Sexual Gender-Based Violence among Adolescent Girls and Young Women 10-24 Years during COVID-19 Pandemic, Bukedi Region, Eastern Uganda
Authors: Patience Mwine1,3*, Benon Kwesiga1,2, Richard Migisha1,2, Juliet Cheptoris3, Daniel Kadobera1,2, Lilian Bulage1,2, Peter Mudiope3, Alex R. Ario1,2 Institutional affiliations: 1Uganda Public Health Fellowship Program, Kampala, Uganda, 2Uganda National Institute of Public Health, Kampala, Uganda, 3AIDS Control Program, Ministry of Health, Kampala, Uganda *Correspondence: Email : pmwine@musph.ac.ug, Tel : +256702449738
Summary Background: Police reports of Sexual Gender-Based Violence (SGBV) in Uganda increased during the COVID-19 pandemic, primarily affecting adolescent girls and young women (AGYW) aged 10-24 years. In April 2022, we investigated factors associated with SGBV among AGYW during the COVID-19 pandemic in Bukedi Region, which reports the highest rates of SGBV among women (40% in 2016) in Uganda. Methods: We use a mixed methods approach to examine data for SGBV cases among adolescent girls and young women (AGYW) aged 10-24 years at ten high-volume health facilities in Bukedi Region. The data were collected retrospectively for the period of March 2020 to December 2021, covering the highest-burden phases of the COVID-19 pandemic in Uganda. We conducted a neighbourhood-matched case-control study. A case was ≥1 SGBV episode (coerced sex) self-reported by an AGYW aged 10-24 years residing in Tororo and Busia Districts. Cases were identified from facility registers. For every case, we identified two neighbourhood-matched AGYW controls who reported no SGBV. We interviewed 108 randomly-selected cases from the health facility line list and 216 controls and asked about socio-demographics, economic changes they or their families experienced during COVID-19, and experiences with SGBV during COVID-19. We conducted key informant interviews with six health facility SGBV focal persons about possible factors associated with SGBV during the COVID-19 period. We used conditional logistic regression to obtain adjusted odds ratios and confidence intervals for the factors associated with SGBV. We analysed qualitative data using content analysis. Results: Among 389 SGBV cases recorded in the facility registers, the mean age was 16.4 (SD±1.61: range 10-24) years, and 350 (90%) were 15-19 years of age. Two-thirds(214; 67%) were pregnant at the time their SGBV experience was recorded. Only eight(2%) received Post-Exposure Prophylaxis (PEP) for HIV. Among the 108 cases interviewed, 79 (73%) reported being physically forced into sex while 29 (27%) were pressured into sex through harassment and threats. Among those who mentioned the perpetrator (73; 68%), many reported it were a friend (29; 40%) or neighbour (17; 23%). In multivariate analysis, self-reports of sexual violence before the COVID-19 period [aOR=5.8, 95%CI: 2.8-12] and having older siblings [aOR=1.9, 95%:CI 1.1-3.4] were associated with SGBV during the COVID-19 period. Living with a family that provided all the basic needs was protective [aOR=0.42, 95%: CI 0.23-0.78].The qualitative data reveal that poverty and being out of school for an extended period appeared to be associated with increased SGBV cases in the region during the COVID-19 period. Conclusion: Previous SGBV and having families without the means to provide basic needs was associated with increased odds of SGBV during the COVID-19 pandemic in Uganda. Finding, s upporting, and enacting protective interventions for potential and existing SGBV survivors and socioeconomically vulnerable AGYW could prevent SGBV during similar events in the future.
Introduction
Sexual gender-based violence (SGBV) is defined as “any sexual act, attempt to obtain a sexual act, or other act directed against a person’s sexuality using coercion, by any person regardless of their relationship to the survivor, in any setting” (1).
Sexual gender-based violence predisposes survivors to HIV, unwanted teenage pregnancies, and mental illnesses like depression. Among adolescent girls and young women (AGYW), it may result in school dropouts, increased risk of mother-to-child HIV transmission, and socio-economic difficulties (2).
Uganda has a high prevalence of SGBV (22%) among women 15-49 years, according to the Uganda Population-based HIV Impact Assessment (UPHIA) 2016. Bukedi Region had the highest prevalence of SGBV among women at 40% and a teenage pregnancy rate of 22%, according to UPHIA 2016 (3).
In Uganda, from March 2020 to January 2022, schools were closed as part of the COVID-19 pandemic response. Anecdotal reports from Uganda Police and an analysis of national SGBV program data suggested that SGBV cases had increased during the COVID-19 pandemic, especially during the two lockdown periods in 2020 and 2021 (4).
Probable causes included prolonged out of school period and the implementation of multiple lockdowns, leading to girls exposure to perpetrators within homes and neighbourhoods during times they would otherwise have been elsewhere (5).
While SGBV among AGYW does not necessarily lead to pregnancy, an analysis of District Health Information System (DHIS2) data showed a 33% increase in teenage pregnancies (among girls age 10-19 years) between 2020 and 2021 compared to 2019 in the Bukedi Region; which was believed to be linked to the increases in SGBV during this the COVID-19 pandemic period.
SGBV survivors receive Post Exposure Prophylaxis (PEP), emergency contraception, testing and treatment for STIs, and treatment of injuries or wounds (6). However, it was unclear how the health facilities addressed SGBV cases during the COVID-19 pandemic.
In addition, there was limited information on factors associated with SGBV among adolescent girls and young women during the COVID-19 pandemic. We evaluated SGBV services and determined the factors associated with SGBV among AGYW during the COVID-19 pandemic in the Bukedi Region to inform areas of improvement and prevention measures for SGBV.
Methods
Study design and setting
We employed a mixed-methods approach, including a descriptive, qualitative, and case-control study among AGYW aged 10-24 years in Tororo and Busia districts, Bukedi Region. These two districts are in Eastern Uganda, bordering Kenya. Both have active trading activities and border points with many transit truck drivers. These districts reported the highest number of teenage pregnancies during COVID-19 period in Bukedi region (7).
Case definition and finding
We defined a SGBV case as an AGYW aged 10-24 years who was recorded in the GBV register during March 2020 to December 2020. To find cases recorded during the pandemic period, we purposively selected ten high-volume health facilities providing SGBV care, including one District Hospital, one Health Center IV, and three high-volume Health Center IIIs from each of the two districts. In each facility, we created a line list of records of SGBV cases among AGYW aged 10-24 from the GBV HMIS 105 registers for the period of March 2020 to December 2021.
Health care workers record information for GBV survivors who are identified through self-reporting or from routine screening for GBV, including in HIV care and treatment clinics and antenatal care clinics.
Using a predesigned data abstraction form, we obtained patient information on the visit date, social demographic characteristics, management of SGBV cases, including HIV post-exposure prevention (PEP), family planning, outcome, and follow-up. Additional information on PEP provision was obtained from the PEP registers.
Descriptive epidemiology
We analysed the line listed SGBV cases’ data Using Epi-Info version 7.2.4.0. We described the SGBV cases by place and person and the quality of SGBV services received by the survivors. We used some of these analyses to identify the study site for the case control study.
Case-control study to identify factors associated with sexual gender-based violence during the COVID pandemic period, Tororo and Busia District, Uganda
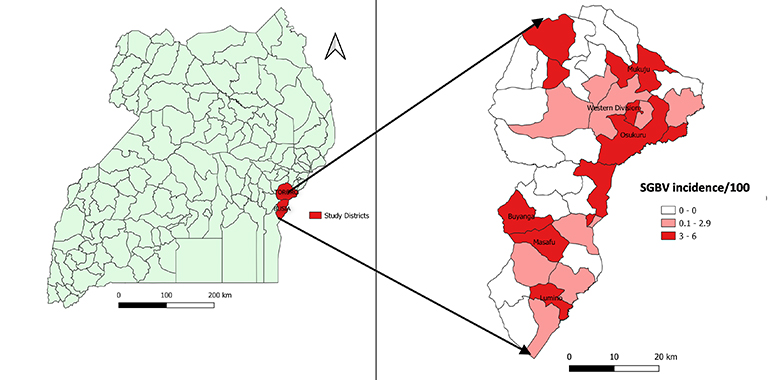
The SGBV incidence rates (IR) among subcounties ranged from 0.1% to 6%. Among the 11 subcounties with IR ≥3%, we randomly selected six (three from each district). These included Mukuju, Western division, and Usukuru subcounties from Tororo district and Masafu, Lumino, and Buyanga subcounties from Busia District (Figure 1). These six subcounties served as the sites for the case-control study.
We conducted a neighbourhood-matched case-control study to determine factors associated with SGBV among AGYW during COVID-19 (March 2020 to December 2021), covering the highest-burden phases of the COVID-19 pandemic in Uganda.
We defined a case as an AGYW aged 10-24 years who reported at least one episode of SGBV to any of 10 high-volume health facilities in Tororo and Busia Districts during this time. For every case, we identified two neighbourhood-matched AGYW controls who reported no SGBV. A control was an AGYW aged 10-24 years who did not experience an episode of SGBV during COVID-19 period.
We assumed a reduction in family income during the pandemic was a significant risk factor for SGBV with an odds ratio of 2 and 40% of the controls exposed. At a ratio of 1:2 cases to controls and 80% power, we obtained a sample size of 324 (108 cases and 216 controls).
Using a line list of SGBV cases from the ten health facilities, we randomly selected SGBV cases for interviews. We traced the cases for interviews in the community with the help of the social workers and village health teams and consecutively interviewed them until we reached 108 cases. We identified two neighbourhood-matched control AGYW who reported no SGBV during the COVID-19 period for every case; controls were asked to confirm that they never experienced SGBV during COVID-19 (March 2020 to December 2021). The controls were identified from a randomly selected neighbour households of cases that had an AGYW living with them. For each household, we interviewed one control. If controls were >1 in a house hold, we used a random number to select a participant for interviews.
Using a predesigned questionnaire, we interviewed cases and controls to obtain information on socio-demographics, risk factors for SGBV, care and services received, economic activities undertaken during COVID-19 by the participant and their immediate family place of residence before and during COVID-19, school attendance before and during COVID-19, household size, household members living in the house, household members’ occupation, day and night-time activities of the case, parental supervision, and others.
We adopted the recent Uganda’s Violence Against Children (VAC) Survey (2018) questionnaire, (8) and tailored it to our study. To determine the factors associated with SGBV, we conducted conditional logistic regression analysis.
Key informant interviews to identify factors associated with SGBV during the pandemic
We attempted to interview all GBV focal persons who manage SGBV cases as key informants at the ten facilities; however, only six facilities had the GBV focal person present during data collection. Using a predesigned key informant guide that had open ended questions.
We asked about possible root causes of increased SGBV cases in the region and explored challenges related to high rates of teenage pregnancies, management of SGBV during the pandemic, and availability of drugs such as emergency contraceptives and PEP.
The interviews were recorded and transcribed into word document. We proof read the transcripts, identified the common codes. These were then developed into broader themes. Results were summarised into short texts and quoted verbatim and were used to support the quantitative findings.
Ethical considerations
This was the Ministry of Health (MoH) directive to evaluate the factors associated with the increased numbers of Sexual Gender-based Violence during COVID-29. However, we also sought permission from the district health officials and heads of the health facilities before conducting the study. A non-research determination form was submitted to US CDC for clearance before the commencement of the assessment as a requirement.
The Office of the Associate Director for Science, U.S. Centers for Disease Control and Prevention, determined that this activity was in response to a public health issue with the primary intent of public health practice (epidemic disease control activity). It was determined, therefore, to not be human subjects research. All protocols were approved by the Ministry of Health and US CDC and performed in accordance with the declaration of Helsinki.
We obtained verbal consent from respondents before the interviews. During data collection, we assigned respondents unique identifiers instead of names to protect their confidentiality; no unique identifier information was recorded.
Results
Description of sexual Gender-based Violence cases
We found 389 SGBV cases of AGYW recorded at the ten selected health facilities in Tororo and Busia Districts from March 2020 to December 2021. Their mean age was 16.4 years (SD± 1.61: range, 10-24 years) and most (350; 90%) were 15-19 years of age.
The majority (214; 67%) were pregnant at the time their SGBV event was recorded in the facility register. Many (180; 46%) presented to the facility at time points beyond 72 hours. Among the 209 who presented within 72 hours, only 8 received PEP (Table 1).
Table 1: Characteristics of sexual gender-based violence cases managed at health facilities during the COVID-19 period in Bukedi sub-region, 2020-2021
| Variable | Frequency n=389 | (%) |
| Age | ||
| 10-14 | 25 | (6.4) |
| 15-19 | 350 | (90) |
| 20-24 | 14 | (3.6) |
| Marital status | ||
| Married | 198 | (51) |
| Not married | 191 | (49) |
| HIV test done | ||
| Yes | 321 | (83) |
| No | 65 | (17) |
| Followed up by HCW after initial visit at least once | ||
| Yes | 16 | (4.1) |
| No | 373 | (96) |
| Followed up by HCW after initial visit at least 4 times (as recommended) | ||
| Yes | 0 | (0) |
| No | 389 | (100) |
| Pregnant | ||
| Yes | 214 | (67) |
| No | 107 | (33) |
| Time between event and presentation for care | ||
| <24 hours | 97 | (25) |
| 24-72 hours | 112 | (29) |
| >72 hours | 180 | (46) |
| PEP among person who presented <72 hrs (n=209) | ||
| Yes | 8 | (3.8) |
| No | 209 | (96) |
HCW- Health care worker
Findings from analysis of the health facility data were confirmed by responses from the key informant interviews. Most GBV focal persons reported that AGYW experiencing SGBV reported too late to the health facility to be eligible for post-exposure prophylaxis.
Many of these cases were only identified as SGBV survivors during their antenatal care visits, often for pregnancies that resulted from the SGBV event or events. As a result, they were not eligible for emergency oral contraceptives despite the fact that medicines were available.
“The management of the SGBV cases was a big challenge during the COVID-19 period. Most girls presented here very late, some already pregnant and whenever you asked them why they never came early, they reported they feared the perpetrators. You had nothing to do for them apart from counselling” Key informant II
Description of sexual gender-based violence cases considered for the case-control study
Of the 108 cases interviewed, 79 (73%) reported being physically forced into sex while 29 (27%) reported that they were pressured into sex through harassment and threats. Most (88; 82%) reported that the episode was their first SGBV experience during COVID-19 period.
Among 73 (68%) who agreed to share information about the perpetrator, 29 (40%) reported it was a friend and 17 (23%) said it was the neighbour. The majority (71; 67%) reported to the health facility after 72 hours or more; of these, 42 (58%) said that they delayed reporting due to feelings of social stigma about their SGBV experience. The most reported adverse outcome from the episode was unwanted pregnancy (38; 35%) (Table 2).
Table 2: Characteristics of sexual gender-based violence cases considered for the case control study during the COVID-19 period in Bukedi sub-region, 2020-2021
| Type of SGBV | N=108 | (%) | |
| Physically forced sex | 79 | (73) | |
| Pressured into sex through harassment | 29 | (27) | |
| First time experience of SGBV during COVID-19 | 88 | (82) | |
| Time of Sexual event | |||
| Day | 23 | (21) | |
| Evening | 21 | (19) | |
| Night | 44 | (40) | |
| Declined to answer | 20 | (19) | |
| Type of perpetrator (among 73 providing information) | |||
| Friend | 29 | (40) | |
| Neighbour | 17 | (23) | |
| Relative | 9 | (12) | |
| Others | 18 | (25) | |
| Where the incident occurred | |||
| On the way somewhere | 25 | (21) | |
| Friends place | 25 | (23) | |
| Home | 26 | (24) | |
| Relative home | 11 | (10) | |
| Workplace | 2 | (1.9) | |
| Not comfortable to mention the place | 20 | (19) | |
| Adverse outcomes | |||
| Unwanted pregnancy | 38 | (35) | |
| Depression | 20 | (19) | |
| Anxiety | 12 | (11) | |
| STI | 7 | (6.5) | |
| Others | 14 | (13) | |
| Reported they received emergency contraception | 35 | (32) | |
| Time from SGBV event to presentation to health facility | |||
| Immediately | 18 | (27) | |
| 1-3 days | 18 | (27) | |
| >3 days | 72 | (67) | |
| Self-reported they received PEP from health facility or other site (among 102 who provided a response) | 35 | (34) | |
| Self-reported they received PEP from health facility or other site (among 36 who presented <3 days after event) | 20 | (56) | |
| Reasons for reporting to the health facility > 3 days (n=72) | |||
| Social stigma | 42 | (58) | |
| Fear of retaliation | 13 | (18) | |
| Lack of awareness | 13 | (18) | |
| Others | 4 | (5.6) | |
*PEP; Post Exposure Prophylaxis, STI: Sexually Transmitted Infection
Factors associated with sexual gender-based violence among adolescent girls and young women during COVID-19, Tororo and Busia districts, Uganda
In bivariate analysis, having older siblings [cOR=1.7, 95% CI: 1.04-2.8], ever being pregnant before the COVID-19 period [cOR=2.5, 95%CI: 1.6-4.0], ever being sexually violated before the COVID-19 period [cOR=8.1, 95% CI: 4.1-16], ever being involved in sex work [cOR=3.4,95% CI: 2.1-5.6] were associated with SGBV during COVID-19.
In contrast, having a family being able to provide all basic needs was protective [cOR=0.33, 95% CI: 0.20-0.56] (Table 3). Age, being in school before COVID-19 period, level of education, ever having had children, knowledge and use of family planning, and family change in economic status during the COVID-19 period were not significantly associated with SGBV.
In multivariable analysis, experiencing sexual violence before COVID-19 [aOR=5.8, 95% CI: 2.8-12] and having older siblings [aOR=1.9, 95%CI: 1.1-3.4] remained significantly associated with SGBV during COVID-19 period. The family’s ability to provide all basic needs [aOR=0.42, 95%:CI 0.23-0.78] was protective. While the odds of SGBV decreased with increasing age, the association was not significant (Table 3).
Table 3: Characteristics of cases and controls and their association with Sexual Gender Based Violence during the COVID-19 period in Bukedi sub-region, 2020-2021
| Characteristic | Cases (n=108) | Controls (n=216) | Bivariate Analysis | Multivariate Analysis | ||||
| n | (%) | n | (%) | cOR | 95% CI | aOR | 95% CI | |
| Age in years | ||||||||
| 10–14 | 16 | (15) | 47 | (22) | Ref | |||
| 15-19 | 67 | (62) | 107 | (50) | 1.8 | (0.97-3.5) | 0.94 | (0.44-2.03) |
| 20-24 | 26 | (24) | 61 | (28) | 1.3 | (0.60-2.6) | 0.52 | (0.20-1.3) |
| Has older sibling(s) | 77 | (71) | 126 | (58) | 1.7 | (1.04-2.8) | 1.9 | (1.1-3.4) |
| Ever pregnant before COVID-19 period | 63 | (58) | 76 | (35) | 2.5 | (1.6-4.0) | 1.7 | (0.86-3.2) |
| Sexually violated before COVID-19 period | 40 | (37) | 8 | (3.7) | 8.1 | (4.1-16) | 5.8 | (2.8-12) |
| Ever involved in sex work | 54 | (50) | 47 | (22) | 3.4 | (2.1-5.6) | 1.7 | (0.9-3.2) |
| Family provides all basic needs | 63 | (58) | 172 | (80) | 0.33 | (0.20-0.56) | 0.42 | (0.23-0.78) |
| Knows about family planning | 58 | (54) | 110 | (51) | 1.06 | (0.67-1.7) | – | – |
| Ever used family planning | 29 | (27) | 51 | (24) | 1.1 | (0.66-1.9) | – | – |
| Ever had children | 44 | (41) | 56 | (26) | 0.83 | (0.39-1.7) | – | – |
| Stayed with during COVID-19 | ||||||||
| Parent | 69 | (64) | 151 | (70) | Ref | – | – | – |
| Friends/relatives | 40 | (37) | 64 | (30) | 1.3 | (1.04-1.6) | – | – |
| Highest education level | ||||||||
| None | 3 | (2.8) | 2 | (0.9) | Ref | – | – | – |
| Primary | 73 | (68) | 130 | (60) | 0.37 | (0.06-2.2) | – | – |
| Secondary | 32 | (30) | 69 | (32) | 0.31 | (0.05-1.9) | – | – |
| Tertiary | 0 | (0.0) | 6 | (2.8) | 1 | – | – | – |
| In school before COVID-19 | 86 | (80) | 182 | (84) | 0.64 | (0.35-1.2) | – | – |
| Family economic status changed during COVID-19 | 87 | (80) | 154 | (77) | 1.2 | (0.68-2.1) | – | – |
Results from the informant interviews supported these findings. Five out of six GBV focal persons pointed out that families of their clients were unable to provide basic needs to their families, including the girls exposed to SGBV.
“During COVID 19, there was a lot of poverty as a result of disrupted businesses and closure of schools. As a result, most parents were unable to support their children. Girls were idle, and such could have forced them to look for necessities from elsewhere” Key informant IV
Discussion
Adolescent girls and young women in the Bukedi region experienced high rates of sexual gender-based violence during the COVID-19 period. Many reported cases were pregnant at the time their SGBV experience was recognized and recorded.
Close to half delayed at least three days to report their experience, making them ineligible for PEP; however, even among those that reported earlier, few received PEP.
Previous experiences of sexual violence and having older siblings increased the odds of SGBV, while having sufficient resources within the family to cater to the needs of the AGYW was protective.
Sexual violence exposes AGYW to HIV acquisition; Uganda reports a national HIV prevalence of 4.3% among adult men ≥15 years, a concern for public health (9).
This poses a high risk of HIV transmission to survivors of SGBV. PEP is an important intervention to reduce the risk of contracting HIV after an unprotected sexual encounter, and in Uganda, it is available in public and private health facilities (10).
Care provided after SGBV includes psychosocial support, PEP to prevent HIV, and emergency contraception to prevent pregnancy.
However, both emergency contraceptives and PEP must be given within 72 hours of the event to be effective (11). We identified many missed opportunities for preventing HIV infection and pregnancy among AGYW who experienced SGBV in Bukedi Region.
Interviews with the GBV focal persons, as well as the high rate of pregnancy among AGYW identified as SGBV survivors from the clinic registers, suggested that many AGYW presented because of their pregnancy rather than the SGBV event itself. AGYW cited fears of the perpetrator and stigma as reasons they did not present immediately. Given that many SGBV events will not result in pregnancy, the high frequency of pregnancy among SGBV survivors who report suggests that the reports described in this paper are the tip of the iceberg.
Many women who do not become pregnant because of the SGBV likely simply do not report. Fear of public stigma is a well-documented factor that hinders patients from accessing health care services (9,10). Unfortunately, social stigma related to SGBV is known to worsen physical and psychological health impacts (13) and may increase the risk of additional violence (14).
Efforts are needed to support AGYW to report SGBV and enable adequate and timely care to prevent HIV and unwanted pregnancies. The Uganda Child Help Line (UCHL) 116 was found to be more acceptable channel to report sexual violence compared to others such as health facilities (15).
UCHL was implemented by Ministry of Gender Labour and Social Development (MGLSD) to improve reporting of child abuse and sexual violence but there is still low awareness and a need for more advocacy. In addition, active case finding for SGBV survivors may be necessary to ensure appropriate care and support to the affected persons.
Even among the AGYW who presented early, few received PEP. However, even among those who received PEP, it appears it was often inappropriately given, highlighting a knowledge gap on PEP use among the health care workers and the users.
Due to data gaps in the SGBV healthy facility registers, we could not verify the appropriateness of PEP use for all reported incidents. Similar findings were noted in a study done in Uganda to compare post-rape care before and during COVID-19 using national Health Management Information System (HMIS) and UCHL data.
In this study, 50% of the cases received PEP beyond the recommended 72 hours during the first six month of COVID-19 (16). This highlights the need for flexible methods of service delivery to increase timely access and utilisation of PEP among SGBV survivors. These might include community based approaches such as “off-facility PEP medication delivery” and “PEP hotlines” (16).
These community-based approaches were piloted in rural populations in Kenya and Uganda; results showed increased uptake and completion of PEP in the population. In addition, there is need to train health care workers on PEP eligibility so that it is only given when it will be effective, and not when it is not appropriate.
Having experienced SGBV before the COVID-19 period and having older siblings were both associated with SGBV during COVID-19. Repeated sexual violence during COVID-19 suggests that affected girls may be continually exposed to the same perpetrator(s). Other studies have also found that individuals who are sexually victimised were likely to be re-victimised (15, 16,17).
Therefore, psychosocial support and ways to protect the once identified survivors are necessary to prevent repeated SGBV experiences. In addition, there is need to strengthen the ‘parents/guardians’ daughter relationship to enable the girl’s open up to parents in case of SGBV through evidence based interventions such as community parenting programs (19).
It is not clear why having older siblings was associated with increased risk of SGBV. However, it may simply reflect a younger age of the SGBV victim compared to non-SGBV survivors; age was found to be negatively associated with SGBV in our study.
We found that having a family providing all the basic needs to AGYW was protective against SGBV during COVID-19. Unfortunately, as a result of COVID-19 measures like the closure of bars, shops, saloons, and markets and movement restrictions (20) many families were unable to provide basic needs for their children (21, 22). Efforts to support vulnerable AGYW with basic needs like food, clothing, and shelter among others may be necessary during future pandemics or similar situations to prevent SGBV.
Study limitations
Our study was subject to several limitations. Firstly, health facility data were incomplete, and this could have resulted in inconclusive information on the health care services. We found irregularities with documentation of health facility registers, especially information on dates of incidence and follow-up services, and data on repeated episodes of SGBV. We could not tell from the data if the persons who were offered PEP accepted or completed the dosage. In addition, information on the first point of care was missing, hence we could not establish if the cases who were recorded as pregnant were identified due to pregnancy through the antenatal clinics. We used the health facility data to identify the cases, and thus our data certainly represent an underestimate of the problem as well as reflecting possible bias if the survivors who did not present to the facility differ from those who do. Also, given the sensitivity of the subject and self-reporting of the data, some cases did not respond to questions related to the perpetrator resulting into potential bias.
Conclusion
Sexual gender-based violence negatively affected the lives of many adolescent girls and women during the COVID-19 pandemic. Most survivors did not present in time for HIV exposure prophylaxis and therefore efforts to improve access to services through community education and engagement with AGYW is key for PEP uptake when needed. Public health programs in the future may need to focus on identifying or supporting known survivors of SGBV and those who are socioeconomically vulnerable and identifying approaches to protect them, especially during school closures or other events that leave them close to home.
Conflict of interest
The authors declare that they had no conflict of interest.
Acknowledgments
We appreciate the health facilities and the data collection teams, especially the health facility GBV focal persons, for the support rendered to interview the cases. We commend the AGYW who participated and shared their experiences to inform the factors associated with SGBV during the COVID-19 period.
Copyright and licensing
All materials in the Uganda National Institute of Public Health Quarterly Epidemiological Bulletin is in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
-
Violence against women [Internet]. [cited 2021 Dec 20]. Available from: https://www.who.int/westernpacific/health-topics/violence-against-women
-
WHO | Gender-based violence in health emergencies [Internet]. WHO. World Health Organization; [cited 2022 Jan 6]. Available from: http://www.who.int/health-cluster/about/work/task-teams/genderbasedvio lence/en/
-
udhs - Bing [Internet]. [cited 2022 Jan 6]. Available from: https://www.bing.com/search?q=udhs&form=WNSGPH&qs=MT&cvid=f94bf64014 b146fab0c9de60c5c77ec6&pq=UDHS&cc=UG&setlang=en-UG&nclid=AC7F2871CA28 10F4E3ACF4DC56F34B94&ts=1641451817090&wsso=Moderate
-
Sexual violence against women and girls in Uganda increased during the COVID-19 pandemic [Internet]. aidsmap.com. [cited 2022 Jan 6]. Available from: https://www.aidsmap.com/news/jul-2021/sexual-violence-against- women-and-girls-uganda-increased-during-covid-19-pandemic
-
Covid reveals flaws in the protection of girls in Uganda: Recommendations on how to tackle sexual and gender-based violence - Uganda [Internet]. ReliefWeb. [cited 2022 Jan 6]. Available from: https://reliefweb.int/report/uganda/covid-reveals-flaws-protection- girls-uganda-recommendations-how-tackle-sexual-and
-
Interagency-GBV-Case-Management-Guidelines_Final_2017.pdf [Internet]. [cited 2022 Jan 21]. Available from: http://www.gbvims.com/wp/wp-content/ uploads/Interagency-GBV-Case-Management-Guidelines_Final_2017.pdf
-
Independent T. Over 47,000 girls impregnated in Bukedi during COVID [Internet]. The Independent Uganda: 2021 [cited 2022 Aug 23]. Available from: https://www.independent.co.ug/over-47000-girls-impregnated-in- bukedi-during-covid/
-
Ministry fo Gender, Uganda. Violence Against Children Survey 2018. 2018.
-
MOH, Uganda U. Preliminary results of 2020 the Uganda Population Population-based HIV Impact assessment [Internet]. 2022 [cited 2022 Jul 21]. Available from: https://www.mediacentre.go.ug/media/release-preliminary- results-2020-uganda-population-based-hiv-impact-assessment
-
Ministry of Health, Uganda. The National policy guidelines on Post Exposure Prophylaxis for HIV, Hepatitis B and Hepatitis C. 2007.
-
World Health Organization, Organization IL. Post-exposure prophylaxis to prevent HIV infection : joint WHO/ILO guidelines on post-exposure prophylaxis (PEP) to prevent HIV infection [Internet]. World Health Organization; 2007 [cited 2022 Jul 21]. Available from: https://apps.who.int/iris/handle/10665/43838
-
Subu MA, Wati DF, Netrida N, Priscilla V, Dias JM, Abraham MS, et al. Types of stigma experienced by patients with mental illness and mental health nurses in Indonesia: a qualitative content analysis. International Journal of Mental Health Systems. 2021 Oct 18;15(1):77.
-
Schmitt S, Robjant K, Elbert T, Koebach A. To add insult to injury: Stigmatization reinforces the trauma of rape survivors – Findings from the DR Congo. SSM - Population Health. 2021 Mar 1;13:100719.
-
Barnett JP, Maticka-Tyndale E, Kenya T. Stigma as Social Control: Gender-Based Violence Stigma, Life Chances, and Moral Order in Kenya. Social Problems. 2016;63(3):447–62.
-
Gumbie, et, al. Child Abuse — Research: Sauti 116 Uganda Child Helpline, A rapid assessment of the gaps in the reporting system and public’s knowledge and awareness of the service [Internet]. GLI. 2020 [cited 2022 Jul 19]. Available from: https://www.globallivingston.org/dir/research/tag/Child+Abuse
-
Apondi R, Awor A, Nelson L, Cheptoris J, Ngabirano F, Egbulem CD, et al. Gender-based violence shadows COVID-19: Increased sexual violence, HIV exposure and teen pregnancy among girls and women in Uganda. Journal of the International AIDS Society. 2021 Jul 1;24(S4):53–5.
-
Ayieko J, Petersen ML, Kabami J, Mwangwa F, Opel F, Nyabuti M, et al. Uptake and outcomes of a novel community-based HIV post-exposure prophylaxis (PEP) programme in rural Kenya and Uganda. Journal of the International AIDS Society. 2021;24(6):e25670.
-
Mohammed F. The Repetition Compulsion: Why Rape Victims Are More Likely To Be Assaulted Again [Internet]. Girls’ Globe. 2015 [cited 2022 Jun 13]. Available from: https://www.girlsglobe.org/2015/08/04/the-repetition-compulsion- why-rape-victims-are-more-likely-to-be-assaulted-again/
-
Daniel et al. A Ugandan Parenting Programme to Prevent Gender-Based Violence: Description and Formative Evaluation [Internet]. [cited 2022 Sep 9]. Available from: https://journals.sagepub.com/doi/full/10.1177/10497315211056246
-
AfricaNews. Uganda imposes another lockdown: What are the restrictions? [Internet]. Africanews. 2021 [cited 2022 May 21]. Available from: https://www.africanews.com/2021/06/07/uganda-imposes-another-lockdown-what-are -the-restrictions/
-
Danish Refugee Council. Uganda Cash Consortium stories: Basic needs approach implementation in Imvepi, Rhino Camp & Nakivale refugee settlements - Uganda | ReliefWeb [Internet]. [cited 2022 May 21]. Available from: https://reliefweb.int/report/uganda/uganda-cash-consortium-stories-basic-needs -approach-implementation-imvepi-rhino-camp


Comments are closed.