Assessment of Oral Pre-exposure Prophylaxis Eligibility and Use among Persons at Substantial Risk of HIV Acquisition, Uganda, 2017-2021
Authors: Sarah Elayeete1*, Gerald Pande2, Benon Kwesiga1, Daniel Kadobera1, Kabwama Stephen1, Alex Ario Riolexus Institutional affiliations 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, 2Ministry of Health, Kampala, Uganda. Correspondence*: Email: selayeete@musph.ac.ug, Tel:+256-782-948-872
Summary
Background: In 2017, Oral pre-exposure prophylaxis (PrEP) was rolled out by the Uganda Ministry of Health (MOH) for high-risk populations at substantial risk of HIV infection (HRPs). In this strategy, HIV-negative individuals are screened for oral PrEP eligibility. Eligible high-risk individuals are offered pre-PrEP counselling, and those who accept are initiated, with subsequent follow-up visits for refills. However, no study has evaluated eligibility and uptake of oral PrEP since its roll-out. We assessed for oral PrEP eligibility, use, and associated factors among HRPs, Uganda, 2017-2021.
Methods: HRPs demographics, oral PrEP eligibility, oral PrEP initiation and refill dates were retrieved from PrEP tracker system for July 2017-May 2021. We conducted descriptive analysis of all HRPs screened for oral PrEP eligibility and oral PrEP use Modified Poisson regression was applied to identify factors associated with oral PrEP eligibility and use.
Results: Overall, 7,727 HRPs were screened for oral PrEP eligibility. Out of these, 3,156 (41%) were identified oral PrEP-eligible for whom 1,900 (60%) were female and 1,392 (44%) were sex workers. Among HRPs identified as oral PrEP-eligible, 2,409 (76%) were initiated on oral PrEP. Of these, 1,513 (63%) were female, 2,136 (89%) were from Central Region, and 1,188 (49%) were sex workers. Being a male (vs. female) HRPs was associated with increased oral PrEP eligibility (IRR=1.2, 95% CI: 1.02-1.41; p=0.03). HRPs in discordant relationship (vs. sex workers) were strongly associated with increased oral PrEP eligibility (IRR=3.6, 95% CI: 2.65-4.85; p<0.0001). Being married or cohabiting (vs. single) was associated with increased oral PrEP use (IRR=1.3, 95% CI: 1.01-1.6; p=0.04). Older HRPs aged 50 years and above had a reduced rate of oral PrEP eligibility (RR=0.4, 95%CI: 0.26-0.56; P<0.0001) and oral PrEP use (RR=0.3, 95%CI: 0.17-0.67; P=0.002).
Conclusion: Despite low rate of oral PrEP eligibility among people at substantial risk of HIV infection, oral PrEP use was high. Married or cohabiting HRPs had an increased rate of oral PrEP use, suggesting a role for partner support. Intensified efforts may be needed to promote partner support to ensure oral PrEP use among HRPs.
Introduction
Oral Pre-exposure Prophylaxis (PrEP) is the use of ARV drugs by HIV-uninfected persons to prevent HIV infection and has been shown to reduce HIV transmission in both clinical trials and community-based studies (1-4) . Oral PrEP using tenofovir (TDF) and emtricitabine (FTC) as a once-daily pill is highly effective against HIV infection (5); however, the degree of effectiveness depends mainly on uptake and continuity (6). The World Health Organization (WHO) recommends the use of oral PrEP for HIV-negative persons at high risk of infection (7), including key populations (KPs) such as female sex workers (FSW), fisherfolk (FF), serodiscordant couples (SDC), men who have sex with men (MSM), and adolescent girls and young women (AGYW) (7-9).
In Kampala, HIV prevalence among MSM was estimated at 13.7% and 31.3% among FSW in 2012 (10). Other studies estimated HIV prevalence among people who inject drugs (PWID) at 34% (11). The higher prevalence of HIV infection among these populations was due to high-risk sexual behaviors (12, 13). In 2017, the Uganda Ministry of Health (MOH) rolled out oral pre-exposure prophylaxis (PrEP) for high-risk populations (5). In this strategy, HIV-negative individuals were screened for oral PrEP eligibility and eligible HRPs were offered pre-PrEP counselling and those who accept were initiated on oral PrEP (14, 15).
Although correct and consistent use of oral PrEP is effective in preventing HIV infection for high-risk population groups at substantial risk of HIV infection, important questions remain about oral PrEP use among people at substantial risk of HIV acquisition in Uganda. We assessed oral PrEP eligibility, oral PrEP use, and associated factors among high-risk populations at substantial risk of HIV infection in Uganda, 2017-2021.
Methods
Study setting, design, sample size consideration, and exclusion criteria
We conducted a secondary data analysis using the PrEP tracker dataset as of July 2017 to May 2021. Oral PrEP data from all health facilities in the US-CDC supported regions offering oral PrEP among high-risk populations at substantial risk of HIV infection during the study period were abstracted and included in the study.
The PrEP tracker is a database created to capture all oral PrEP use data in the country these include Key populations- and other priority Populations at substantial risk of HIV acquisition like AGWY, Pregnant and Breast-feeding mothers. The database provides insights in the client’s baseline and follow-up data including: numbers of oral PrEP users, demographic characteristics, oral PrEP eligibility screening data, dates of follow-up, oral PrEP eligibility, initiation dates, HIV screening, reasons for declining oral PrEP and enrolment dates.
Oral PrEP data are routinely generated at health facility level using clients’ registers and then uploaded into the tracker (web-based reporting). The PrEP tracking system is designed to collect monthly and quarterly data that are nationally representative of oral PrEP use across health facilities offering oral PrEP services to people at substantial risk of HIV. Oral PrEP was rolled out in 142 sites in June 2017 and we included all participants data from the start of the program up to May, 2021. We excluded all participants with missing information on oral PrEP eligibility and oral PrEP use during the study period.
Study variables, data abstraction, and analysis
We abstracted HRPs demographic data, including (sex, age, marital status, region of origin), key populations classification category (sex workers, clients of sex workers, men who have sex with men, people who inject drugs, transgender people), and priority populations category (migrant workers, fish folks, uni-formed men, discordant couples, adolescent girls and young women, truckers, people in prison and displaced persons)), HRPs oral PrEP eligibility, initiation and refill dates.
We conducted descriptive analysis of HRPs demographic characteristics using frequencies and percentages. HRPs at substantial risk of HIV infection were categorized as: “eligible or not eligible” and “oral PrEP users or non- oral PrEP users.” “oral PrEP eligibility” was the percentage of HRPs meeting oral PrEP use criteria of the total screened at baseline for the study period (July, 2017-May, 2021). “oral PrEP use”-the percentage of HRPs initiated on oral PrEP at baseline of the total HRPs identified eligible. “oral PrEP non-use”- the proportion of HRPs who declined using oral PrEP of all those identified as oral PrEP-eligible.
To identify factors associated with oral PrEP eligibility and oral PrEP use among HRPs at baseline, modified Poisson regression was applied to estimate incident rate ratios (IRRs) and 95% confidence intervals of oral PrEP eligibility and use by HRPs baseline characteristics. All factors at bivariate analysis were included in the multivariate model and statistical significance was set at P ≤ 0.05. All data analysis was done using Stata version 14.0.
Ethical considerations
We used KPs PrEP surveillance data with no identifying information We obtained oral PrEP data with permission from Makerere University School of Public Health Monitoring and Evaluation Technical Support Program (METs) who are currently custodians of HRPs oral PrEP data together with Ministry of Health (MOH). In addition, the Office of the Associate Director for Science, U.S. Centers for Disease Control and Prevention, determined this project as a non- human subject’s research that is in response to a public health problem with the primary intent of public health practice (epidemic disease control).
Result
Social-demographic characteristics of high-risk populations screened for oral PrEP eligibility and oral PrEP use at baseline in Uganda, 2017-2020
A total of 7,727 high risk populations (HRPs) were screened for oral PrEP eligibility at baseline. Of these, 3,156 (41%) were identified eligible for oral PrEP use. The majority 1,900 (60%) were female with a median age of 25 years (range: 10, 75 years). A high proportion of oral PrEP-eligible HRPs were from central region 2,821 (89%), and 1,392 (44%) were sex workers (Table 1).
Among HRPs identified eligible for oral PrEP, 2,409 (76%) were initiated on oral PrEP at baseline. Out of those, 1,513; (63%) were female, most HRPs 1,127 (47%) were single, the majority 2,136 (89%) were from central region and 1,188 (49%) were sex workers (Table 1).
Table 1: Socio-demographic characteristics of high-risk populations screened for oral PrEP eligibility and oral PrEP use at baseline, Uganda, 2017-2021
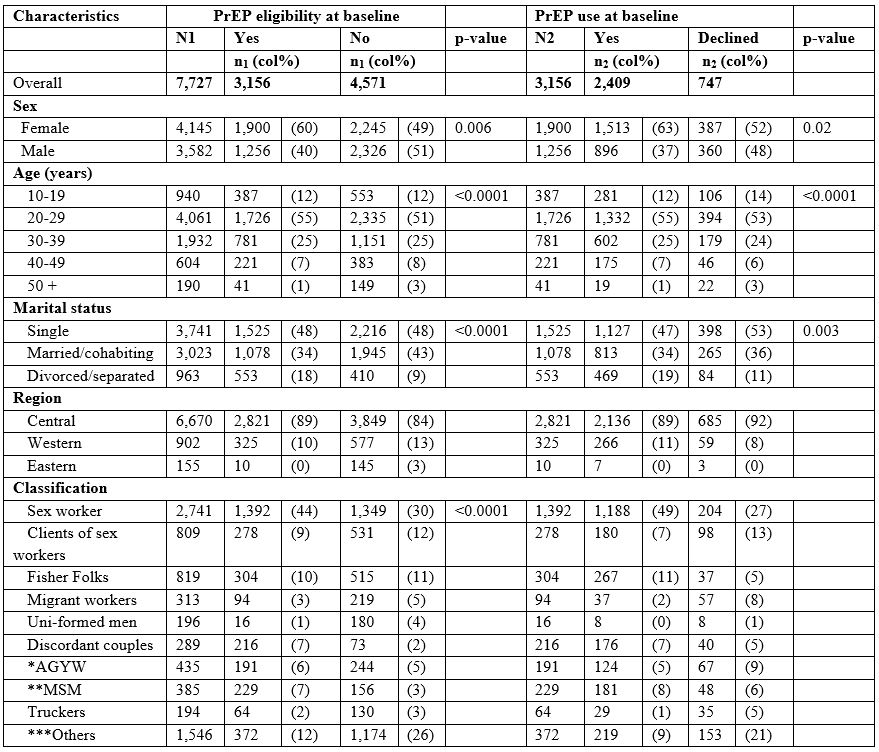
- N1– Overall total of those screened for PrEP eligibility
- §N2–The proportion of those identified eligible for PrEP use at baseline
*AGYW=Adolescent girls and young women
**MSM=Men who have sex with men
***Others include= people who inject drugs, people in prison, transgender, None, non-injecting drug users, and displaced persons
Factors associated with oral PrEP eligibility among high risk populations screened at baseline, Uganda, 2017-2021
Male HRPs were strongly associated with increased oral PrEP eligibility compared with their female counter parts (IRR=1.2, 95% CI: 1.02-1.41; P=0.03) (Table 2). Being divorced or separated compared with being single was associated with increased oral PrEP eligibility (IRR=2.0, 95% CI: 1.67-2.29; P=<0.0001). HRPs from Eastern verses central region were associated with 30% reduced rate of oral PrEP eligibility (P=<0.0001). HRPs in discordant relationships were strongly associated with increased PrEP eligibility compared with sex workers (IRR=3.6, 95% CI: 2.65-4.85; P=<0.0001) (Table 2).
Table 2: Factors associated with Oral PrEP eligibility among high-risk populations at substantial risk of HIV infection screened at baseline, Uganda, 2017-2021
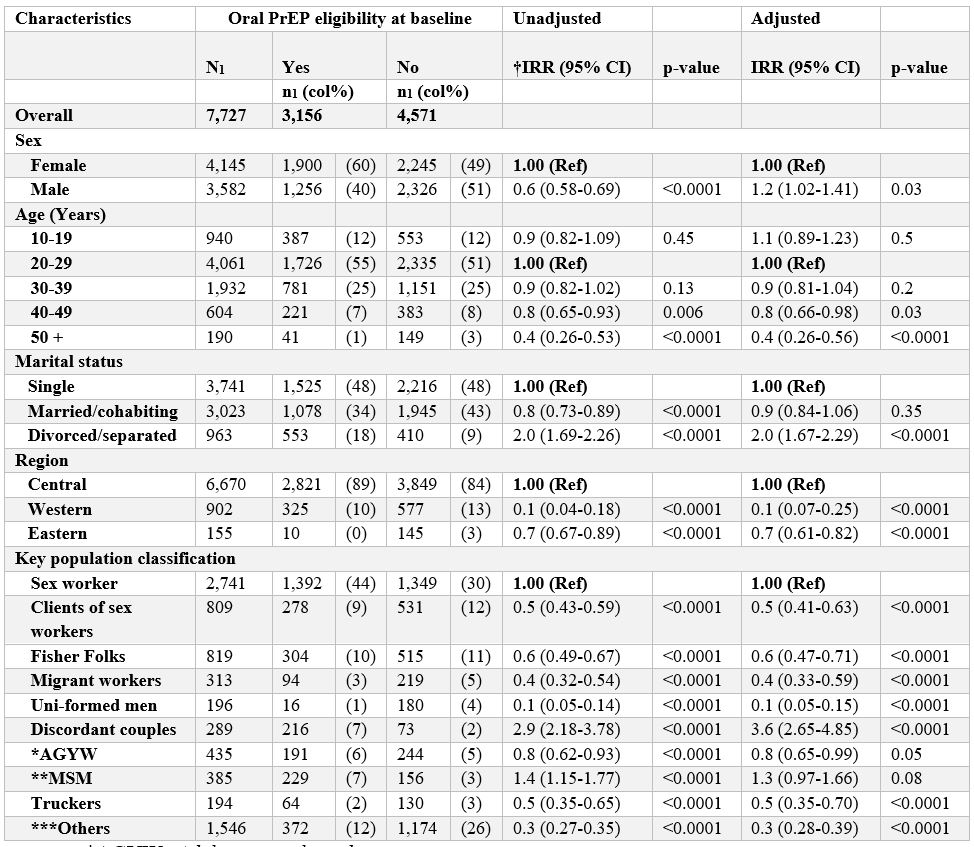
*AGYW=Adolescent girls and young women
**MSM=Men who have sex with men
***Others= people who inject drugs, people in prison, transgender, None, non-injecting drug users, and displaced persons
†IRR=Incidence rate ratio
Factors associated with oral PrEP use among eligible high-risk populations at substantial risk of HIV infection at baseline in Uganda, 2017-2021
Male HRPs were strongly associated with increased oral PrEP use compared with female HRPs (IRR=1.7, 95% CI: 1.27-2.36; P=0.001) (Table 3). HRPs at substantial risk of HIV infection aged 50 years and older were associated with 70% reduced rate of using oral PrEP at baseline compared with younger HRPs aged 20-29 years (p=0.002). Being married or cohabiting was significantly associated with increased oral PrEP use compared with being single (IRR=1.3, 95% CI: 1.01-1.58; P=0.04). Divorced or separated HRPs were strongly associated with increased oral PrEP use (IRR=1.7, 95% CI: 1.24-2.22; p=0.001). HRPs from Eastern verses central region were strongly associated with increased oral PrEP use (IRR=1.8, 95% CI: 1.33-2.56; P=<0.0001) (Table 3).
Table 3: Factors associated with oral PrEP use among eligible high-risk populations at substantial risk of HIV infection at baseline, Uganda, 2017-2021
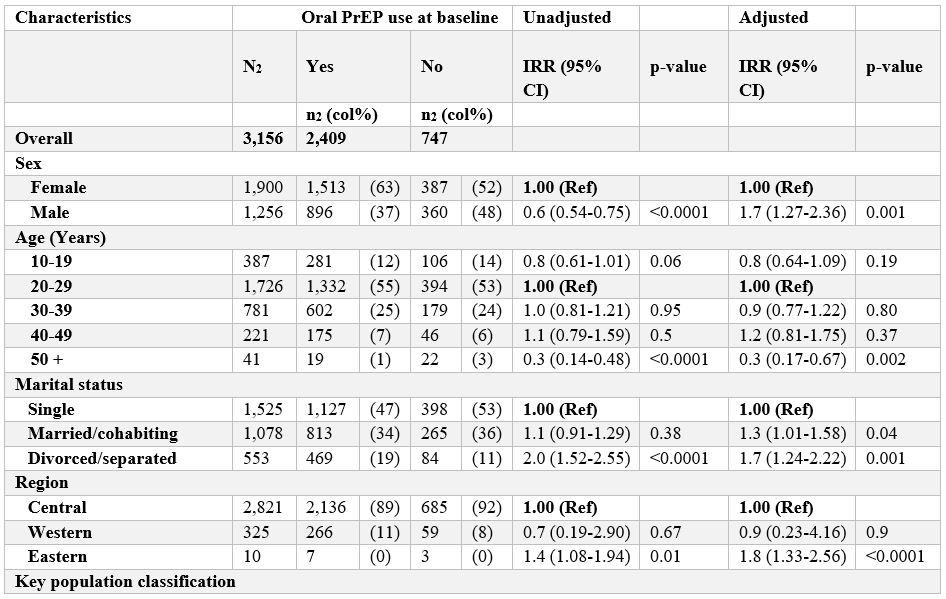
*AGYW=Adolescent girls and young women
**MSM=Men who have sex with men
***Others=people who inject drugs, people in prison, transgender, None, non-injecting drug users, and displaced persons
†IRR=Incidence rate ratio
Discussion
This study found high oral PrEP use among high-risk populations at substantial risk of HIV infection at baseline. Female HRPs were often eligible oral PrEP users at baseline. Old age was strongly associated with reduced rate of both oral PrEP eligibility and oral PrEP use. Married or cohabiting HRPs were strongly associated with increased oral PrEP use. These findings indicate willingness to use oral PrEP among high-risk populations at substantial risk of HIV infection.
High oral PrEP use at baseline has also been documented in previous studies that assessed oral PrEP acceptability among other key populations in East and Southern Africa (16). Oral PrEP use among HRPs is possibly because high-risk population groups perceived themselves to be at increased risk of HIV acquisition. A study among fishing communities in Uganda, reported a link between risk perception and acceptability to use oral PrEP (17). Because of the risky sexual behaviours among these population categories, this might explain the high oral PrEP use among them.
Female high-risk populations being more likely to be eligible oral PrEP users during this study, may be because most of our study participants were sex workers who possibly consider themselves to be at increased risk of HIV and other sexually transmitted infections due to involvement in sex work with multiple sex partners (18). Several of these observations were also reported in a study on HIV vulnerability among Sub-Saharan African migrants (19). In addition, since most of our study participants were married, another possible explanation for female being more likely to be eligible oral PrEP users could be that women had regular sexual partners of whom they never trusted and therefore considered using oral PrEP to protect themselves while sustaining their relationships. The importance of showing trust by having unprotected sex in relationships have widely been reported elsewhere (20, 21).
The connection between old age and oral PrEP use has been reported in other studies as an effect of high risky sexual behaviours among older people (22). In a cohort study conducted in Amsterdam, it was found that the rate of oral PrEP use was highest among men aged 40 years and older (15). However, in this study, HRPs aged 50 years and older were associated with reduced rate of oral PrEP use at baseline. This could be attributed to the lower proportion of older HRPs identified eligible for oral PrEP use in our study and could have possibly perceived themselves to be at lower risk of HIV infection. It has been documented that understanding the risk associated with high risky behaviour is the first step to oral PrEP use (23, 24).
Married or cohabiting HRPs were associated with oral PrEP eligibility and use at baseline. In many parts of Africa, the risk of HIV acquisition is known to be high among married or cohabiting couples especially where intimate partner violence exists (25). The risk of HIV infection among married couples is increased due to gender inequalities (26, 27). Gender inequalities, particularly in communities where men are allowed to have extra marital relationships (28) render women vulnerable to HIV infection from their husbands (29-31). As a result, women opt to use oral PrEP as a way of protecting themselves from contracting HIV from their partners. Another possible explanation is that women’s sexuality is often controlled by their husbands or male partners (32) such that refusing sex becomes difficult, because marriage is believed to be more respectable than divorce, and therefore, oral PrEP becomes a means to keep the peace in a marriage.
Study strengths and limitations
Our study utilizeda national oral PrEP dataset for high risk populations at substantial risk of HIV acquisition with differing oral PrEP use rate levels, thus giving us a nationwide outlook regarding oral PrEP eligibility and use. However, the study solely depended on secondary data and could not be used to analyse behaviour or attitude over a period of time. Secondly, we assessed for only oral PrEP eligibility and oral PrEP use rather than preference to continue using oral PrEP, for this reason, we could not account for any dropout rates. Further studies requiring primary data are needed to better understand willingness to continue PrEP and HRPs at substantial risk of HIV infection.
Conclusion
Despite low rate of oral PrEP eligibility among HRPs, this study found that oral PrEP use was high among this population category. Married or cohabiting persons had increased odds of PrEP use in Uganda during 2017-2021, suggesting a role for partner support. Intensified efforts may be needed to promote partner support to ensure PrEP use among high-risk populations in the country.
Conflict of Interest
The authors declare that they had no competing interests.
Acknowledgments
We acknowledge the Public Health Fellowship Program and the Ministry of Health, Uganda, for implementation support, Makerere University School of Public Health for support and oversight. We also thank Makerere University School of Public Health Monitoring and Evaluation Technical Support Program (METs) METS for the dataset of people at substantial risk of HIV infection.
References
- . Liu AY CS, Vittinghoff E, et al. Preexposure Prophylaxis for HIV Infection Integrated With Municipal- and Community-Based Sexual Health Services. 2016.
- Grant RM LJ, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. 2010.
- McCormack S DD, Desai M, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. The Lancet. 2016;387(10013):53–60. . 2016.
- Volk JE MJ, Phengrasamy T, et al. No new HIV infections with increasing use of HIV preexposure prophylaxis in a clinical practice setting:. 2015.
- Health R. Pre-exposure prophylaxis for HIV-negative persons with partners living with HIV. . 2017.
- H J. Current concepts for PrEP adherence. . 2016.
- Organization WH. Updated recommendations on first-line and second-line antiretroviral regimens and post-exposure prophylaxis and recommendations on early infant diagnosis of HIV. 2018.
- Marazzo. Pre-exposure prophylaxis for HIV in women. 2013.
- V. D. The FEM-PrEP trial of emtricitabine/tenofovir disoproxil fumarate (Truvada) among African women. . 2012.
- Hladik W SE, Berry M, Ganafa S, Kiyingi H, Kusiima J, et al. Men who have sex with men in Kampala, Uganda: results from a bio-behavioral respondent driven sampling survey. . 2017.
- report by Uganda Harm Reduction Network. Uganda harm reduction network- (UHRN) Annual report 2017. 2017.
- Baral S BC, Muessig K, Poteat T, Wirtz AL, Decker MR, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. 2012.
- Benn J, Koutantji, M., Wallace, L., Spurgeon, P., Rejman, M., & Healey, A. Feedback from incident reporting: Information and action to improve patient safety. 2009.
- Health. UMo. Consolidated Guidelines on the Prevention and Treatment of HIV in Uganda. Kampala, Uganda: Ministry of Health. 2018.
- UAC. National HIV and AIDS Strategic Plan 2015/2016–2019/2020. 2015.
- Eisingerich AB WA, Gomez GB, Garnett GP, Dybul MR, Piot PK. . Attitudes and Acceptance of Oral and Parenteral HIV Preexposure Prophylaxis among Potential User Groups: A Multinational Study. . PLOS ONE 2012;Jan 11;7(1):e28238.
- Kuteesa MO QM, Biraro S, Katumba KR, Seeley J, Kamali A, et al. . Acceptability and Predictors of Uptake of Anti-retroviral Pre-exposure Prophylaxis (PrEP) Among Fishing Communities in Uganda:A Cross-Sectional Discrete Choice Experiment Survey. . 2019;AIDS Behav. (10):2674–86.
- Longo JD SM, Diemer HS, Grésenguet G, Brücker G, Belec L. . Risk factors for HIV infection among female sex workers in Bangui, Central African Republic. . PLoS One 2017;Nov 6;12(11):e0187654. doi: 10.1371/journal.pone.0187654. PMID: 29108022; PMCID: PMC5673229.
- Voeten HA VD, Gregson S, Zaba B, White RG, de Vlas SJ, Habbema JD. . Strong association between in-migration and HIV prevalence in urban sub-Saharan Africa. . Sex Transm Dis. 2010( Apr;37(4):240-3. doi: 10.1097/OLQ.0b013e3181c3f2d0. PMID: 19959971; PMCID: PMC3514976.).
- Okafor UO, Crutzen, R., Aduak, Y., Adebajo, S., & Van den Borne, H. W. Behavioural interventions promoting condom use among female sex workers in sub-Saharan Africa: A systematic review. African Journal of AIDS Research, 16(3), 257–268. https://doi.org/10.2989/16085906.2017.1358753. 2017.
- Rutakumwa R MM, Kiwanuka T, Bagiire D, Seeley J. . Why do men often not use condoms in their relationships with casual sexual partners in Uganda? Cult Health Sex. . 2015(2015;17(10):1237-50. doi: 10.1080/13691058.2015.1053413. Epub 2015 Jul 9. PMID: 26158527.).
- Young I, Li J, McDaid L. Awareness and willingness to use HIV pre-exposure prophylaxis amongst gay and bisexual men in Scotland: implications for biomedical HIV prevention. PLoS One. 2013;8(5):e64038.
- Pillay D, Stankevitz K, Lanham M, Ridgeway K, Murire M, Briedenhann E, et al. Factors influencing uptake, continuation, and discontinuation of oral PrEP among clients at sex worker and MSM facilities in South Africa. PLoS One. 2020;15(4):e0228620.
- RM Delabre JG, A Bernier, R Stranz, C Mey, A Vilotitch, V Schlegel, H Sweers, S Chanos, K Jonas, B Spire, D Rojas Castro. HIV-related Risks and Interest in Pre-exposure Prophylaxis (PrEP) among Transgender Respondents of the Community-based Survey “Flash! PrEP in Europe” 2018.
- Mkandawire L WC, Stevens PE, et al. . Marriage as a risk factor for HIV: learning from the experiences of HIV-infected women in Malawi. Glob Public Health. 2013;8(2):187–201. .
- Mtenga S PC, Sonja M, et al. . Prevalence and social drivers of HIV among married and cohabitating heterosexual adults in south-eastern Tanzania: analysis of adult health community cohort data. . Glob Health Action. 2015;8:28941.
- Musheke M MS, Bond V. . Why do marital partners of people living with HIV not test for HIV? A qualitative study in Lusaka, Zambia. BMC Public Health. 2016;16(1):882.
- Auerbach JD PJ, Caceres CF. . Addressing social drivers of HIV/AIDS for the long-term response: conceptual and methodological considerations. . Global Public Health 2011;6(3):S293–309 2011.
- (WHO). JUNPoHAUatWHO. AIDS epidemic update 2009. Geneva: UNAIDS; 2009.
- Abdulazeez A AE, Naphthali R. . Concurrent infection of HIV-! And HIV-2 serotypes in Adamawa State Nigeria. World J Med Sci. 2008;3:15–8. . 2008.
- South African national HIV prevalence, Incidence and behaviour survey, 2012. [press release]. Cape Town: HRSC Press; 2015. 2015.
- Stephen Ojiambo Wandera BK, Patricia Ndugga and Allen Kabagenyi. . Partners’ controlling behaviors and intimate partner sexual violence among married women in Uganda. . BMC Public Health (2015) 15:214.


Comments are closed.