Uptake of Human Papilloma Vaccination in Uganda, Barriers and Opportunities: A Policy Brief
Quarterly Epidemiological Bulletin: October– December, 2020 Volume 5 / Issue 4 /Article No. 6 Author: Dr. John Kamulegeya, Uganda Public Health Fellowship Program, Kampala, Uganda
Summary
Human papillomavirus (HPV) infection is the primary cause of cervical cancer. Cervical cancer is the leading cause of cancer deaths among women in Uganda and Sub Saharan Africa. HPV types 16 and 18 are responsible for about 70% of all cervical cancer cases worldwide. Vaccination against these prominent types of human papilloma virus has the potential to drastically reduce HPV-associated diseases, including cervical and other anogenital cancers. HPV vaccine against two sero types, 16 and 18 has been available for routine immunisation since 2014, targeting 10 year old girls using a two- dose schedule with an interval of six months between doses. However, HPV vaccination uptake is low with less than 50% of targeted girls receiving their 2nd follow up dose. A number of individual, community, and health system factors affect HPV vaccination. Multi prong strategies aimed at reaching younger girls, empowering the girl child and their parents /caretakers to demand for HPV vaccination services should be embraced in order to achieve high vaccination uptake in Uganda.
The policy brief is intended to strengthen the guidance for health policy implementation of HPV vaccination in Uganda.
Background
Human papillomavirus (HPV), is a highly prevalent sexually trans-mitted infection. Human papillomavirus is the primary cause of cervical cancer (>99% of cases) (1). Vaccination against prominent types of human papillomavirus (HPV) has the potential to dramatically reduce HPV- associated diseases, including cancer. However vaccine uptake has been variable and suboptimal in most countries, with low levels of both initiation and completion of the HPV doses (2). A woman’s lifetime risk of acquiring HPV infection is greater than 80% and most infections occur within 3–4 years of sexual debut. Among HIV positive women, the prevalence of HPV infections and high grade cervical pre-cancer lesions is several folds higher than in HIV negative women.
Approximately 90% of deaths from cervical cancer occur in low- and middle-income countries. The high mortality rate from cervical cancer globally could be reduced through a comprehensive approach that includes prevention through HPV vaccination, early diagnosis, effective screening and treatment programmes. Women in low- as opposed to those in high-income settings have about a twofold cumulative risk of developing cervical cancer before the age of 65 years. Equally, women in low income settings have a threefold risk of dying from cervical cancer than those in high income settings(3, 4).
In developing countries, primary prevention through Human papilloma vaccination is the most feasible and cost effective method to reduce the morbidity and mortality due to CxCa . With moderate financial support, it is feasible to archive high vaccination rates by using existing education and health infrastructure(5). An optimal coverage (≥70%) of the target population, the lifetime risk of cervical cancer could be reduced by >50%.
Oncogenic HPV types 16 and 18 are responsible for over 70% of cervical cancers, globally. Uganda has one of the highest cervical cancer incidence rates in the world with the age- standardized incidence rate of 47.5 per 100, 000. Cervical cancer(CxCa) is the leading cancer among women in Uganda , contributing up to about 50–60% of all female malignancies(6) .
In Uganda, preventive HPV vaccine that protect against two sero types HPV 16 and 18 has been available for routine immunisation since 2014, using a two-dose schedule with an interval of six months between doses for human papillomavirus(HPV) vaccine.
Ugandan targets to vaccinate all girls aged 10 years. The strategy used is reaching out to pupils in primary four. Vaccination is delivered during every static and outreach immunization sessions but intensified through Integrated Child Health Days during the months of April and October where health workers conduct school-based outreaches.
We explored uptake of HPV vaccination, implementation challenges (cultural barriers, operational and logistical) so to identify and recommend strategic interventions to improve HPV vaccination uptake in Uganda.
Problem Analysis
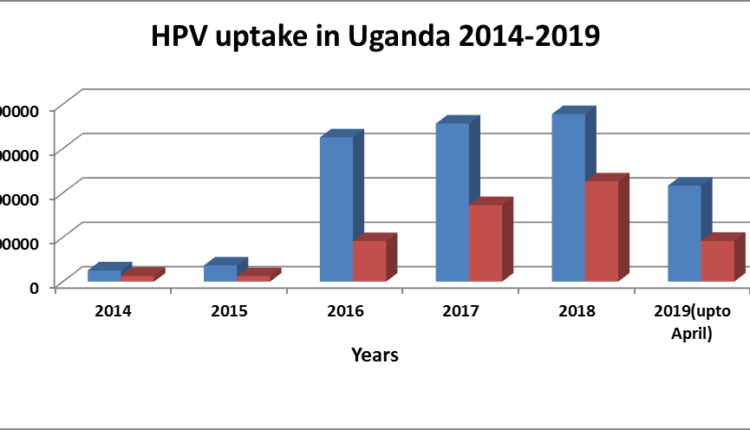
Despite HPV vaccination being free, HPV vaccination uptake is low with less than 50% of targeted girls receiving their 2nd follow up dose. In addition, the routine immunisation program is not reaching out to all targeted girls (Figure 1) (Source- District Health Information System- DHIS 2)
Factors affecting uptake of Human Papilloma Vaccination, Uganda
HPV vaccine uptake (i.e., initiation and completion) among eligible girls is affected by a number of factors. These include, health system factors, individual factors such as HPV awareness and knowledge, beliefs about HPV and the vaccine (e.g., perceived vaccine effectiveness, daughters ‘perceived risk for HPV, perceived severity of HPV infection), general immunization attitudes and demographics of parents. Cultural and religious factors have been shown to affect immunisation uptake
Human papillomavirus (HPV) vaccine uptake in many countries has been sub-optimal. Several individual factors are associated with low vaccination including fears about sexual risk , concerns about vaccine safety, inadequate vaccination recommendations by health care providers (HCPs), and distrust due to the perceived “newness” of HPV vaccines(7).
HPV vaccination presents special challenge for the fact that it targets sexually transmitted disease yet given to adolescent girls who have not yet had sexual intercourse. Secondly, the primary efficacy endpoint was a surrogate for invasive cancer, which takes decades to develop after initial HPV infection. It is because of this that some communities in Uganda claim that the vaccine has a contraceptive component that can cause infertility.
Teachers’ knowledge
Since one of the major delivery strategies is through school outreaches, it critical that teachers to the pupils have adequate knowledge on HPV vaccination and cervical cancer. Studies have found out that knowledge about HPV vaccine among school teachers was low. Empowering teachers to be vaccine champions in their community may be a feasible way of disseminating information about HPV vaccine and cervical cancer. Teachers with little knowledge on HPV vaccine are less likely to accept the vaccine than those who know more(8).
Health system factors
Health service delivery challenges are one of the greatest barriers to HPV vaccination, specifically the lack of capacity to track and distribute reminders to eligible patients, low ability to effectively mobilise communities and commodity logistic challenges. Also variation in health workers’ counseling approaches to emphasize cancer prevention benefits of the vaccine has been noted as barriers to HPV uptake (9, 10). Health care providers do not strongly recommend the vaccine, are not effectively educating their patients about it, are not outlining its vaccination schedule, and are not urging families to start and then complete the vaccination in time.
Community/societal factors
In addition, parental consent for daughters to receive the HPV vaccination is critical for the HPV vaccination programme (11). Engagement of all stakeholders is critical for successful HPV vaccination. Leadership by public health professionals and clinicians and nurses is essential but parents, teachers, schools, legislators, religious and cultural leaders, all need to be involved at both planning and implementation of HPV vaccination in communities (12).
Because of culture, adults feel embarrassed talking about sex with “children,” This is exacerbated by the fact that different cultures have strongly held taboos about children sex education this process. Unlike other vaccine preventable diseases such as polio, measles, pneumonia and meningitis, which most parents have at least heard of and know enough to fear, HPV is a largely unknown entity(13).
Solution Analysis
The success of future human papillomavirus (HPV) vaccination programs will depend on individuals’ willingness to accept vaccination, parents’ willingness to have their preadolescent and early adolescent children vaccinated, and health care providers’ willingness to recommend HPV vaccination(14).
Involvement of Adolescents, Care takers, and Parents
Studies have found that individuals’ knowledge and attitudes toward the vaccine are associated with immunization uptake. Providing substantial information for participants, particularly adolescents who may exercise a significant level of autonomy in decision-making can greatly increase HPV vaccination uptake
Research to understand reasons for low uptake
Since HPV vaccine is administered prior to an adolescent’s sexual debut, this ultimately requires understanding decision-making for a young adolescent to receive a vaccine targeting a sexually transmitted infection (STI). Given the fact that vaccinating pre-adolescents and adolescents is a relatively new phenomenon in many resource-limited settings, formative socio-behavioral research is essential for providing a framework for optimizing vaccine uptake(14). Qualitative research to understand psychosocial barriers to HPV vaccination, including concerns about vaccine safety and efficacy, and its impact on future fertility in order to effectively design programs that would optimize vaccine uptake.
Use of care givers and peer and cultural influencers
In a study in South Africa on uptake of HPV vaccines, caregivers expressed difficulty initiating conversations with their adolescents related to sexual activity or sexual risk-taking, due to lack of information about HPV as well as cultural constrains. Healthcare providers at the adolescent clinic were described as adult proxies who could have conversations with their children about sexual health, in order to ‘‘provide knowledge about sexual issues
Parents value the information and recommendations provided by their children’s health care providers. At the same time, health care providers will need to be prepared to provide patients and parents with information about HPV and HPV immunization and to respond productively to the rare parent who expresses opposition to HPV vaccine(10).
Recommendations
Community Dialogue
Community dialogues have the potential to alleviate some critical concerns that parents may have when vaccinating their children against HPV. The dialogues should emphasize HPV vaccination benefits. Studies that have examined the dyadic process of vaccine decision-making between parents and adolescents have identified benefits that result from the process itself as well as the communications surrounding HPV vaccine. In addition, information given in community dialogues communication about HPV vaccine may improve parents discussions with young adolescents on positive sexual health. Community dialogues will bridge information and communication gap between parents, young adults, adolescents, and health care providers so that higher HPV vaccination rates can be achieved
Community sensitization
Accumulating evidence suggests that many of the social/behavioral concerns associated with HPV vaccine that have sparked resistance among patients and providers (and have been the focus of media reports) have little or no basis in reality (16). Community sensitization using mass media such as radio, TV and social media platforms to correct miss-information may improve uptake of HPV in Uganda.
Involvement of Teachers
Since the greatest target population for HPV vaccination is in primary schools, teachers should be given enough information about HPV vaccination, its importance and safety. In addition, teachers and schools’ administration should be involved in all stages of planning, monitoring and vaccination implementation.
Reminders and Brochures
Electronic alerts prompted telephone reminders for dose completion. These results show that an evidence-based educational brochure and reminder system appeared to improve HPV vaccine uptake and dose completion rates at this private pediatric practice. Electronic alerts prompted telephone reminders for dose completion(15)
Research to identify barriers and opportunities to improve HPV vaccination uptake
Research has shown that the reasons for and expressions of vaccine hesitancy are highly varied and need to be better understood in order to appropriately address emerging concerns. Reasons for suboptimal HPV vaccination coverage will be better understood by carrying out a qualitative and quantitative research in Uganda in order to inform policy.
References
- Munoz Human papillomavirus and cancer: the epidemiological evidence. Journal of clinical virology. 2000;19(1):1-5.
- Gattoc L, Nair N, Ault Human papillomavirus vaccination: current indications and future directions. Obstet Gynecol Clin North Am. 2013;40(2):177-97.
- Shanta V, Krishnamurthi S, Gajalakshmi C, Swaminathan R, Ravichandran Epidemiology of cancer of the cervix: global and national perspective. Journal of the Indian Medical association. 2000;98(2):49.
- Comprehensive cervical cancer control,A guide to essential practice. 2006.
- Goldie SJ, O’Shea M, Campos NG, Diaz M, Sweet S, Kim S-Y. Health and economic outcomes of HPV 16,18 vaccination in 72 GAVI-eligible countries. Vaccine. 2008;26(32):4080-
- Wabinga H, Parkin D, Wabwire-Mangen F, Nambooze Trends in cancer incidence in Kyadondo County, Uganda, 1960-1997. British Journal of Cancer. 2000;82(9):1585-92.
- Zimet GD, Rosberger Z, Fisher WA, Perez S, Stupiansky NW. Beliefs, behaviors and HPV vaccine: Correcting the myths and the Preventive Medicine. 2013;57(5):414-8.
- Mabeya H, Menon S, Weyers S, Naanyu V, Mwaliko E, Kirop E, et Uptake of three doses of HPV vaccine by primary school girls in Eldoret, Kenya; a prospective cohort study in a malaria endemic setting. BMC Cancer. 2018;18(1):557.
- Sussman AL, Helitzer D, Bennett A, Solares A, Lanoue M, Getrich Catching Up With the HPV Vaccine: Challenges and Opportunities in Primary Care. The Annals of Family Medicine. 2015;13(4):354-60.
- Zimet Improving adolescent health: Focus on HPV vaccine acceptance. Journal of Adolescent Health. 2005;37(6, Supplement):S17-S23.
- Buang SN, Ja’afar S, Pathmanathan I, Saint V. Human papillomavirus immunisation of adolescent girls: improving coverage through multisectoral collaboration in Malaysia. BMJ. 2018;363:k4602.
- Yildirim JG, Arabaci Z. Innovations in HPV vaccination and roles of nurses in cervical cancer Asian Pacific journal of cancer prevention : APJCP. 2014;15(23):10053-6.
- Palfrey New initiatives to improve HPV vaccination rates. Human Vaccines & Immunotherapeutics. 2016;12(6):1594-8.
- Katz IT, Nkala B, Dietrich J, Wallace M, Bekker L-G, Pollenz K, et al. A Qualitative Analysis of Factors Influencing HPV Vaccine Uptake in Soweto, South Africa among Adolescents and Their Caregivers. PLoS One. 2013;8(8):e72094.
- Cassidy B, Braxter B, Charron-Prochownik D, Schlenk EA. A Quality Improvement Initiative to Increase HPV Vaccine Rates Using an Educational and Reminder Strategy With Parents of Preteen Girls. Journal of Pediatric Health 2014;28(2):155-64.
- Zimet GD, Rosberger Z, Fisher WA, Perez S, Stupiansky NW. Beliefs, behaviors and HPV vaccine: correcting the myths and the misinformation. Prev Med. 2013;57(5):414-8.
Reference this Article as below
John Kamulegeya, Uptake of Human Papilloma Vaccination in Uganda, Barriers and Opportunities: A Policy Brief. Kampala, Uganda National Institute of Public Health. 2020 December 26th. Available from::https://uniph.go.ug/wp-content/uploads/2021/05/6-LB18Jan2021-John-Kamulegeya_HPV.pdf.


Comments are closed.