Mpox knowledge, vaccine attitudes, and vaccine concerns among healthcare workers, Kampala Metropolitan Area, Uganda, February 2025.
Authors: Loryndah Olive Namakula1, Richard Migisha1, Benon Kwesiga1, Alex Riolexus Ario1 Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Ministry of Health, Kampala Uganda. Correspondence: Tel: 0777650580, Email: olivenamakula@uniph.go.ug,
Summary
Background: Vaccination is one of the key outbreak countermeasures against mpox. However, it is challenged by vaccine hesitancy. Not only are healthcare workers one of the most at-risk populations prioritized for vaccination, they also play a crucial role in health-education, health-promotion, and vaccine advocacy. We assesed mpox knowledge, and vaccine attitudes and concerns among the healthcare workers in the Kampala Metropolitan area (KMA), Uganda, to guide the Mpox vaccination program.
Methods: We conducted a cross-sectional study using a semi-structured self-administered questionnaire among 423 healthcare workers. Kampala Metropolitan area was purposively selected as it had 74.6% of the Mpox cases in the country at the time. In each of the districts, the highest level of healthcare facility and a randomly selected primary-level-care facility were selected. A knowledge score of ≥60% was considered adequate knowledge, and an attitude score ≥60% was considered a good attitude.
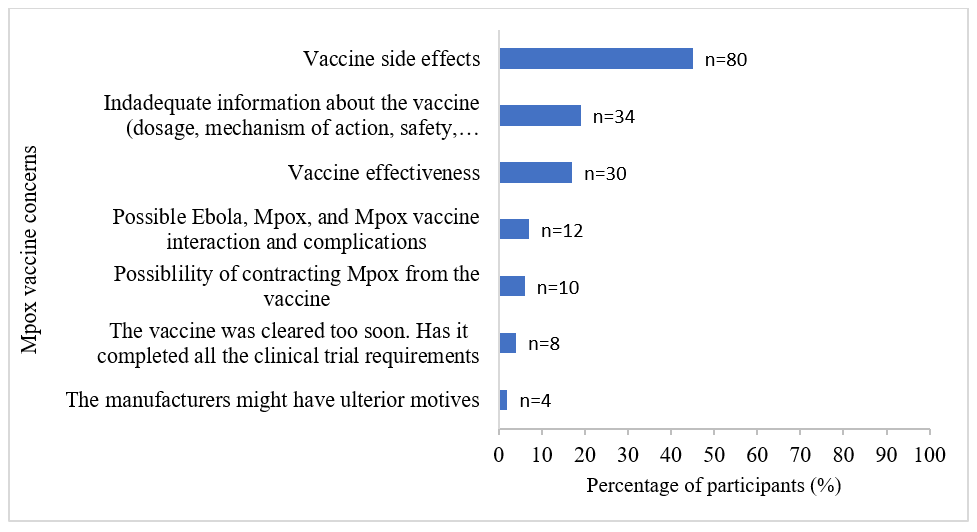
Results: All the 423 study participants had heard about Mpox, but only 44% (186) had adequate knowledge about Mpox. Only 44% (186) were aware that Mpox vaccines exist. Most 68.3% (289) of the participants had a positive attitude towards the Mpox vaccines; 71% (300) believed the vaccines are effective, and 52% (219) believed they are safe. Complacency was low, and 79% (334) agreed that getting vaccinated would protect their loved ones. Forty-two percent (178) of the participants expressed concerns about the Mpox vaccine, especially; vaccine safety 80(45%), effectiveness 30(17%), the fact that they aren’t well informed about the vaccines 34(19%), and possible interaction with Ebola infection 12(7%).
Conclusion: Less than half of the healthcare-workers had adequate knowledge about mpox, and key knowledge gaps which should be addressed were identified. Most of the healthcare-workers had a positive attitude towards the mpox vaccine, which set a good platform for advocacy. Healthcare-workers’ concerns regarding the Mpox vaccine were identified. Vaccine campaigns addressing the healthcare-workers’ concerns could improve their attitude towards the vaccine, and ultimately increase vaccine advocacy and intent to get vaccinated.
Background
As of August 14, 2024, the World Health Organization (WHO) recommended and approved vaccines for Mpox. The vaccines can be administered as a pre-exposure prophylaxis for people at higher risk of getting Mpox, and can also be administered as post- exposure prophylaxis for people who have been in contact with someone with Mpox, within 4 days of exposure, or up to 14 days if the person has not developed symptoms yet(1). On January 21, 2025, the 10,000 doses of Mpox vaccine were delivered to Uganda(2).
According to the national situation report on mpox, as of January 22, 2025, 74.6% (1,646) of the 2,209 Mpox cases in the country were from the Kampala Metropolitan Area (KMA). In view of the limited vaccines, the Ministry of Health planned to conduct the vaccination in phases, prioritizing the most affected areas, and high-risk groups such as sex workers and healthcare workers among others. Noteworthy, Uganda has experienced vaccine hesitancy in the past, hindering the efforts to combat outbreaks (3-5). Healthcare workers are not only one of the most at-risk populations prioritized for Mpox vaccination, they also play a key role in health-education, health-promotion, and vaccine advocacy. Establishing the mpox knowledge, and vaccine attitudes and concerns among healthcare workers is crucial in guiding key talking points to address knowledge gaps and vaccine concerns to improve vaccine advocacy and intent to get vaccinated. We determined the mpox knowledge, and vaccine attitudes, and concerns among healthcare workers in the Kampala Metropolitan Area, Uganda, to guide the Mpox vaccination program.
Methods
We conducted a cross-sectional study among Healthcare workers (clinical and non-clinical) working at public hospitals in the KMA. In the context of limited vaccine supply and targeted vaccination, the study area, KMA, was purposively selected as it bared the biggest burden of Mpox, with 74.6% (1,646/2,209) of the cases in the country as of January, 22, 2025.
Using the Keish Lesly formula for cross-sectional studies we enrolled a total of 423 study participants.
We collected data on social demographic characteristics, knowledge on Mpox, as well as attitudes and concerns towards the mpox vaccine. Knowledge on mpox was assessed using seven questions; the signs and symptoms, mode of transmission, incubation period, possibility of re-infection, who is as at higher risk of mpox, if mpox has specific treatment, and if it has a vaccine. Attitude towards the mpox vaccine was assessed using seven vaccine statements, and the participants asked if they had any concerns about the vaccine, those with concerns were requested to state them.
Knowledge on mpox: for the seven knowledge questions, “yes” was indicated as a correct answer and scored 1, and “no or don’t know” answers were scored 0. Three of the seven knowledge questions had multiple answers; leading to a maximum score of 22. A cut off point of 60% was set; one was considered to be knowledgeable about Mpox if they scored ≥60% and not knowledgeable if they scored ≤59%. Regarding attitude, the seven questions were scored on a 3-point Likert scale (disagree, agree and don’t know). The responses were scored 1 for those who agreed to positive statements and disagreed to negative statements, and a score of 0 for don’t know and no responses. A score of ≥60% was considered good attitude towards the Mpox vaccine, and a score of ≤59% was considered a negative attitude. Results on concerns about the mpox vaccine were presented using frequencies and proportions.
The Ministry of Health (MOH), Uganda, provided administrative clearance and authorized this study. The US Centers for Disease Control and Prevention provided a non-research determination (NRD) for non-human subjects. We sought verbal consent from respondents during data collection. Participants were told that their participation was voluntary and that there would be no negative consequences if they refused to participate (none declined). During data collection, respondents were assigned unique identifiers instead of names to protect their confidentiality. Information was stored in password-protected computers and was not shared with anyone outside the investigation team.
Results
Socio-demographic characteristics of healthcare workers, Kampala Metropolitan Area, Uganda, February 2025
A total of 423 participants were enrolled. The mean (SD) age of the study participants was 31.6 ±7.6, and slightly over half 59% (250) were female. Most 62.4% (264) of them had been health workers for < 5 years, and the majority 84% (354) had received the Covid-19 vaccine (Table 1).
Table 1: Socio-demographic characteristics of healthcare workers, Kampala Metropolitan Area, Uganda, February 2025
| Social demographic characteristic | Frequency (N=423) | Percentage (%) |
| Sex | ||
| Female | 250 | 59 |
| Male | 173 | 41 |
| Age | ||
| 20-30 | 233 | 55 |
| 31-40 | 141 | 33 |
| >40 | 49 | 12 |
| Marital status | ||
| Single | 185 | 43.7 |
| Married | 227 | 53.7 |
| Divorced/separated/widowed | 11 | 2.6 |
| Level of education | ||
| Certificate | 170 | 40 |
| Diploma | 123 | 29 |
| Degree | 111 | 26 |
| Masters or PHD | 19 | 5 |
| Healthcare role | ||
| Non-clinical (administrators, janitors, security, etc.) | 72 | 17 |
| Allied health (Pharmacy, laboratory, physiotherapy) | 78 | 19 |
| Nurses and Midwives | 209 | 49 |
| Doctors | 64 | 15 |
| Health facility level | ||
| District and Primary-care facilities | 142 | 34 |
| Regional Referral Hospital | 123 | 29 |
| National Referral Hospital | 158 | 37 |
| Years in healthcare service | ||
| <5 | 264 | 62.4 |
| 5-10 | 103 | 24.4 |
| >10 | 56 | 13.2 |
| Comorbidities | ||
| Yes | 39 | 9 |
| No | 384 | 91 |
| Did you get the COVID-19 vaccine? | ||
| Yes | 354 | 84 |
| No | 39 | 16 |
Mpox knowledge
All of the participants had heard about mpox, but only 44% had adequate knowledge about mpox. Over 115(27%) knew all the signs and symptoms, 49 (12%) correctly stated all the modes of transmission, 93(22%) correctly stated the different categories of people at a higher risk of getting mpox, 110 (26%) correctly stated the different categories of people at a higher risk of getting worse outcomes, 186 (44%) were aware that mpox vaccines exist, 187 (44.2%) correctly stated the incubation period, 225(53%) were aware that one can get re-infected with mpox, and 212(50%) correctly stated that there is no specific medication for mpox.
Attitude towards the mpox vaccine
Most 289 (68.3%) of the study participants had a positive attitude towards the mpox vaccine. Most expressed confidence in the mpox vaccine; 300 (71%) believed that the vaccine is effective, and 219 (52%) believe that it is safe. Complacency was low; only 91 (22%) agreed that mpox is not severe enough to warrant vaccination, and 19% (81) believed that their immune system is strong enough to obviate the need for vaccination. A strong sense of collective responsibility was also observed, with 79% (334) of the participants agreeing that vaccination contributes to the protection of others in the community (Table 2).
Table 2: Attitudes towards the mpox vaccine among health care workers, Kampala Metropolitan Area, Uganda, February 2025
| (Attitude statement: n=423) | Agree
n (%) |
Disagree
n (%) |
Don’t know
n (%) |
| The Mpox vaccine is safe | 219 (52) | 64 (15) | 140 (33) |
| The Mpox vaccine is effective in protecting me against Mpox | 300 (71) | 123 (29) | – |
| Getting the Mpox vaccine will protect me and my loved ones against Mpox | 334 (79) | 89 (21) | – |
| There are better ways of preventing Mpox than vaccination | 264 (62) | 159 (38) | – |
| Mpox is not so severe that I should get vaccinated | 91 (22) | 332 (78) | – |
| My immune system is strong, I don’t need to get the Mpox vaccine | 39 (9) | 239 (57) | – |
| Getting more information about the Mpox vaccine will make me more willing to get vaccinated | 239 (57) | 39 (9) | 145 (34) |
Concerns about the mpox vaccine
When asked if they had any concerns about the mpox vaccine, 178 (42%) of the study participants expressed concerns about the mpox vaccine. The participants were concerned about possible side effects from the vaccine 80(45%), the fact that they had not receive enough information about the mpox vaccine 34(19%), vaccine effectiveness 30(17%), and possible interaction between the vaccine, mpox infection, and Ebola infection 12(7%) as there was an Ebola outbreak at the time, the speed at which the vaccine was cleared for use 8(4%), and the fact that the government might have had ulterior motives for vaccinating the population 4(2%) (Figure 1).
Discussion
Less than half of the participants had adequate knowledge about mpox, and only 44% were aware that mpox vaccines exist. When informed that mpox vaccines do exist, most of the participants had a positive attitude towards the vaccines; majority expressed confidence in the vaccine, there was low compliancy, and a strong sense of collective responsibility was observed. Forty-two percent of the participants expressed concerns about the mpox vaccine, specifically regarding vaccine side effects, vaccine effectiveness, the possible interaction between mpox, the mpox vaccine, and ebola disease, and the fact that they didn’t have enough information about the mpox vaccines.
The finding that only 44% were knowledgeable about the Mpox is consistent with what has been found elsewhere(6, 7). The fact that there were some knowledge gaps identified is concerning, especially since this study was conducted six months into the outbreak in Uganda, and years since it was declared a Public Health Event of International Concern. More than half of the healthcare workers weren’t aware that mpox vaccine exist. This is particularly concerning as healthcare workers are responsible for health education, and ultimately vaccine advocacy. Furthermore, healthcare workers are one of the most at-risk populations and hence they are prioritized for vaccination.
The healthcare workers expressed a good attitude towards the mpox vaccine. A positive attitude towards a vaccine has been known to positively influence vaccine advocacy and willingness to recommend the vaccine, as well as one’s intention to get vaccinated.(8) This study highlights the concerns the healthcare workers have about the mpox vaccine, which provide information on key talking points for vaccination campaigns. Addressing these concerns in the vaccine campaign program could increase vaccine advocacy, and willingness and intent to get vaccinated. This can also increase the knowledge base among the healthcare workers and facilitate sharing of facts to their patients and the population at large.
Study limitations
Including only the participants on duty on the day of the interview could have introduced a selection bias. However, we checked and established that for most of the health facilities, the healthcare workers work day and night duties in turns, giving almost every healthcare worker an equal probability of being on a day duty shift on the day of the interview.
Conclusion
Less than half of the healthcare-workers had adequate knowledge about mpox, and key knowledge gaps to be addressed were identified. Most of the healthcare-workers had a positive attitude towards the mpox vaccine, which set a good platform for advocacy. The study also highlighted the healthcare-workers’ concerns regarding the Mpox vaccine. Mpox vaccine campaigns addressing the healthcare-workers’ concerns could improve their attitude towards the vaccine, and ultimately increase vaccine advocacy and intention to get vaccinated.
Competing interests
The authors declare no competing interests, be it financial or personal.
Author contribution
LON: Participated in the conception, design, analysis, and interpretation of the study results, drafted the bulletin; RM, BK, ARA reviewed the report and bulletin for intellectual content and scientific integrity.
Acknowledgments
The authors extend their gratitude to the staff of Uganda Public Health Fellowship Program for their technical support. The authors also acknowledge the support of the teams at the different health facilities which participated in the study, and the study participants who volunteered the information.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- WHO. Mpox: Vaccines 2025 [Available from: https://www.who.int/news-room/questions-and-answers/item/mpox-vaccines.
- Health EUP. HERA delivers mpox vaccines to support Uganda’s outbreak response 2025 [Available from: https://health.ec.europa.eu/latest-updates/hera-delivers-mpox-vaccines-support-ugandas-outbreak-response-2025-01-21_en.
- Kabagenyi A, Wasswa R, Nannyonga BK, Nyachwo EB, Kagirita A, Nabirye J, et al. Factors associated with COVID-19 vaccine hesitancy in Uganda: a population-based cross-sectional survey. International Journal of General Medicine. 2022;15:6837.
- Bongomin F, Olum R, Andia-Biraro I, Nakwagala FN, Hassan KH, Nassozi DR, et al. COVID-19 vaccine acceptance among high-risk populations in Uganda. Therapeutic Advances in Infectious Disease. 2021;8:20499361211024376.
- Kanyike AM, Olum R, Kajjimu J, Ojilong D, Akech GM, Nassozi DR, et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Tropical medicine and health. 2021;49(1):37.
- Ajayi PO, Esan DT, Ipinnimo TM, Olanrewaju MT, Solomon OO, Atanda-Owoeye OO. Knowledge and awareness of human mpox infection among healthcare workers: a cross-sectional study in southwestern Nigeria. Asian Pacific Journal of Tropical Medicine. 2023;16(6):245-52.
- Jahromi AS, Jokar M, Sharifi N, Kashkooli S, Rahmanian K, Rahmanian V. Global knowledge and attitudes towards mpox (monkeypox) among healthcare workers: a systematic review and meta-analysis. International Health. 2024;16(5):487-98.
- Mahameed H, Al-Mahzoum K, AlRaie LA, Aburumman R, Al-Naimat H, Alhiary S, et al. Previous vaccination history and psychological factors as significant predictors of willingness to receive mpox vaccination and a favorable attitude towards compulsory vaccination. Vaccines. 2023;11(5):897.


Comments are closed.