Patterns of tuberculosis case notification and treatment outcomes in the context of COVID-19 pandemic: analysis of national surveillance data, January 2019 – June 2021
Authors: Veronicah Masanja1,2*, Robert Kaos Majwala2, Stavia Turyahabwe2, Doreen Nsimiire Gonahasa 1, Benon Kwesiga1, Daniel Kadobera1, Lilian Bulage1, Alex Riolexus Ario1 Institutional affiliations 1Uganda Public Health Fellowship Program,Uganda National Institute of Public Health, Kampala, Uganda, 2National TB and Leprosy Control Program, Ministry of Health, Kampala, Uganda *Correspondence: Tel: +256775511542, Email: vmasanja@musph.ac.ug
Summary
Background: Tuberculosis case notification and outcomes monitoring are critical for TB control but can both be disturbed by interruptions to normal health system functioning. The first major wave of COVID-19 in Uganda occurred during August-December 2020. The government-imposed lockdown measures during March-June 2020 in which residents were required to stay at home. Kampala was particularly affected by the lockdown. We investigated trends and distribution of TB case notification rates (CNR) and treatment success rates (TSR) during January 2019-June 2021 to determine the effect of COVID-19 epidemic and associated lockdown.
Methods: We analysed TB case notification and treatment success data for January 2019-June 2021 from the Uganda District Health Information Software version2 (DHIS2) and disaggregated them by region. We also collected data on the COVID-19 cases and compared COVID-19 cases with the TSR, and CNR trends over the period. We computed the CNR per 100,000 population, defined as number of notified TB cases/100,000 population. TSR was defined as the proportion of patients initiated on TB treatment that successfully completed treatment or cured. We described the quarterly trends and distribution of CNR and TSR pre (January 2019-March 2020) and during COVID-19 (April 2020-June 2021). We used interrupted time series analysis to determine the significance of the trends before and during COVID-19. We defined time periods by year (2019, 2020, or 2021) and quarter (Q).
Results: The overall TB CNR between January 2019 and June 2021, was 165/100,000; TSR was 79.4%. CNR ranged from 166.2/100,000 pre COVID-19 to 164/100,000 during COVID-19. CNR declined significantly by 22% (p=0.042, CI= [-41.4, -1.1]) from January 2020 to April 2020, concurrent with the lockdown and rising COVID-19 cases and was primarily driven by the sharp decline from 426/100,000 to 265/100,000 in Kampala City. This was followed by a significant quarterly increase in the national CNR of 16/100,000 (p<0.001, CI= [10.0,21.6]), and 39/100,000 (p=0.01, CI= [15.66,62.32]) in Kampala. TSR increased significantly by 1.6% (p<0.0001,95%CI 1.3-1.9%) quarterly.
Conclusion: CNR appeared to be affected by the initial lockdown but recovered quickly. However, this decline was heavily driven by declines in CNR in Kampala District. Kampala CNR trends are not reflective of the rest of the country during 2019-2021 and should be examined separately. TSR increased over time but was still below the 90% target. There is need to focus on continuity of TB care interventions in future in areas heavily affected by lockdowns.
Background
Both tuberculosis (TB) and COVID-19 were declared pandemics by the World Health Organisation (WHO) and currently have sustained community transmission globally (1). Before COVID-19 pandemic, TB was the leading cause of death from an infectious disease globally (2). While COVID-19 caused over 3 million deaths in a little over one year in 2020, TB caused 1.4 million deaths out of approximately 10 million new cases reported annually (3-5). However, the epidemiological interaction between TB and COVID 19 are still complex and unclear (6, 7). In response to the pandemic, policies such as lockdowns and reassignment of health infrastructure, staff, finances, and equipment such as the TB diagnostic GeneXpert machines have been widely adopted to contain the pandemic. These policies greatly affected access to and delivery of essential TB services in 2020 (6, 8, 9). According to data reported by WHO from 84 countries, there was a 21% reduction in TB case notification from 6.3 million cases in 2019 before the pandemic to about 4.9 million cases in 2020 in the 10 high burden TB countries including Uganda (9) The WHO modelling and analysis of the impact of reductions in the performance of TB detection and care on the TB mortality showed that an estimated 1.4 million additional TB deaths may occur between 2020-2025 as a direct consequence of the COVID-19 pandemic (8-10).
On the 21st of March 2020, Uganda, one of the 30 high burden TB and TB/HIV countries (11) confirmed her first COVID-19 case. By late June 2021, the country had recorded nearly 80,000 cases and 1,725 deaths (12). Following the confirmation of the first case, Uganda closed its borders except for cargo and goods transported by trucks. This was followed by suspension of public transport and restrictions on private transport on the 25th of March 2021, and nationwide curfew from 7pm to 6:30am on the 30th of March 2020. Additionality, TB diagnostic equipment such as GeneXpert machines were moved from their respective health facilities to COVID-19 diagnostic units, while some MDR TB units were re-purposed to serve as COVID-19 isolation and treatment units. These reassignments, coupled with restrictions in movement, and psychological fear of contracting the disease in health care facilities were feared to have compromised diagnostic treatment of TB as well as TB and COVID-19 coinfections, hindering the Uganda National TB and Leprosy Program’s efforts for TB control in the country (1, 6, 13).
Due to the pressure and demand that COVID-19 put on the health systems, people with TB were likely to face limited access to diagnostic and treatment services, which may have consequently resulted in adverse outcomes (1). Additionally, both COVID-19 and TB are associated with considerable social impacts such as stigma, isolation, and discrimination (5, 6, 14, 15). Seeking health care had been deferred because of social distancing measures, as well as community fears that health facilities may be infected and therefore risky (1). Although anecdotal reports suggested that these restrictions and changes may have had serious effects on health service seeking and delivery, there were limited data on its effect on TB services including TB case notification and treatment outcomes in Uganda. We analysed the nationwide TB surveillance data for the period of January 2019 to June 2021 (5 quarters before and 5 quarters during the COVID-19), to assess the indirect effect of COVID-19 on TB case notifications and treatment outcomes in Uganda.
Methods
Study setting
We conducted a cross-sectional study using TB surveillance data reported by all TB diagnostic units in all districts in Uganda. We calculated and assessed the TB Case Notification Rates (CNR), TB Treatment Success Rates (TSR), and number of COVID-19 cases at both national and regional level.
Uganda has 135 districts and 11 cities distributed across the 15 different regions in Uganda. The 15 regions include; Acholi, Ankole, Bugisu, Bukedi, Bunyoro, Busoga, Kampala, Karamoja, Kigezi, Lango, North Central, South Central, Teso, Toro, and West Nile.
Study design, data source, and description of the tuberculosis surveillance system
We performed a descriptive analysis of routinely collected surveillance data on TB obtained from the electronic District Health Information Software version 2 (DHIS2) from January 2019 to June 2021 in Uganda and calculated TB CNR and TSR for the pre-COVID-19 (January 2019-March 2020) and after COVID-19 (April 2020-June 2021) periods. The DHIS2 is an open source, web based software platform for data collection, management, and analysis (16, 17). The DHIS2 was released in 2006 and adopted in Uganda in January 2011 at the National level, before it was rolled out throughout the country in July 2012 (18). Data on the diagnosed TB patients is entered into the different registers at the health facilities. These include the laboratory registers (TB, Presumptive TB, and Unit TB). This data is then summarised into the weekly HMIS Form 033 every end of week, the monthly HMIS 105 form, and the quarterly HMIS 106 report. The weekly, monthly, and quarterly reports are submitted to the biostatistician for entry into the DHIS2, which is accessed by the Ministry of Health (MoH).
Study variables, data abstraction, analysis
We extracted data from DHIS2, which was obtained from the HMIS Form 106 (19). The HMIS Form 106 is a report on outpatient department (OPD) attendances, diagnoses, maternal and child health (MCH), HIV/AIDS, laboratory, stock status of essential drugs and supplies, and finances among others (19), which is completed and submitted to the MoH through DHIS2 at the end of every quarter. We extracted data on the treatment success rate and number of TB cases notified, expected TB cases, and percentage TB cases by sex for the pre and during COVID-19 period. We defined the CNR as the number of cases per 100,000 population, and TSR as the proportion of patients initiated on TB treatment that successfully completed treatment or cured. We used the expected TB cases and incident TB cases to calculate the proportion of expected TB cases notified and obtained the line list of monthly COVID-19 cases reported at both national and regional level.
We extracted data from the DHIS2 and exported into Microsoft Excel for cleaning and imported into Epi-info version 7.2.4 for analysis. Data on the quarterly expected TB cases, incident TB cases, percentage of notified TB cases by sex, proportion of expected TB cases notified, the CNR and TSR were summarised in tables. We computed CNR and TSR and presented them in line graphs to show the national and quarterly trends in TB CNR and TSR in Uganda before and during the COVID-19 pandemic. The treatment outcomes were classified according to the National TB control guidelines as adopted from the WHO guidelines for TB diagnosis and case definition (20). We constructed logistic regression models to examine the trends and assess the significance of these trends.
We used interrupted single group time-series analysis (ITSA) with segmented regression analysis (21, 22) to evaluate the effect of COVID-19 on the quarterly CNRs in Uganda. We estimated and presented the coefficients of ordinary least-squares (OLS) regression and produced Newey–West standard errors to handle the autocorrelation and possible heteroscedasticity (22). A p-value less than 0.05 was considered as statistically significant for all analyses.
We considered the April-June 2020 as the period in which the intervention started because the first case of COVID-19 and initial lockdown were declared in the last weeks of the January-March 2020 quarter, which may not have had a noticeable impact.
Results
National trends of case notification rates for all tuberculosis cases and all forms per 100 000 population, January 2019-June 2021
Generally, there was a fluctuating trend in the national TB case notification rates between January 2019-June 2021. However, there was a 22% decline in the April-June 2020 quarter, where the CNR decreased from 161/100,000 in January -March 2020 quarter to 133/100,000 in April 2020 quarter (Table 1). A total of 164,427 incident (new and relapse) TB cases were notified during January 2019-June 2021, with an average quarterly notification rate of 165/100,000 population. Half (82,320) of the total incident cases were reported in each of the COVID19 periods. The highest quarterly notification rate was 190/100,000 in the quarter of April-June 2021 in the later quarters of the COVID-19 pandemic, while the lowest was 133/100,000 in quarter of April 2020, in the first quarter of COVID-19 and lockdown declaration. About two thirds (79.9%) of the expected TB cases were notified pre-COVID-19 while 79.4% was notified during the COVID-19 pandemic. Consistent with the lowest CNR (133/100,000) and first quarter of COVID-19 and lockdown declaration in Uganda, the quarter of April 2020 had the lowest number of incident TB cases notified (12,871), which was only 61.6% of the expected TB 20,896 cases in the same quarter. TB cases notified between January 2019-June 2021 were majorly males (62%), which was almost twice as high as the females. This was consistent in all quarters pre and during COVID-19 period (Table 1).
Table 1:Quarterly Expected and Incident TB Cases, proportion of expected TB cases notified, proportion of notified cases by sex, Case Notification rates and Treatment success rates in Uganda, January 2019-June 2021
| Period | Estimated | Incident | % Notified of expected Incident TB cases | % Male | % Female |
CNR/100,000 |
% TSR |
| Jan-19 | 20154 | 16746 | 83.1 | 62.0 | 37.6 | 169 | 71.9 |
| Apr-19 | 20154 | 16127 | 80.0 | 62.0 | 37.6 | 161 | 73.8 |
| Jul-19 | 20896 | 18099 | 86.6 | 62.0 | 37.6 | 188 | 74.7 |
| Oct-19 | 20896 | 14948 | 71.5 | 62.1 | 37.9 | 152 | 75.8 |
| Jan-20 | 20896 | 16400 | 78.5 | 64.1 | 35.9 | 161 | 79.3 |
| Apr-20 | 20896 | 12871 | 61.6 | 63.5 | 36.5 | 133 | 81.1 |
| Jul-20 | 20585 | 15801 | 76.8 | 62.2 | 37.8 | 159 | 83.2 |
| Oct-20 | 20585 | 15819 | 76.8 | 63.0 | 37.0 | 160 | 83.6 |
| Jan-21 | 20585 | 18238 | 88.6 | 61.4 | 38.4 | 178 | 85.2 |
| Apr-21 | 20585 | 19217 | 93.4 | 60.5 | 39.7 | 190 | 85.3 |
| Average | 20623 | 16427 | 79.7 | 62.0 | 38.0 | 165.1 | 79.0 |
Interrupted time series regression analysis of the national trends of TB case notification rates in Uganda, January 2019–June 2021
The CNR at the beginning of the observation period pre-COVID-19 was at 171.2 cases per 100,000. There was a decrease in the CNR of 2.5 cases/100,000 (p=0.270, CI = [-7.5, 2.5]) per quarter pre-COVID-19, although this decline was not statistically significant. In the immediate quarter (April-June 2020) after the declaration of COVID-19 and lockdown, there was a statistically significant decline of 21.3 cases/100,000 (p<0.042, CI = [-41.5, -1.1]) in the national CNR. This was followed by a statistically significant sustained quarterly increase of 15.8 cases/100,000 (p<0.001, CI = [10.0, 21.6]) in national TB CNR in the subsequent quarters during COVID-19 (Table 2).
Table 2: Interrupted Time Series Analysis for Impact of COVID-19 on the National, Kampala and Outside Kampala quarterly TB Case notification rates, January 2019-June 2021
| Parameter | Coefficient | 95% CI | p value | |
| National | ||||
| Intercept β0 | 171.2 | [156.8 -185.6] | <0.0005 | |
| Baseline trend β1 | -2.5 | [-7.5 2.5] | 0.270 | |
| Level change after intervention β2 | -21.3 | [-41.5 -1.1] ** | 0.042 | |
| Trend change after cap β3 | 15.8 | [10.0 21.6] *** | 0.001 | |
| Kampala | ||||
| Intercept β0 | 504.4 | [485.9 522.9] *** | <0.0005 | |
| Baseline trend β1 | -24.90 | [-38.3 -11.5] *** | 0.004 | |
| Level change after intervention β2 | -77.70 | [-182.5 27.2] | 0.120 | |
| Trend change after cap β3 | 39 | [15.7 62.3] *** | 0.006 | |
| Elsewhere/outside Kampala | ||||
| Intercept β0 | 168.3 | [153.8 182.8] *** | <0.0005 | |
| Baseline trend β1 | -2.31 | [-7.3 2.7] | 0.306 | |
| Level change after intervention β2 | -20.48 | [-40.6 -0.3] ** | 0.047 | |
| Trend change after cap β3 | 15.46 | [9.6 21.3] *** | 0.001 | |
*Significant association at *** p<0.01, ** p<0.05, * p<0.1
Trends of TB case notification rates at national level and Kampala, January 2019–June 2021
At the start of the observation period pre-COVID-19, there was an estimated CNR of 171.2 cases per 100,000 at the national level, 168.3 cases/100,000 for other districts outside Kampala, and 504.4 cases/100,000 in Kampala. The CNR appeared to decrease slightly every quarter prior to COVID-19 and lockdown declaration. However, the decrease in trend of CNR was only significant in Kampala. For each quarter, the CNR significantly decreased by 24.90 cases/100,000 per quarter in Kampala. Although there was a decreasing trend in CNR at the National level of 2.5 cases/100,000(p=0.270, CI= [-7.5-2.5] and 2.31 cases/100,000 (p=0.306 CI= [-7.3- 2.7]) per quarter elsewhere outside Kampala, this decrease was not significant. In the first quarter of the COVID-19 and lockdown declaration, there appeared to be a statistically significant decrease in quarterly CNR of 21.30 cases/100,000 (p<0.05, 95% CI = [-41.5, -1.1]) at national level and 20.48 cases/100,000 (p<0.05, 95%CI = [-40.7, -0.31]) in other districts outside Kampala. However, despite the 77.70 cases/100,000 (p=0.120, 95%CI= [-182.5 27.2]) decrease in CNR, the decrease was not statistically significant in Kampala. This was followed by a statistically significant increase in CNR of 39 cases/100,000 (p<0.01, 95% CI = [15.66, 62.34]) in Kampala, 15.46 cases/100,000 (p<0.01, 95% CI = [9.66, 21.26]) outside Kampala and 15.80 cases/100,000 (p<0.01,95% CI = [10.04, 21.56]) at the National level per quarter in the subsequent quarters during COVID-19. (Table 2).
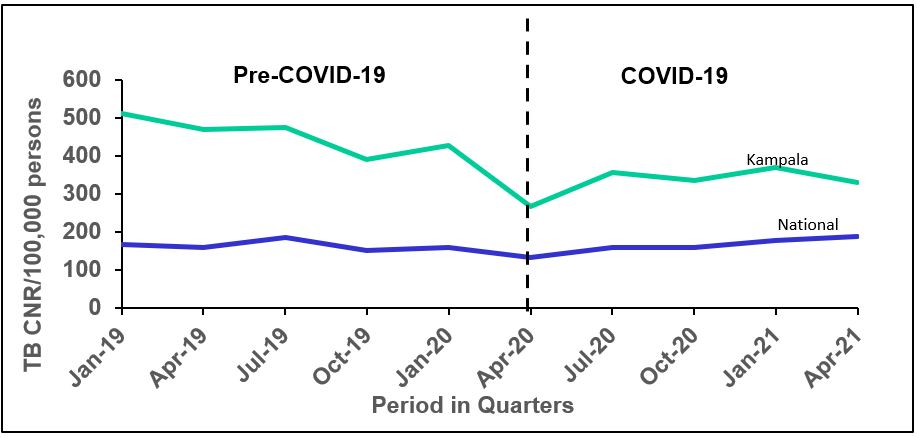
Trends of TB case notification rates by region before and during the COVID-19 pandemic
Generally, there was no noticeable change in TB CNR at national level throughout the study period, pre and during COVID-19. However, the regional trends showed a 27.5% decline in TB CNR in Kampala, and a 10.8 increase in TB CNR in Karamoja during the COVID-19 pandemic.
Interrupted time series regression analysis of the regional trends of TB case notification rates in Uganda, January 2019–June 2021
There was a general decline in TB CNR in quarters pre and immediately after the COVID-19 outbreak declaration across all regions in Uganda, while there was a general increase in the subsequent quarters during the COVID-19 pandemic in majority of the regions. However, CNR were generally consistent in Karamoja, Lango, Teso, and West Nile regions throughout the study period both pre and during COVID-19 (Table 3).
Majority of the regions in Uganda experienced a decline in the TB case notification rates before the emergence of the COVID-19 pandemic and related lockdowns. However, these declines were not statistically significant in majority of the regions except for Acholi, Kampala, and Kigezi regions. The TB CNR at the start of the observation period was 255 cases/100,000 (CI = [211.4–298.3]) in Acholi, 504 cases/100,000(CI = [485.9 522.9]) in Kampala, and 158 cases/100,000 in Kigezi (CI= [140.5–174.7]). There was a statistically significant decrease in CNR every quarter pre-COVID-19, decreasing quarterly by 21.7 cases/100,000 (p=0.010, CI = [-36.1-7.3]) in Acholi, 24.9 cases/100,000(p=0.004, CI = [-38.3-11.5]) in Kampala and 11.6 cases/100,000 (p=0.005, CI = [-18.2- -5.0]) in Kigezi region (Table 3).
In the immediate quarters after the COVID-19 pandemic there was a statistically significant quarterly decline of 26 cases/100,000 (p=0.038, CI = [-49.1–1.9]) in Ankole and 59 cases/100,000 (p=0.001, CI = [-84.9-33.7]) in North Central region. The remaining 12 regions experienced declines in the CNR every quarter during the early quarters of COVID-19 but these were not statistically significant. Contrary to the 14 regions that experienced declines in quarterly CNR, Acholi experienced an increase in CNR by 39 cases/100,000 (p=0.145, CI = [-18.2-96.9]), although this increase was not statistically significant (Table 3).
Unlike the immediate quarters following outbreak of COVID-19 in Uganda where majority of the regions experienced a decline in CNR, there was a sustained general increase in CNR across the different regions in Uganda in the subsequent months after the COVID-19 and lockdown declaration, except Karamoja which had a 4.2 cases/100,000 (p=0.828, CI = [-49.4 – 41.0]) non-statistically significant decline in the CNR per quarter. In the majority of the regions (11/15), the increase in CNR was statistically significant while there was no significant change in Lango, Teso, and West Nile. The CNR significantly increased per quarter by 26 cases/100,000 (p=0.012, CI = [8.2 – 43.8]) in Acholi, 14 cases/100,000(p=0.001, CI = [8.2 – 20.4]) in Ankole, 5 cases/100,000 (p=0.012, CI = [1.6 – 8.7]) in Bugisu, 15cases/100,000(p=0.032, CI = [1.7 – 27.2]) in Bukedi, 17cases/100,000 (p=0.031, CI = [2.2 – 32.6]) in Bunyoro, 12 cases/100,000 (p=0.008, CI = [4.4 – 19.5]) in Busoga, 39 cases/100,000(p=0.006, CI = [15.7 – 62.3]) in Kampala, 22 cases/100,000 (p=0.001, CI = [13.3 – 30.2]) in Kigezi, 20cases/100,000 (p=0.003, CI = [9.6 – 30.8]) in North Central, 29 cases/100,000(p<0.001, CI = [18.6 – 38.9]) in South Central, and 27cases/100,000 (p=0.004, CI = [12.3 – 42.3]) in Toro (Table 3).
Table 3: Interrupted time series regression analysis for the impact of COVID-19 on the regional trends of TB Case Notification rates in Uganda, January 2019-June 2021
| Parameter | Coefficient | 95% CI | p value | |
| Acholi Region | ||||
| Intercept β0 | 254.9 | 211.4–298.3 | <0.0005 | |
| Baseline trend β1 | -21.7 | -36.1 -7.3 | 0.010 | |
| Level change after intervention β2 | 39.4 | -18.2–96.9 | 0.145 | |
| Trend change after cap β3 | 26.0 | 8.2 – 43.8 | **0.012 | |
| Ankole | ||||
| Intercept β0 | 119.3 | 112.0–126.6 | <0.0005 | |
| Baseline trend β1 | -2.4 | -7.7– 2.9 | 0.314 | |
| Level change after intervention β2 | -25.5 | -49.1–1.9 | 0.038 | |
| Trend change after cap β3 | 14.3 | 8.2–20.4 | 0.001 | |
| Bugisu | ||||
| Intercept β0 | 98.6 | 91.9–105.2 | <0.0005 | |
| Baseline trend β1 | 2.7 | -1.4–6.8 | 0.156 | |
| Level change after intervention β2 | -18.7 | -38.6–1.2 | 0.061 | |
| Trend change after cap β3 | 5.1 | 1.6–8.7 | 0.012 | |
| Bukedi | ||||
| Intercept β0 | 69.7 | 36.4–102.9 | 0.002 | |
| Baseline trend β1 | -3.2 | -14.6-8.2 | 0.522 | |
| Level change after intervention β2 | -3.9 | -37.5–29.7 | 0.79 | |
| Trend change after cap β3 | 14.5 | 1.7–27.2 | 0.032 | |
| Bunyoro | ||||
| Intercept β0 | 169.4 | 151.2–187.5 | <0.0001 | |
| Baseline trend β1 | -1.9 | -8.2– 4.4 | 0.489 | |
| Level change after intervention β2 | -48.1 | -99.2–3.0 | 0.061 | |
| Trend change after cap β3 | 17.4 | 2.2–32.6 | 0.031 | |
| Busoga | ||||
| Intercept β0 | 105.5 | 95.4–115.6 | <0.0001 | |
| Baseline trend β1 | -0.3 | -4.3– -3.7 | 0.859 | |
| Level change after intervention β2 | -14.9 | -32.3–2.5 | 0.081 | |
| Trend change after cap β3 | 11.9 | 4.4-19.5 | 0.008 | |
| Kampala | ||||
| Intercept β0 | 504.4 | 485.9–522.9*** | <0.0001 | |
| Baseline trend β1 | -24.90 | -38.3 -11.5 *** | 0.004 | |
| Level change after intervention β2 | -77.70 | -182.5–27.2 | 0.120 | |
| Trend change after cap β3 | 39 | 15.7–62.3 *** | 0.006 | |
| Karamoja | ||||
| Intercept β0 | 318.3 | 261.5–375.1 | <0.0001 | |
| Baseline trend β1 | 11.6 | -8.7–31.9 | 0.211 | |
| Level change after intervention β2 | -11.9 | -123.3–99.5 | 0.803 | |
| Trend change after cap β3 | -4.2 | -49.4–41.0 | 0.828 | |
| Kigezi | ||||
| Intercept β0 | 157.6 | 140.5–174.7 | <0.0001 | |
| Baseline trend β1 | -11.6 | -18.2– -5.0 | 0.005 | |
| Level change after intervention β2 | -19.2 | -43.3–4.9 | 0.099 | |
| Trend change after cap β3 | 21.8 | 13.3–30.2 | 0.001 | |
| Lango | ||||
| Intercept β0 | 242.4 | 188.6–296.2 | <0.0001 | |
| Baseline trend β1 | -6.2 | -25.1–12.6 | 0.450 | |
| Level change after intervention β2 | -14.9 | -82.1–52.2 | 0.606 | |
| Trend change after cap β3 | 18.7 | -5.0–42.4 | 0.101 | |
|
North Central |
||||
| Intercept β0 | 160.1 | 151.2–168.9 | <0.0001 | |
| Baseline trend β1 | 1.8 | -1.7–5.4 | 0.245 | |
| Level change after intervention β2 | -59.3 | -84.9–33.7 | 0.001 | |
| Trend change after cap β3 | 20.2 | 9.6–30.8 | 0.003 | |
| South Central | ||||
| Intercept β0 | 233.3 | 210.2–256.4 | <0.0001 | |
| Baseline trend β1 | -6.5 | -15.3–2.3 | 0.122 | |
| Level change after intervention β2 | -23.1 | -53.9–7.7 | 0.116 | |
| Trend change after cap β3 | 28.7 | 18.6–38.9 | <0.0001 | |
| Teso | ||||
| Intercept β0 | 92.4 | 70.6–114.2 | <0.0001 | |
| Baseline trend β1 | -1.3 | -9.3–6.7 | 0.707 | |
| Level change after intervention β2 | -23.2 | -57.9–11.6 | 0.155 | |
| Trend change after cap β3 | 9.6 | -2.9-22.1 | 0.109 | |
| Toro | ||||
| Intercept β0 | 155.0 | 138.5–171.5 | <0.0001 | |
| Baseline trend β1 | -5.4 | -14.4–3.7 | 0.199 | |
| Level change after intervention β2 | -15.0 | -47.3–17.2 | 0.298 | |
| West Nile | ||||
| Intercept β0 | 166.0 | 108.1–223.8 | <0.0001 | |
| Baseline trend β1 | 6.7 | -13.7–26.9 | 0.459 | |
| Level change after intervention β2 | -22.5 | -82.7–37.8 | 0.397 | |
| Trend change after cap β3 | 2.9 | -23.9–29.8 | 0.798 | |
*Significant association at p<0.05 **Marginally significant association at p≥0.05<0.1
Trends of the treatment success rate in Uganda, January 2019-June 2021
Generally, there was a steady increase in the TSR between January 2019-June 2021, which may imply that COVID-19 had no impact on the treatment outcomes (Figure 3). The average TSR was 79% between January 2019-June 2021 (Table 1). Contrary to the CNR where we saw a decline, there was a 1.8% increase in TSR from 79.3% in the quarter of January 2020 to 81.1% in the quarter of April 2020 when the movement restriction was instituted in Uganda.
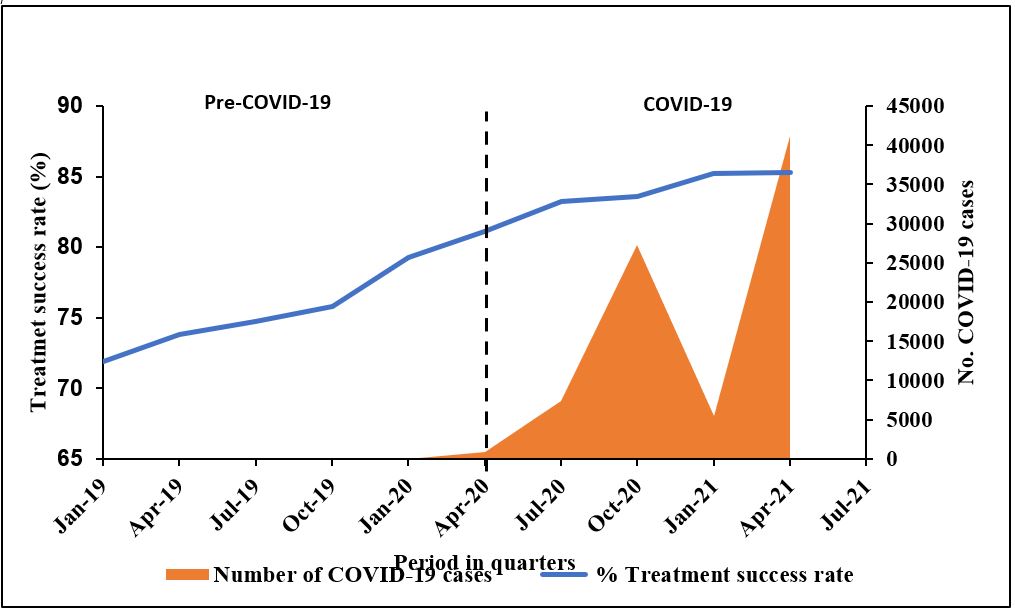
Interrupted time series analysis of effect of COVID-19 on treatment success rate
There was a general increase in the national TSR between January 2019 to June 2021. The TSR at the start of the observation period was 71.74% (p=CI= [70.91-72.57]). There was a statistically significant 1.68 percentage (p<0.0001, CI= [1.18-2.18]) increase in TSR per quarter before the COVID-19 outbreak in Uganda. In the quarter of April -June 2020 when the movement restrictions were put in place, there was a non-statistically significant 1.46 (p=0.225, CI= [-1.18-4.10]) percentage increase in TSR per quarter. This was followed by a statistically significant sustained decline in the TSR where we found a 0.64 percentage quarterly decrease (p=0.016, CI= [-1.11-0.17]). (Table 4)
Table 4: Interrupted Time Series Analysis for Impact of COVID-19 on TB treatment success rate in Uganda, January 2019-June 2021
| TSR | Coeff | SE | t | p>|t| | [95% CI] |
| Time | 1.68***
|
0.204 | 8.22 | 0.000 | [1.18 2.18] |
| Intervention | 1.46
|
1.079 | 1.35 | 0.225 | [-1.18 4.10] |
| Time since intervention | -0.64**
|
0.192 | -3.33 | 0.016 | [-1.11 -0.17] |
| Intercept | 71.74*** | 0.340 | 210.98 | 0.000 | [70.91 72.57] |
Discussion
COVID-19 has not only led to the loss of millions of human lives but also affected delivery of health services directly or indirectly across the globe (7, 23). We analysed the quarterly trends of TB case notification rates and treatment success rates before and after the COVID-19 pandemic in Uganda from January 2019- June 2021.
In this study, there was a general decline in the national CNRs and a steady increase in TSR in Uganda between January 2019-June 2021. The study showed that fewer cases were notified during the pandemic than the reported number of cases in the absence of the pandemic. The decline in TB CNRs wasin the first quarter of the COVID-19 pandemic and lockdown in Uganda. These findings are consistent with studies from the United States, Malawi, Taiwan, Korea, and Ethiopia (24-28). However, we found that after the initial decline immediately after the declaration of the COVID-19 pandemic and related movement restrictions, the TB CNRs gradually increased through the subsequent quarters between April 2020-June 2021. Despite the increase in TB cases notified in the last quarters of the COVID-19 pandemic, the CNRs and overall number of TB cases reported was lower during the COVID-19 period compared with the pre-COVID-19 period. This is also consistent with findings from Spain, Malawi and 9 other countries (10, 23, 28).
Although the incidence of TB in Uganda has decreased steadily over the years (4, 29), a 22% decrease in TB CNRs in the immediate quarter after declaration of the COVID-19 pandemic and lockdown measures is larger than predicted by the ITSA model. This could be attributed to different factors. First, the decline in TB CNR may be due to reduced transmission associated with the wide use of face masks, social distancing and restrictions in movement(6, 7, 25, 30). Studies have shown a 10% reduction in TB transmission in high burden TB countries due to social distancing and use of masks (10). However, the 22% immediate decline in the TB CNR in Uganda may also suggest additional factors such as interruption in TB contact tracing and preventive therapy. It could also be due to poor access to TB care services due to movement restrictions and rechannelling of health facility resources from TB care to COVID-19 treatment. This agrees with a study in the United States that showed an overall decline
Further analysis of the regional CNRs shows that although the pre-COVID-19 decline was not statistically significant at the national level and the other 12 regions, it was statistically
significant in Acholi, Kampala, and Kigezi regions. Contrary to the pre-COVID decline, we found a statistically significant decline in the national CNR in the first quarter of the COVID-19 and lockdown declarations in Uganda. However, a deep dive into the data shows that this decline was only statistically significant in the Ankole and North central regions. Contrary to the baseline period and the period immediately after the declaration of COVID-19 outbreak and lockdown where we saw general reductions in CNR, the following quarters showed a positive and sustained increase in CNRs across all regions except Karamoja which had a non-statistically significant decrease in CNR. In this period, we found a sustained increase in CNR which was statistically significant at the national level and in majority of the regions except Lango, Teso, and West Nile where the increase was not statistically significant.
We hypothesize that these variations in CNR during the observation period may be due to the uneven enforcement of COVID-19 control measures across the different regions in Uganda. Urban areas like Kampala and North Central could have had a blend of application of restrictions compared to other areas. Additionally, this could be due to some mitigation measures in other areas such as the TB emergency response in the North and Eastern regions in Uganda compared to other regions that did not have these interventions. We also hypothesize that the recovery performance from COVID-19 lockdown in the later quarters of COVID-19 pandemic and lockdown declarations were due to several innovations by the National TB and Leprosy program (NTLP) in collaboration with implementing partners in the different regions (29). The innovations included the community awareness screening and testing (CAST-TB) campaign in some regions where over 1500 missing TB cases were diagnosed and started on treatment, intensified active case finding, quality improvement collaboratives, installation of mobile digital X-ray machines for active TB case finding, and intensive private sector and media engagement among others (29).
Study Limitations
Our study had some limitations. First, we used routinely collected surveillance data with the inherent limitations of retrospective data and its potential to over or underestimate the TB cases notified depending on likelihood of data entry errors. However, being a national data set, reflects a good picture of the general trends in the TB CNRs across the country in the study period. Second, the study period was limited to a few quarters before and during the COVID-19 pandemic, thus not allowing for the assessment of the longer-term outcomes, however, these may be assessed in the later stages of the pandemic. Finally, several factors may have played a role in the decline in the TB CNRs yet our study was not in position to distinguish between the effects of COVID-19 preventive measures and the delays in disease diagnosis. However, we can comfortably note that may have several unknown consequences on TB care and outcomes based on findings from several studies globally.
Conclusion
COVID-19 had an immediate substantiated effect on TB CNR in Uganda. The effect varied across the different regions. However, the initial COVID-19 related decline in TB CNRs was not sustained as there was a quick recovery seen in the later quarters of the pandemic and lockdown.
Conflict of Interest
The authors declare that they had no competing interests.
Acknowledgments
The authors would like to thank the Ministry of Health for allowing us to access data in the DHIS2 database
References
- Wingfield T, Cuevas LE, MacPherson P, Millington KA, Squire SB. Tackling two pandemics: a plea on World Tuberculosis Day. The Lancet Respiratory Medicine. 2020;8(6):536-8.
- USAID STP. Simultaneous, integrated diagnostic testing approach to detect COVID-19 and TB in high TB burden countries 2021.
- Kitara DL, Ikoona EN. COVID-19 pandemic, Uganda’s story. The Pan African medical journal. 2020;35(Suppl 2):51.
- World Health Organization. Global Tuberculosis Report 2020. Licence: CC BY-NC-SA 3.0 IGO. Geneva: World Health Organization, 2020. 2020.
- World Health Organization. Novel Coronavirus (2019-nCoV): situation report, 11. Geneva: World Health Organization; 2020 2020-01-31.
- Behera D. TB control in India in the COVID era. The Indian journal of tuberculosis. 2021;68(1):128-33.
- Bell D, Hansen KS, Kiragga AN, Kambugu A, Kissa J, Mbonye AK. Predicting the Impact of COVID-19 and the Potential Impact of the Public Health Response on Disease Burden in Uganda. Am J Trop Med Hyg. 2020;103(3):1191-7.
- Glaziou P. Predicted impact of the COVID-19 pandemic on global tuberculosis deaths in 2020. medRxiv. 2020:2020.04.28.20079582.
- World Health Organization. Impact of the COVID-19 Pandemic on TB Detection and Mortality in 2020. 2021.
- Stop TB Partnership G. The potential impact of the covid-19 response on tuberculosis in high-burden countries: a modelling analysis 2020.
- World Health Organization. WHO releases new global lists of high-burden countries for TB, HIV-associated TB and drug-resistant TB. 2021.
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard 2021 [Available from: https://covid19.who.int/.
- Bell D, Hansen KS, Kiragga AN, Kambugu A, Kissa J, Mbonye AK. Predicting the Impact of COVID-19 and the Potential Impact of the Public Health Response on Disease Burden in Uganda. Am J Trop Med Hyg. 2020;103(3):1191-7.
- Negin J, Abimbola S, Marais BJ. Tuberculosis among older adults–time to take notice. International journal of infectious diseases: IJID : official publication of the International Society for Infectious Diseases. 2015;32:135-7.
- Wingfield T, Tovar MA, Datta S, Saunders MJ, Evans CA. Addressing social determinants to end tuberculosis. Lancet (London, England). 2018;391(10126):1129-32.
- Open Health News: The Voice for the Open Health Community. District Health Information System 2 (DHIS2) 2020 [Available from: https://www.openhealthnews.com/resources/district-health-information-system-2-dhis2.
- University of Oslo. DHIS2 In Action.
- Kiberu V, Matovu J, Makumbi F, Kyozira C, Mukooyo E, Wanyenze R. Strengthening district-based health reporting through the district health management information software system: The Ugandan experience. BMC medical informatics and decision making. 2014;14:40.
- Uganda eHMISUganda’s Electronic Health Information System: DHIS2 [Internet]. Ministry of Health. Available from: https://hmis.health.go.ug/dhis-web-commons/security/login.action.
- Stosic M, Grujicic SS, Grgurevic A, Kuruc V, Ristic L, Antonijevic G, et al. Trends in tuberculosis notification and mortality and factors associated with treatment outcomes in Serbia, 2005 to 2015. Eurosurveillance. 2020;25(1):1900322.
- Bottomley C, Scott JAG, Isham V. Analysing interrupted time series with a control. Epidemiologic Methods. 2019;8(1).
- Linden A. Conducting interrupted time-series analysis for single-and multiple-group comparisons. The Stata Journal. 2015;15(2):480-500.
- Aznar ML, Espinosa-Pereiro J, Saborit N, Jové N, Sánchez Martinez F, Pérez-Recio S, et al. Impact of the COVID-19 pandemic on tuberculosis management in Spain. International Journal of Infectious Diseases. 2021;108:300-5.
- Arega B, Negesso A, Taye B, Weldeyohhans G, Bewket B, Negussie T, et al. Impact of COVID-19 pandemic on TB prevention and care in Addis Ababa, Ethiopia: a retrospective database study. BMJ Open. 2022;12(2):e053290.
- Kwak N, Hwang SS, Yim JJ. Effect of COVID-19 on Tuberculosis Notification, South Korea. Emerging infectious diseases. 2020;26(10):2506-8.
- Lai C-C, Yu W-L. The COVID-19 pandemic and tuberculosis in Taiwan. J Infect. 2020;81(2):e159-e61.
- Lange SJ, Ritchey MD, Goodman AB, Dias T, Twentyman E, Fuld J, et al. Potential Indirect Effects of the COVID-19 Pandemic on Use of Emergency Departments for Acute Life-Threatening Conditions – United States, January-May 2020. MMWR Morbidity and mortality weekly report. 2020;69(25):795-800.
- Soko RN, Burke R, Feasey HRA, Sibande W, Nliwasa M, Henrion MYR, et al. Effects of Coronavirus Disease Pandemic on Tuberculosis Notifications, Malawi. Emerging Infectious Disease journal. 2021;27(7):1831.
- Ministry of Health. Uganda National TB and Leprosy Program Annual Performance Report 2020/2021. 2021.
- Robsky KO, Hughes S, Kityamuwesi A, Kendall EA, Kitonsa PJ, Dowdy DW, et al. Is distance associated with tuberculosis treatment outcomes? A retrospective cohort study in Kampala, Uganda. BMC Infectious Diseases. 2020;20(1):40


Comments are closed.