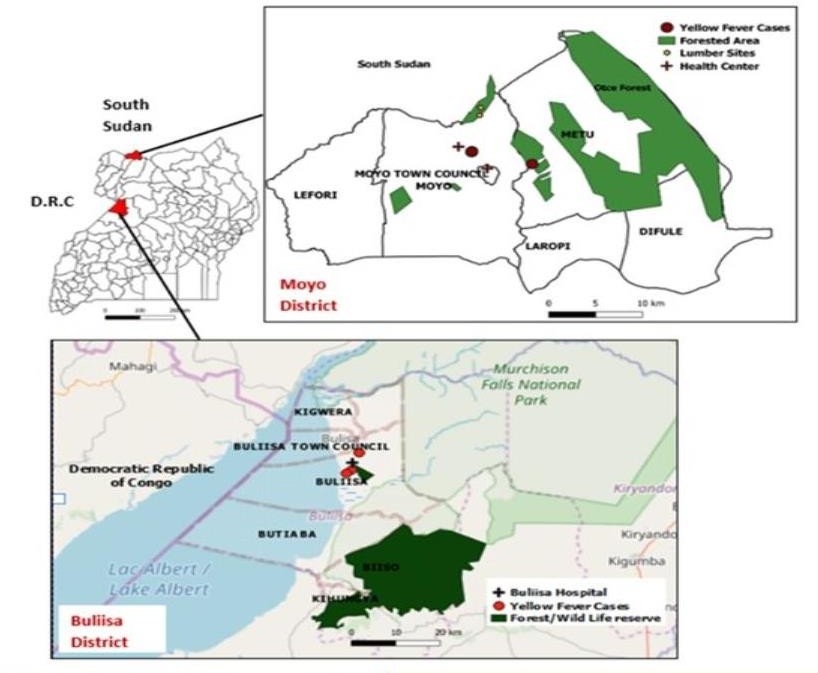
Note! Because of logistical reasons we were unable to get the coordinates for the actual location of the Maracha case.
Discussion
Results from our investigation revealed that these outbreaks were possibly all sylvatic, affecting unvaccinated individuals. Environmental investigation showed presence of sylvatic monkeys, and mosquito breeding sites around farmlands and homesteads of case-patients. Majority of the case-patients lived or worked within 500 metres of a forested area with monkeys and standing water.
There was close interaction of humans with sylvatic monkeys in 54% of the cases who lived within 10 metres of monkey fields and hunted them for food. This transmission form of yellow fever (sylvatic/jungle cycle) has been identified in other yellow fever out- break investigations where transmission involves transmission of the virus between non-human primates and mosquitoes.
Studies have shown that humans working or travelling in the forest are bitten by infected mosquitoes and develop yellow fever(5–7). In this investigation, massive deforestation was observed. Areas experiencing yellow fever outbreaks have been observed to practice deforestation, resulting in increased contact with sylvatic monkeys (8). Monkeys were hunted for food in Buliisa and Moyo Districts.
This practice greatly increased the risk of human exposure to yellow fever due to the close human-monkey interactions (4). These outbreaks occurred in different districts that do not share boarders, they could have occurred spontaneously and independently due to transmission of the virus from sylvatic monkeys to humans via mosquito bites.
However, this could not be ascertained due to logistical limitations to do genetic sequencing of the viruses from different districts. The affected districts experienced rains in the period between October and February in which the outbreaks occurred. This increased breading sites for mosquitoes and facilitated the outbreaks. In this outbreak, all case-patients reported no history of yellow fever vaccination yet vaccination is the single most important measure to contain yellow fever outbreaks (9).
In Uganda, yellow fever vaccination is not part of the routine immunisation schedule. Only those seeking international travel access this vaccine at a cost. This implies the immunity against yellow fever is low and majority of Ugandans are at risk (4). At the end of this outbreak, ministry of health organised a mass vaccination campaign in the affected districts.
Conclusions & Recommendations
We recommended Mass Vaccination in the affected districts and subsequent inclusion of Yellow Fever Vaccine in Uganda’s routine vaccination schedule. We also recommended avoidance of very close interaction of humans with wild animals and their habitats and removal of potential mosquito breeding sites.
References
- Areas with Risk of Yellow Fever Virus Transmission in Africa. 2020.
- Yellow fever Fact sheet N°100. 2013 May.
- Heymann Control of communicable diseases manual. American Public Health Association; 2008.
- Kwagonza L, Masiira B, Kyobe-Bosa H, Kadobera D, Atuheire EB, Lubwama B, et al. Outbreak of yellow fever in central and southwestern Uganda, February–may 2016. BMC Infect 2018;18(1):548.
- Soghaier MA, Hagar A, Abbas MA, Elmangory MM, Eltahir KM, Sall AA. Yellow Fever outbreak in Darfur, Sudan in October 2012; the initial outbreak investigation report. J Infect Public 2013;6(5):370–376.
- Carrington CV, Auguste Evolutionary and ecological factors underlying the tempo and distribution of yellow fever virus activity. Infect Genet Evol. 2013;13:198–210.
- Hamrick PN, Aldighieri S, Machado G, Leonel DG, Vilca LM, Uriona S, et al. Geographic patterns and environmental factors associated with human yellow fever presence in the PLoS Negl Trop Dis. 2017;11(9):e0005897.
Reference this page as below
1Peter Muwereza, 1Maureen Nabatanzi, 1Gerald Rukundo, 1 Lilian Bulage. Yellow Fever Outbreaks in Buliisa, Moyo, and Maracha Districts, Uganda, November 2019-February 2020. Kampala. Uganda National Institute of Public Health. 2020 September 30th. Available from:https://uniph.go.ug/yellow-fever-outbreaks-in-buliisa-moyo-and-maracha-districts-uganda-november-2019-february-2020.


Comments are closed.