Prolonged animal anthrax outbreak amplified by slaughtering infected carcasses on the pastureland in Arua District, Uganda, 2016 – 2018
Authors: Fred Monje1, Vivian Ntono1, Esther Kisaakye1, Benon Kwesiga1, Daniel Kadobera1, Alex Riolexus Ario1; Affiliation: Uganda Public Health Fellowship Program, Kampala, Uganda
Summary
In 2017, Uganda Ministry of Health reported a human anthrax outbreak in Arua District. Subsequent epidemiologic investigations conducted confirmed animals as the source of the infection.
We conducted an investigation to assess the scope of anthrax in domestic ruminants; identify possible exposures and recommend evidence based control measures. We identified 140 case-kraals and line listed 1600 animal cases by 22nd July, 2018. Rigbo sub-county was the most affected (AR/1000= 37). We conducted a frequency matched case control study . We found that skinning infected carcasses on the pastureland (OR=7.5; CI = 3.9 – 14) and grazing animals near the river bank where previous suspected anthrax animals died (OR=2.3; CI=1.2 – 4.4) were the main exposures. We recommended immediate anthrax vaccination of domestic ruminants at risk followed by annual vaccinations and sensitization of communities; animal and medical health workers about anthrax.
Introduction
In 2017, Uganda Ministry of Health reported a human anthrax outbreak in Arua District. Subsequent epidemiologic investigations confirmed animals as the source of infection. We conducted an investigation to assess the magnitude of anthrax infection in domestic ruminants; identify possible exposures and recommend evidence based control measures.
Methods
We defined suspected case as sudden death in a domestic ruminant of Arua District with unclotted blood from body orifices between January 1, 2016 to July, 2018. A probable case was a suspected case with a positive RDT test consistent with B. anthracis. A confirmed case was a suspected case tested positive by PCR. We reviewed district veterinary anthrax records and conducted active community animal case finding to update the line list. We conducted environmental assessment of the anthrax affected areas, including laboratory testing of specimens from dead animals. We conducted a case control study in which we defined a case-kraal as one with sudden death of animal (s) with unclotted blood from body orifices between January, 2016 to July 2018 in the selected villages. We defined a control-kraal as a kraal which had not had any sudden animal (s) death (s) with unclotted blood from body orifices in the same period from the selected villages. We matched cases and controls by frequency in each village in a ratio of 1:1.
Results
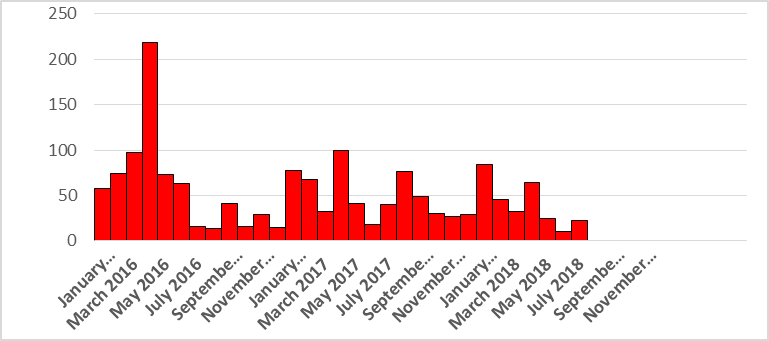
We identified 140 case-kraals and line listed 1600 animal cases and found that distribution of the kraals showed an epidemic curve of a continuous common source pattern. Animal deaths due to suspected anthrax increased gradually and peaked in the month of April. There was an increase in animal deaths in the months of January and February in 2017 and 2018 (Figure 1).
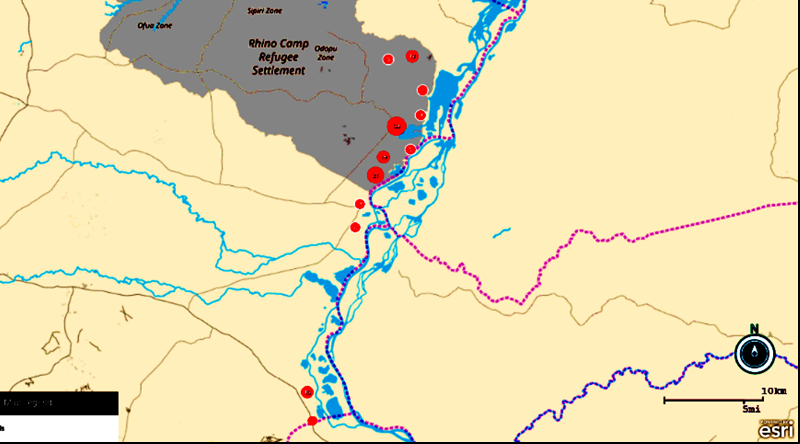
Rigbo sub-county (AR/1000=37) was the most affect- ed followed by Pawor (AR/1000=12)and Rhino camp (AR/1000=1.4). The case-kraals were distributed mainly along the Nile river, with majority of them situated in Ajai game reserve in Arua District (Figure 2)
Environmental assessment and laboratory
We observed remains of animal carcasses in the grazing fields. Migration routes in the pasture land were evident. We saw animals graze near the river bank of the Nile river. We witnessed communal grazing in affected sub counties. 5/6 livestock carcasses tested positive by rapid diagnostic test (RDT) consistent with B. anthracis.
Case-control findings: Slaughtering infected carcasses
on the pasture land (OR= 7.5; CI=3.9 – 14) , buying animals from another sub-county or district (OR=4.5; CI=2.2-9.2), grazing animals near the river bank were previous suspected anthrax animals died (OR=2.3; CI=1.2 – 4.4) and giving animals antibiotic treatment before the outbreak were associated with anthrax infection in animals.
Discussion
Our investigation found that the outbreak in Arua District was associated with slaughtering anthrax infected dead animals on the pastureland, and grazing animals near the river bank were previous animal deaths due to suspected anthrax occurred. Slaughtering anthrax infected dead animals on the pastureland exposes anthrax spores that contaminate the pastureland posing a risk to cattle, goats and sheep. Similarly, grazing animals on the pastureland where an anthrax animal case died also poses a risk to animals since a dead anthrax animal oozes blood with spores from all body orifices that remain viable on the pastureland for decades. The spores shed by an animal dying or dead from anthrax are the source of infection for other animals (2). Our findings are consistent with other studies in Bhutan, Asia Bangladesh and North Dakota, USA (3,4,5). We also found more animal cases towards the end of the dry season (March to May) and beginning of the rainy season (August to September) indicating seasonality
of the anthrax outbreak. During prolonged dry season the animals congregate at the water points along the river bank and graze close to the ground hence ingesting the anthrax spores. Cattle were more affected than goats probably because they ingest more soil while grazing but goats typically browse on grass only making them less ex-posed to anthrax spores in soil. This is consistent with findings from a study in China.(8).
Conclusions and Recommendations
Slaughtering anthrax infected animals on the pastureland, grazing animals near the river bank were previous animal deaths due to suspected anthrax occurred and buying animals from another sub-county or district were associated with anthrax infection among animals in Arua district. We
recommended immediate and annual anthrax vaccination of domestic ruminants at risk by MAAIF and Arua District. Also enhanced sensitization of the communities; animal health workers and medical health workers about anthrax exposure.
References
1. Carlson CJ, Getz WM, Kausrud KL, Cizauskas CA, Blackburn JK, Carrillo FAB, et al. Spores and soil from six sides: interdisciplinarity
and the environmental biology of anthrax (Bacillus anthracis). Biol Rev [Internet]. [cited 2018 Sep 19];0(0).
2. World Health Organization, International Office of Epizootics, Food and Agriculture Organization of the United Nations, editors.
Anthrax in humans and animals. 4th ed. Geneva, Switzerland: World Health Organization; 2008. 208 p.
3. Thapa NK, Wangdi K, Dorji T, Dorjee J, Marston CK, Hoffmaster AR. Investigation and Control of Anthrax Outbreak at the Human–
Animal Interface, Bhutan, 2010. Emerg Infect Dis. 2014 Sep;20 (9):1524–6.
4. Hassan J, Ahsan M, Rahman M, Chowdhury S, Parvej M, Nazir K. Factors associated with repeated outbreak of anthrax in Bangladesh:
qualitative and quantitative study. J Adv Vet Anim Res. 2015

