Spatial and Temporal Trends of Cervical Cancer, Uganda, 2012-2021: Analysis of Surveillance Data
Authors: Rose Nampeera1*, Miriam Nakanwagi1, Edirisa Juniour Nsubuga1, Benon Kwesiga1, Daniel Kadobera1, Nixon Niyonzima2, Alex Riolexus Ario1; Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda 2Uganda Cancer Institute, Kampala, Uganda; Correspondence*: Email: rnampeera@musph.ac.ug, Tel: +256-704-367-815
Summary Background: Cervical cancer is the commonest cancer and the leading cause of cancer-related deaths among women in Uganda. The Uganda Ministry of Health (MoH) has adopted a number of strategies to address the burden of cervical cancer, including cervical cancer screening in public health facilities, family planning services and human papillomavirus vaccination for girls aged 9-13 years. However, the impact of these interventions on cervical cancer incidence is not documented. We described the spatial and temporal trends of cervical cancer screening and incidence among women attending health facilities in Uganda from 2012 to 2021 to inform programming by relevant institutions. Methods: We extracted surveillance data for screening and incident cervical cancer cases per month during 2012-2021 by district, region and country. We calculated the screening and incidence rate by district, region and country level using the Uganda Bureau of Statistics population projections of total female population aged 15+ as the denominator. We calculated significance of the trends over time using logistic regression. Results: A total of 439,230 women were screened for cervical cancer from 2017 to 2021. The highest screening rate was in 2020 (1,420/100,000) and the lowest was in 2019 (10/100,000). There was a 378% increase in the screening rate over the years. Nationwide, 14,257 newly diagnosed cervical cancer cases were observed from 2012 to 2021.The peak incidence of cervical cancer was 2,020 (20/100,000) in 2016 and the lowest incidence was 1,143 (5/100,000) recorded in 2021. There was a 32% decrease in the incidence of cervical cancer from 12/100,000 in 2012 to 5/100,000 in 2021 (p<0.001). Regionally, there was a significant decrease in the incidence of cervical cancer over the years except in Northern Uganda which had a 2% increase over the years. Central Uganda had the biggest decrease of 8% over the years. Conclusions: Despite the significant increase in cervical cancer screening, fewer cases of cervical cancer were registered in Uganda over the years. Only Northern Uganda had an increase in incidence of cervical cancer over the years. We recommend expansion of screening to cover all eligible female populations and strengthening of strategies to sustain the decline in cervical cancer cases. Further investigations are needed to understand the reasons for the increasing incidence in Northern Uganda.
Background
In 2020, cervical cancer was the fourth commonest cancer worldwide with 604,000 new cases and 342,000 deaths; the Low and Middle Income Countries (LMICs) bearing the brunt at 84% of new cases and 90% of deaths (1) East Africa had the highest age standardized cervical cancer mortality of 30 per 100,000 and second highest incidence rate of 40/100,000 in 2018 (2). In Uganda, cervical cancer was the commonest cancer among women with an age standardized rate (ASR) incidence of 56.2 per 100,000 and cancer related death rate of 41.4 per 100,000 in 2020 (3).
Most of the cervical cancer cases (at least 95%) are due to infection with human papillomaviruses (HPV) that are transmitted through sexual intercourse (4). Majority of sexually active women are infected with HPV in their lifetime but nearly all clear the infection in a year (5). Unfortunately, 12% of acute HPV infections become persistent and may progress to precancerous lesions or invasive cervical cancer over decades (6). This known cause plus the long natural history of HPV infection allows an opportunity for effective interventions to manage cervical cancer (7). Cervical cancer can be prevented by HPV vaccination. Additionally, screening for cervical cancer aids timely intervention to treat precancerous lesions (8).
Papanicolaou (PAP) smear testing has been used as a screening tool for cervical cancer for more than 50 years in Uganda (9). The Uganda Ministry of Health (MoH) recommends screening with Visual Inspection with Acetic acid (VIA) for all women aged 25-49 years. The screening is scheduled every year for HIV positive women and every 3 years for HIV- negative women (9). However, screening uptake has been low due to limited resources or unwillingness to commit financial resources (10). HPV vaccination was scaled up in Uganda in 2015 after 2 successful pilot studies in 2008 and in 2012, and is now part of the national routine immunisation program (11).
Despite these measures, the incidence of cervical cancer is still unacceptably high. There is limited documentation of trends and geographical distribution of cervical cancer in Uganda. We describe the spatial and temporal trends of cervical cancer screening and incidence among women attending health facilities in Uganda, 2012-2021 to inform programming by relevant institutions including MoH.
Methods
Study design, data source, and study population
We analyzed surveillance data on screening and newly diagnosed cervical cancer among women attending health facilities in Uganda, 2012-2021 from the District Health Information System version 2 (DHIS2). DHIS2 is a platform for reporting, analysis, and dissemination of health data reported through the health management information system (12). Cervical cancer screening and diagnosis in Uganda is routinely carried out in family planning clinics in health facilities from Health Centre III (HC III) upwards. However, since 2020, cervical cancer screening is also being carried out in HIV clinics. At the healthy facilities, cervical cancer individual level patient data on screening and diagnosis is recorded in outpatient department registers. The individual level patient data is then summarised in the outpatient department monthly report among other parameters in the report. The reports from HC III facilities are then submitted to the HC IV and then to the district level.
At the district, data for health facility levels III and IV are entered into the DHIS2 by the district biostatistician. Regional and national referral hospitals send data directly to DHIS2. At the MoH headquarters, data from all health facilities are collated and the national performance on each indicator is determined.
The DHIS2 specifically contains data regarding cervical cancer screening, total cases, and newly diagnosed cases. We considered all records of women who tested positive for cervical cancer from 2012–2021 and all women who screened for cervical cancer from 2017–2021 as reflected in the DHIS2. Data for cervical cancer screening was not available before 2017 because it was not being reported at the time.
Study variables, data abstraction, and analysis
We extracted district, regional, and national data from the DHIS2 on: Newly diagnosed cancer of the cervix cases from the HMIS 108-GC01a in the new DHIS2 (2020-2021) and HMIS 108-6 in the old DHIS2 (2012-2019) and cases of cervical cancer screening done from HMIS 105-MC11a in the new DHIS2 (2020-2021) and LMIS in the old DHIS2 (2012-2019). We also abstracted data on outpatient reporting rates from the HMIS 105:01 from the new DHIS2 (2020-2021) and HMIS 105:1 in the old DHIS2 (2012-2019) to show accuracy of the trend. We abstracted data on adult women aged 15+ from the Uganda National Bureau of Standards from 2014–2021. For the years 2013 and 2014, the population was calculated using the national yearly growth rates.
We extracted surveillance data for screening and incident cervical cancer cases per month during 2012-2021 regionally, nationally, and per district. We calculated the screening and incidence rate at the national, regional, and district level. The screening and incidence of cervical cancer was calculated using the population projections of total female population as the denominator for the country, region, or district by the Uganda Bureau of Statistics. We calculated significance of the cervical cancer trends over time using logistic regression in Epi-info version 7. We interpreted the odds ratios as the odds of increase or decrease in the incidence of cervical cancer or cervical cancer screening per 100,000 women per year. Choropleth maps were drawn using QGIS version 3.6.3 to show the regional and district-level distribution of cervical cancer.
Ethics considerations
Our study utilized routinely collected aggregated program surveillance data that did not have any personal identifiers. We obtained permission to use the HMIS data from the Ministry of Health Resource Centre which has the overall mandate to collect and store health related information. Additionally, the U.S. Centers for Disease Control and Prevention (CDC) Center for Global Health determined our study was non-research whose primary intention was to address public health problems. We stored data in password-protected computers and data was not shared with anyone outside the investigation team.
Results
Trends of incidence, screening rate, and outpatient reporting rate of cervical cancer, Uganda, 2012 –2021
Overall, a total of 439,230 women were screened for cervical cancer from 2017 to 2021. The highest screening rate was in 2020 (1,420/100,000) and the lowest was in 2019 (10/100,000). Nationwide, 14,257 newly diagnosed cervical cancer cases were registered from 2012 to 2021. The peak incidence of cervical cancer was 2,020 (20/100,00) in 2016 and the lowest incidence was 1,143 (5/100,000) in 2021. There was a 378% general increase in the screening rate over the years. The outpatient reporting rates increased across the years from 50.3% in 2012 to 99.8% in 2021. There was an overall decrease in incidence of cervical cancer despite the increase in outpatient reporting rates and screening rates (Figure 1 and Table 2).
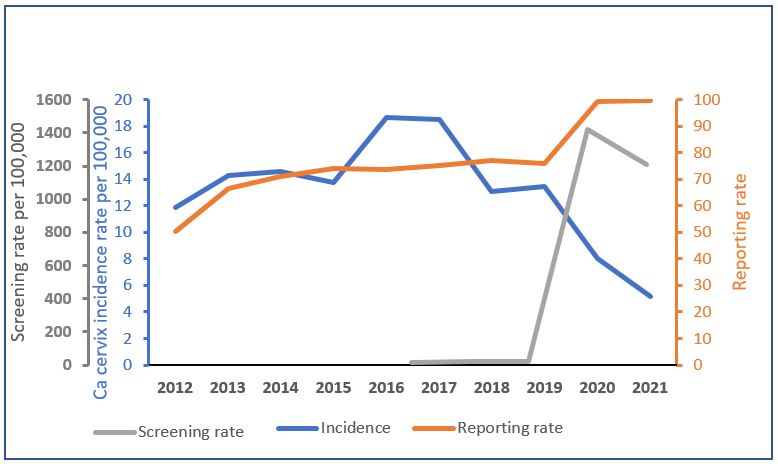
Table 1: Significance of the trends of cervical cancer incidence, Uganda,2012 to 2020
| Year | Incidence | OR | 95% CI | P-Value |
| 2012 | 12 | 1 | ||
| 2013 | 14 | 1.1 | 1.1 – 1.3 | < 0.001 |
| 2014 | 15 | 1.2 | 1.1 – 1.3 | < 0.001 |
| 2015 | 14 | 1.2 | 1.07 – 1.2 | < 0.001 |
| 2016 | 20 | 1.6 | 1.5 – 1.7 | < 0.001 |
| 2017 | 17 | 1.6 | 1.4 – 1.7 | < 0.001 |
| 2018 | 13 | 1.1 | 1.02 – 1.2 | 0.016 |
| 2019 | 13 | 1.1 | 1.05 – 1.2 | < 0.001 |
| 2020 | 8 | 0.7 | 0.62 – 0.74 | < 0.001 |
| 2021 | 5 | 0.4 | 0.4 – 0.5 | < 0.001 |
Trend of incidence, screening for cervical cancer, and inpatient reporting rates by region, Uganda, 2012–2021
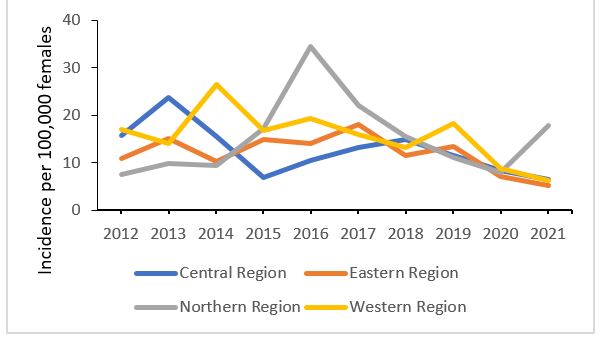
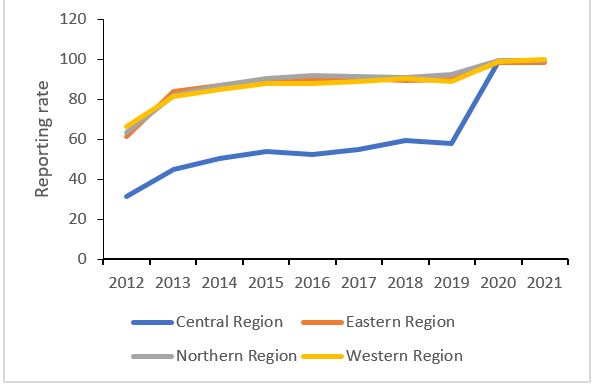
Regionally, Western region had the highest overall incidence (15.6/100,00) while the Eastern region had the lowest overall incidence (12/100,000). There was a general increase in reporting rate across all regions from 2012 to 2021 (Figure 2).
 |
Trend of the incidence of cervical cancer |
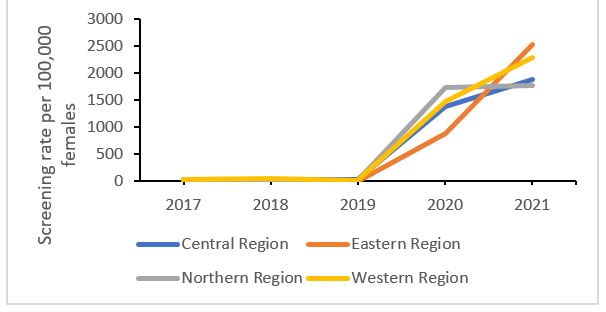 |
Trend of the screening rate |
 |
Trend of the inpatient reporting rate |
Figure 2: Trend of incidence, screening for cervical cancer, and inpatient reporting rates by region, Uganda, 2012–2021
Regional trends analysis shows that the incidence in Northern Uganda increased by 2% over the 10 years while the incidence in the other regions of Uganda decreased over time with Central Uganda having the biggest decrease of 8% (Table 2)
Table 2: Significance of the trends of cervical cancer incidence from 2017 to 2020 at regional level in Uganda
| Region | Odds Ratio | 95% CI | P-Value |
| Central Region 2012/2021 | 0.916 | 0.928 – 0.905 | < 0.001 |
| Eastern Region 2012/2021 | 0.945 | 0.957 – 0.934 | < 0.001 |
| Northern Region 2012/2021 | 1.020 | 1.032 – 1.008 | < 0.001 |
| Western region 2012/2021 | 0.924 | 0.934 – 0.914 | < 0.001 |
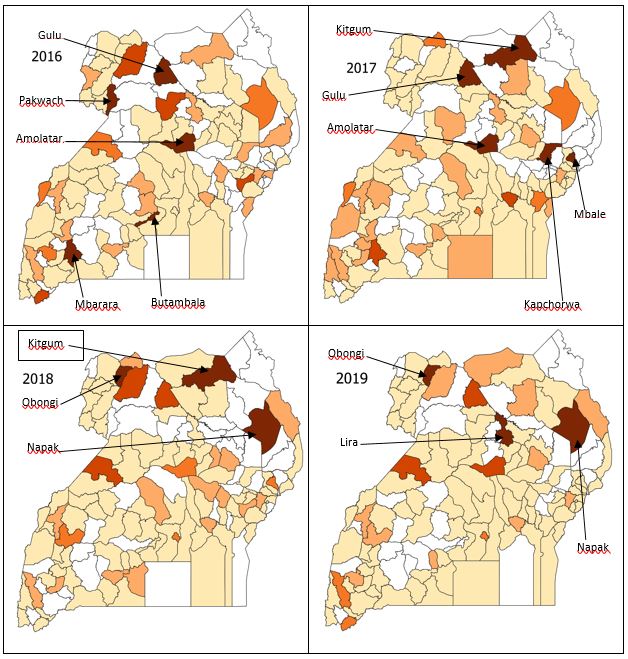
Spatial distribution of cervical cancer in Uganda, 2012-2014
The incidence of cervical cancer was highest in Northern Uganda except for the years 2012 and 2014 where it was highest in Western Uganda. Similarly, Western Uganda had some districts with high incidence of cervical cancer over the years (Figure 3). There were variations of incidence rates over the years by districts nationwide (Figure 3).
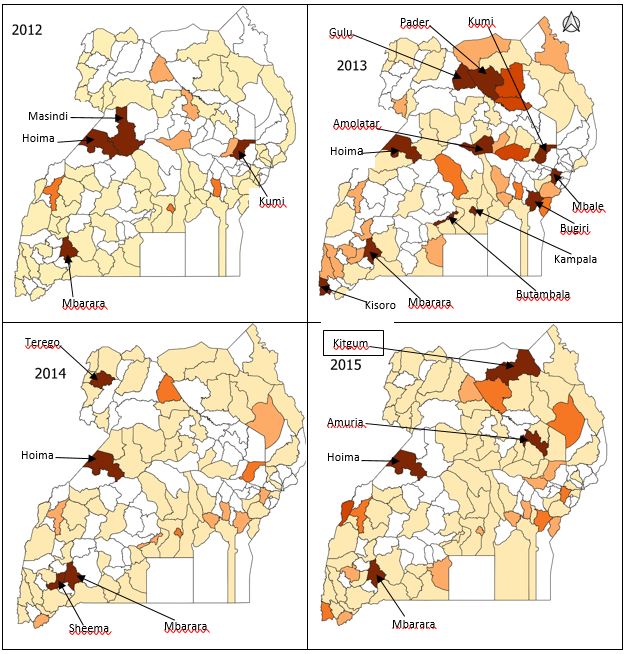
|
Discussion
Our findings showed overall decreasing incidence of cervical cancer in the country from 2012 to 2020. They also showed a significant increase in incidence of cervical cancer from 2012 to 2019 and then a decrease during 2020 and 2021. Regionally, only the Northern region had an increase in the incidence of cervical cancer over the years. The Central region had the most significant decrease in incidence of cervical cancer over time. The trends are similar to many other studies done globally for the past 2 decades that have shown decreasing incidence of cervical cancer (13, 14). However, a study in Kampala by Jedy-Agba et al., showed an increase in incidence of cervical cancer from 1991 to 2015 (15). The reasons for the decreasing trend in Uganda could be due to implementation of safe male circumcision policy since 2010 which encourages all males to be circumcised (16). Although, safe male circumcision was initially introduced as a means of reducing HIV transmission. However, many studies have demonstrated that uncircumcised men have an increased risk of HPV infection which is localised at the glans penis or corona decreasing the risk of HPV infection (17, 18). Furthermore, in 2015, the Government of Uganda under Ministry of Health upscaled HPV vaccination in the whole country as a way of helping to reduce cervical cancer and it can be done in different health facilities for girls aged 9 – 14 years (11).
The initial increase in the incidence of cervical cancer could have been due to increased cervical cancer screening. The initial decline that follows could have been be due to low screening rates: however, the incidence in 2020 and 2021 declines even further despite the increase in screening rates. This could be because of the decline in reporting rates and the lock down and other restrictions on transport and increase in transport charges in 2020 and 2021 may have prevented women who really needed screening services from accessing them. The increase in screening noted in 2020 and 2021 was due to an increase in screening for cervical cancer among eligible women living with HIV (19).
Despite the national decrease in cervical cancer incidence over the years, the Northern region had an increase in the incidence of cervical cancer over time. This is could be because Northern Uganda had the highest reporting rate over time compared to other regions. In addition, Northern Uganda has a high prevalence of childhood marriages (20) which exposes the young girls to sexual intercourse at an early age which increases their risk of cervical cancer. This supports the need for HPV vaccination for eligible girls especially while they are still in school and the need to address childhood marriages as a means of preventing cervical cancer in addition to the existing ways of preventing cervical cancer in the country.
The central region had the most decrease in the incidence of cervical cancer over time. This is contrary to what is expected since the Central region has the highest prevalence for HIV (21) which increases the risk of cervical cancer. However, this could be because of the improvement in Antiretroviral treatment in Uganda which could have led to a decrease in cervical cancer (22). Thus, despite the decrease in the incidence cervical cancer, there is still need to strengthen cervical cancer screening services in the region.
The low incidence of cervical cancer in Eastern Uganda could be due to practice of male circumcision. Studies have showed that women whose male patterners are circumcised are less likely to get infected with HPV. In Eastern Uganda, there is a practice of male circumcision in the Bugishu region. In addition, a study on the impact of safe male circumcision done in Uganda showed that Eastern Uganda had the highest uptake of safe male circumcision (23, 24). Despite the lower incidence in Eastern Uganda, efforts are still needed to reduce cervical cancer.
Despite the current decreasing prevalence of cervical cancer, Uganda still has a long way to reach the WHO target of eliminating cervical cancer by the next generation. Therefore, there is need to strengthen cervical cancer screening in the entire population especially in Northern Uganda. There is also need to emphasize community education about cervical cancer screening to improve detection of cases especially in central Uganda where the incidence is expected to be higher.
Study limitations
Because DHIS2 data is aggregated and does not represent patient-level data like age, we could not describe the individual characteristics to show the change in cervical cancer incidence with age; yet based on literature, older age has been documented to be associated with cervical cancer. There is poor uptake of screening in Uganda as low as 4.8% in rural areas (9), hence a likely underestimation of the incidence in the country. Eastern Uganda had 0 reporting for cervical cancer screening for the years 2018 and 2019, something unlikely to be true, hence a possible underestimation of the magnitude of cervical cancer in the region and the entire country.
Conclusions
Despite the significant increase in cervical cancer screening, fewer cases of cervical cancer were registered in Uganda over the years. Only Northern Uganda had an increase in incidence of cervical cancer over the years. We recommend expansion of screening to cover all eligible female populations and strengthening of strategies to sustain the decline in cervical cancer cases. Further investigations are needed to understand the reasons for the increasing incidence in Northern Uganda.
Conflict of interest
The authors declare that they had no conflict of interest.
Acknowledgements
We would like to thank the Ministry of Health Division of Health Information for permitting us to use these data.
Copyright and licensing
All materials in the Uganda National Institute of Public Health Quarterly Epidemiological Bulletin is in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
-
Isabirye A, Mbonye MK, Kwagala B. Predictors of cervical cancer screening uptake in two districts of Central Uganda. PLOS ONE. 2020;15(12):e0243281.
-
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6) :394-424.
-
International WCRF. Cervical cancer statistics. 2022.
-
WHO. Cervical cancer. 2020. Available at: https://www.who.int/news-room/ fact-sheets/detail/cervical-cancer// [Accessed on 23 Septermber 2022].
-
WHO. Comprehensive cervical cancer control: a guide to essential practice. Geneva. 2014.
-
Adebamowo SN, Olawande O, Famooto A, Dareng EO, Offiong R, Adebamowo CA. Persistent Low-Risk and High-Risk Human Papillomavirus Infections of the Uterine Cervix in HIV-Negative and HIV-Positive Women. Front Public Health. 2017;5:178.
-
Nakisige C, Trawin J, Mitchell-Foster S, Payne BA, Rawat A, Mithani N, et al. Integrated cervical cancer screening in Mayuge District Uganda (ASPIRE Mayuge): a pragmatic sequential cluster randomized trial protocol. BMC Public Health 2020;20(1):142.
-
WHO. Cervical Cancer: Eliminating cervical cancer. 2020.
-
Nakisige C, Schwartz M, Ndira AO. Cervical cancer screening and treatment in Uganda. Gynecologic oncology reports. 2017;20:37-40.
-
Ndejjo R, Mukama T, Musabyimana A, Musoke D. Uptake of Cervical Cancer Screening and Associated Factors among Women in Rural Uganda: A Cross Sectional Study. PloS one. 2016;11(2):e0149696.
-
Kisaakye E, Namakula J, Kihembo C, Kisakye A, Nsubuga P, Babirye JN. Level and factors associated with uptake of human papillomavirus infection vaccine among female adolescents in Lira District, Uganda. Pan Afr Med J. 2018;31:184.
-
Claire Biribawa RN, Frederick Oporia, Ezekiel Baguma, Lilian Bulage, Denis Okethwangu, Alex Riolexus Ario, Olive Kobusingye. Trends of Injuries due to Gender Based Violence, Uganda, 2012 - 2016, a retrospective descriptive analysis. JIEPH. 2020;3.
-
Zhang X, Zeng Q, Cai W, Ruan W. Trends of cervical cancer at global, regional, and national level: data from the Global Burden of Disease study 2019. BMC Public Health. 2021;21(1):894.
-
Shujuan Lin KG, Simeng Gu, Liuqing You, Sangni Qian, Mengling Tang, Jianbing Wang, Kun Chen, and Mingjuan Jin. Worldwide trends in cervical cancer incidence and mortality, with predictions for the next 15 years. 2021.
-
Jedy-Agba E, Joko WY, Liu B, Buziba NG, Borok M, Korir A, et al. Trends in cervical cancer incidence in sub-Saharan Africa. British journal of cancer. 2020;123(1):148-54.
-
Health Mo. Safe male circumsicion policy. 2010.
-
Hernandez BY, Wilkens LR, Zhu X, McDuffie K, Thompson P, Shvetsov YB, et al. Circumcision and human papillomavirus infection in men: a site-specific comparison. The Journal of infectious diseases. 2008; 197(6):787-94.
-
Vanbuskirk K, Winer RL, Hughes JP, Feng Q, Arima Y, Lee SK, et al. Circumcision and acquisition of human papillomavirus infection in young men. Sexually transmitted diseases. 2011;38(11):1074-81.
-
Josephine Connie Ninsiima IL, Evelyn Akello, Tamara Nsubuga- Nyombi, Charity Nuwagaba Kyomugisha, Steven Baveewo, Mina Nakawuka, Simon Muhumuza, Julius Kalamya Namonyo, Rhodah Wanyenze. Roll out of cervical cancer screening and treatment program for HIV-infected women in Uganda: Implications for national scale up. 8th National Quality Improvement Conference2021.
-
UNICEF. Ending Child Marriage and Teenage Pregnancy in Uganda. A Formative Research to Guide the Implemenetation of the National Strategy on Ending Child Marriage and Teenage Pregnancy in Uganda. 2015.
-
MoH. Uganda Population-Based HIV Impact Assessment UPHIA 2016-2017. 2019.
-
Kelly H, Weiss HA, Benavente Y, de Sanjose S, Mayaud P. Association of a ntiretroviral therapy with high-risk human papillomavirus, cervical intraepithelial neoplasia, and invasive cervical cancer in women living with HIV: a systematic review and meta-analysis. Lancet HIV. 2018;5(1): e45-e58.
-
Svare EI, Kjaer SK, Worm AM, Osterlind A, Meijer CJ, van den Brule AJ. Risk factors for genital HPV DNA in men resemble those found in women: a study of male attendees at a Danish STD clinic. Sex Transm Infect. 2002;78(3):215-8.
-
Morris BJ, Hankins CA, Banerjee J, Lumbers ER, Mindel A, Klausner JD, et al. Does Male Circumcision Reduce Women's Risk of Sexually Transmitted Infections, Cervical Cancer, and Associated Conditions? Front Public Health. 2019;7:4.


Comments are closed.