Investigation of yellow fever outbreak associated with swamp-based rice cultivation, Kibuku District, Uganda, December 2024
Authors: Annet Mary Namusisi1* Daniel Wenani1, Paul Okello1, Richard Migisha1, Fred Nsubuga2, Benon Kwesiga1, Alex Riolexus Ario1 Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda; 2Uganda National Expanded Program on Immunization, Ministry of Health Uganda, Kampala, Uganda Correspondence*: Tel: +256785859760, Email: annetnamusisi@uniph.go.ug
Summary
Background: In August 2024, the Uganda Ministry of Health was notified of three laboratory-confirmed yellow fever cases in Kibuku District. We estimated the outbreak scope, characterized cases, assessed transmission risk factors, and recommended evidence-based control measures.
Methods: We defined a suspected case as acute onset of fever plus ≥2 of the following symptoms: altered mental state, abdominal pain, diarrhea, vomiting, headache, unexplained bleeding and jaundice, in a resident of Kibuku District from June 1-December 31,2024. We defined a probable case as a suspected case with positive IgM for YF specific antibodies and is unvaccinated against yellow fever. A confirmed case was defined as a probable case with a positive Plaque Reduction Neutralization Test (PRNT). We conducted case-patient reviews, reviewed medical records, conducted risk assessment, obtained samples from suspected case-patients and shipped them to the Uganda Virus Research Institute (UVRI) for testing.
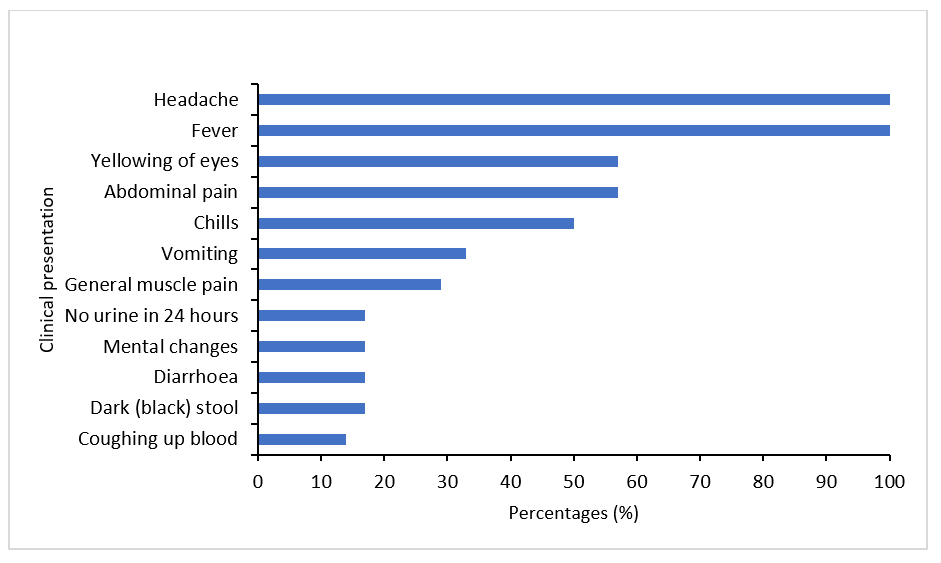
Results: We identified 3 confirmed, 4 probable, and 35 suspected cases, with no deaths. The mean age among probable and confirmed cases was 12 years. Common symptoms included fever (100%), headache (100%), jaundice (60%), and abdominal pain (60%). All confirmed cases were from Kasasira Subcounty and were unvaccinated. All reported rice farming near swampy areas, indicating likely exposure to infected mosquitoes. One probable case was identified in December, suggesting ongoing transmission.
Conclusion: Sylvatic yellow fever outbreak occurred in Kibuku District. The outbreak was linked to exposure to mosquito bites during rice cultivation and no vaccination. We recommend strengthening routine yellow fever vaccination and implementing targeted vector control in high-risk swampy areas.
Background
Yellow fever is an acute viral hemorrhagic disease caused by a flavivirus in the Flaviviridae family (1). It is transmitted to humans through the bite of infected Aedes or Haemagogus mosquitoes, and occurs in three main transmission cycles: sylvatic (jungle), intermediate (savannah), and urban (2, 3). The disease has 2 phases; the acute phase characterized by fever, muscle pain, backache, rigors, loss of appetite, nausea, vomiting and abdominal pain; the toxic phase is characterized by jaundice, abdominal pain with vomiting, unexplained bleeding from the mouth, nose, eyes and stomach, appearing in vomit, urine and feaces. Yellow fever has no cure but prevention is mainly by vaccination (4).
Uganda is located within the yellow fever endemic zone (5). Since 2016, multiple districts in Uganda, including Masaka, Wakiso, Buikwe, and Bundibugyo, have reported outbreaks (6). In October 2022, Uganda introduced mandatory yellow fever vaccine into the routine immunization schedule, given at nine months of age (7). Despite the vaccination campaigns conducted, gaps in coverage and surveillance leave some population at risk.
On August 13, 2024, the Uganda Ministry of Health (MoH) was notified of three positive yellow cases from Kasasira Primary School, Kibuku District. We estimated the scope of the outbreak, characterized the cases, assessed associated risk factors for transmission, and evaluated the presence of active viral transmission.
Methods
The outbreak occurred in in Kibuku District, Eastern Uganda. Kibuku District is characterized by an extensive network of wetlands associated with Mpologoma River(8). These wetlands facilitate extensive rice farming, fishing, and subsistence agriculture.
We defined a suspected case as acute onset of fever plus ≥2 of the following symptoms: altered mental state, abdominal pain, diarrhea, vomiting, headache, unexplained bleeding and jaundice, in a resident of Kibuku District from June 1-December 31, 2024. A probable case was defined as a suspected case with positive IgM for YF specific antibodies and is unvaccinated against yellow fever. A confirmed case was defined as a probable case with positive Plaque Reduction Neutralization Test (PRNT).
We visited the health facility that had confirmed yellow fever cases and other health facilities within Kibuku District. We further conducted case search in the affected community. We reviewed medical records of identified cases and conducted interviews using a case investigation form we designed. We line-listed suspected cases and took off blood samples for a yellow fever test from Uganda Virus Research Institute.
We conducted an environmental assessment to identify possible risk factors of yellow fever transmission. We observed the farm lands where confirmed cases cultivated from and determined the distance of their homes from the farm lands.
We conducted six case interviews using a yellow fever case investigation form. Case-patients were interviewed on potential risk factors that occurred prior to symptom onset.
We trapped mosquitoes from around the homesteads and farmlands of the three confirmed cases to identify their species and morphology. We collected water samples from swamps close to the confirmed cases’ homes to facilitate our findings about the presence of Aedes mosquito species in the homesteads
We performed descriptive epidemiology and described data by person, place and time. We analyzed data on only 7 cases.
to conduct this project under the Non-Research Determination criteria was obtained from the U.S Centers of Disease Control and Prevention (CDC). We sought authorization from the District Health Office and health facility In-charges, to access case-patients’ medical records. Informed consent and verbal assent were sought from the case-patients prior to conducting interviews.
Results
Descriptive epidemiology
Between June and December 2024, we identified a total of 42 yellow fever case-patients in Kibuku District: 3 confirmed, 4 probable, and 35 suspected. Their mean age was 12years (10-14). Most were female, 6 (86%), muslim by religion 5 (71%), and were from Kasasira town council 5 (71%). All the case-patients presented with fever and headache 7 (100%) and the majority presented with yellow eyes 4 (60%), abdominal pain 4 (60%) and chills 3 (50%) (Figure 1). The 3 confirmed case-patients were sparsely distributed in Kasasira subcounty.
Over 6 yellow fever cases (both probable and confirmed) were registered in the district during the month of June, where as one case was registered in December 2024.
Confirmed yellow fever case summaries
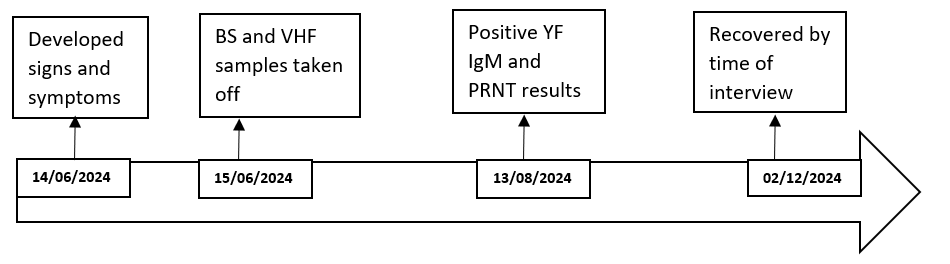
Confirmed case one was a 12-year-old female from Bugiri 2 village, Kasasira Parish, Kibuku District, developed high-grade fever with chills, rigors, headache, and abdominal pain on June 14, 2024. She lost consciousness and was taken to Kasasira Health Centre III, where a malaria rapid diagnostic test was positive. She was hospitalized, and samples for viral hemorrhagic fevers, including yellow fever, were collected. She later exhibited jaundice and hematuria but no vomiting. Serological testing on August 13, 2024, revealed positive IgM and PRNT titers for yellow fever. Her family engages in rice farming near her home, and she sleeps under a mosquito net, with no history of yellow fever vaccination. By December 2024, she was asymptomatic (Figure 2).
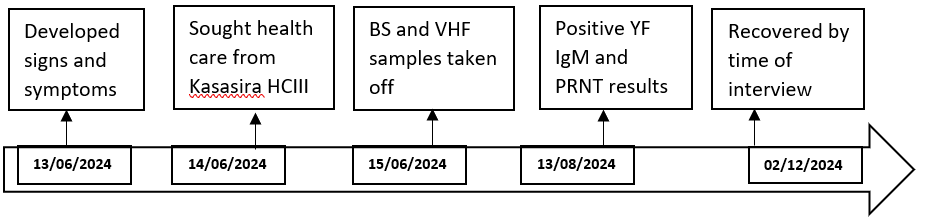
Confirmed case two was a 10-year-old female in Primary 3 from Kasasira 2 village, Kibuku District, presented with fever, headache, dizziness, altered mentation, and passing deep yellow urine on June 13, 2024. She was taken to Kasasira HCIII on June 14, 2024, where an mRDT was positive for malaria, and samples for viral hemorrhagic fever (VHF) were collected and shipped to Uganda Virus Research Institute (UVRI) on June 15. She was promptly started on antimalarials. Laboratory results later indicated positive yellow fever IgM antibodies and a PRNT titer of 20, suggesting recent yellow fever infection (Figure 3).
Probable cases that tested negative on confirmatory with PRNT tests for yellow fever disease
There were 4 individuals, three of whom were pupils of primary level of education at Kasasira primary school, and the fourth was a pupil at another school in the nearby subcounty to Kasasira in Kibuku District, who developed signs and symptoms suggestive of yellow fever. They had VHF samples taken off which tested positive for IgM specific YF antibodies but negative PRNT. All carried-out rice farming from nearby swamps, had no travel history to other districts and had never been vaccinated against yellow fever.
From observations made near farmlands and homes of confirmed case-patients, there were no forests, but rice farming was done in swamps that were about 5km from their homes. These had stagnant water which was a fertile source for mosquito breeding. In addition, there were fish ponds near the homes of one of the confirmed cases, where fish rearing was done.
Findings for probable exposure risk factors to yellow fever disease
Among 6 case-patients, not being vaccinated against yellow fever 6 (100%), working from the agricultural field 5 (83%), visiting a swamp before exposure period, 5 (83%) and cultivation in a swamp 5 (83%) were the likely exposures to yellow fever disease in the district.
Discussion
The outbreak affected several sub-counties with Kasasira the most affected. The outbreak was most likely sylvatic in nature, propagated by agricultural activities in swampy environments and lack of vaccination in the community. Our findings are consistent with a study in Central and Southwestern Uganda, where yellow fever was transmitted by mosquito bites during farming in swampy areas (6). There was clustering of confirmed cases within Kasasira town council suggesting localized transmission, likely driven by environmental and behavioral factors. There was one probable case-patient registered in December, with a time lag of five months after confirmation of three case-patients in June. This finding suggests recurrent yellow fever outbreaks and likely endemicity of the disease in the district, which is likely due to decline in population immunity to infection, increased human activities such as swamp reclamation, and climate change (6, 9). There is need to re-enforce prevention and control strategies against yellow fever, such as vaccination. The primary economic activity of rice farming in swamps emerged as a likely risk factor, as stagnant water in swamps provides breeding grounds for Aedes mosquito species, the primary vector for yellow fever (2). These findings are consistent with global patterns where proximity to water bodies and wetlands contributes to higher YF transmission risk (10).
Probable cases with positive IgM but negative PRNT results indicated possible cross-reactivity with other flaviviruses, such as Dengue, Zika or West Nile viruses, highlighting the need for comprehensive differential diagnosis to avoid misdiagnosis and missed opportunities for outbreak control (11). Surveillance on other flavi viruses is required in these communities to avoid future outbreaks.
Notably, all case-patients were unvaccinated against yellow fever, underscoring gaps in immunization coverage despite the country’s introduction of routine yellow fever vaccination in October 2022. Vaccination is a critical preventive measure and has been shown to reduce risk of disease and outbreaks (12). There is need for frequent mass-vaccinations in the district to build herd immunity especially among the older population who existed before the introduction of routine yellow fever vaccination in the immunization schedule
Our findings should be interpreted with the following limitation. First, Kibuku District has a high malaria burden. Malaria clinical manifestation is similar to yellow fever. This likely led to missing out yellow fever cases during active case search. This could have led to an under estimation of the magnitude of the outbreak.
Conclusion
The outbreak occurred among children of school going age and Kasasira subcounty was the most affected. All the confirmed cases were not vaccinated against yellow fever, and engaged in rice cultivation from swamps, which could be the possible risk factor to acquiring yellow fever disease.
Recommendations
We recommended mass vaccination against Yellow Fever among residents of Kibuku District to build community-level immunity. Ongoing Yellow Fever surveillance should be implemented at the community level to enable timely detection of cases.
Conflict of interests
The authors declare that they have no conflict of interests.
Authors’ contributions
AMN, DW, PO, designed the study and contributed to the data collection and analysis. AMN led the writing of the manuscript. AMN, DW, PO, RM, FN, BK, ARA, participated in bulletin writing and review to ensure scientific integrity and intellectual content. All the authors contributed to the final draft of the bulletin.
Acknowledgements
We appreciate the management of Kibuku District Local Government for their stewardship, and the community for their participation in this investigation. We also thank the Uganda national Institute of Public health for their technical support and financial support during this investigation.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Gaythorpe KA, Hamlet A, Jean K, Garkauskas Ramos D, Cibrelus L, Garske T, et al. The global burden of yellow fever. eLife. 2021;10.
- WHO. Yellow fever. 2023.
- Nwaiwu AU, Musekiwa A, Tamuzi JL, Sambala EZ, Nyasulu PS. The incidence and mortality of yellow fever in Africa: a systematic review and meta-analysis. BMC Infectious Diseases. 2021;21(1):1089.
- Yellow Fever: Symptoms, Diagnosis, and Treatment [Internet]. 2024. Available from: https://www.cdc.gov/yellow-fever/symptoms-diagnosis-treatment/index.html.
- Kwagonza L, Masiira B, Kyobe-Bosa H, Kadobera D, Atuheire EB, Lubwama B, et al. Outbreak of yellow fever in central and southwestern Uganda, February–may 2016. BMC Infectious Diseases. 2018;18(1):548.
- Kwagonza L, Masiira B, Kyobe-Bosa H, Kadobera D, Atuheire EB, Lubwama B, et al. Outbreak of yellow fever in central and southwestern Uganda, February-may 2016. BMC Infect Dis. 2018;18(1):548.
- WHO. Uganda introduces life-saving yellow fever vaccine into routine immunization programme. 2023.
- Ministry MEaWo. Mpologoma catchment management Plan. 2018.
- hub Ohp. Disease outbreaks, endemics, epidemics and pandemics 2020 [Available from: https://www.onehealthpoultry.org/disease-outbreaks-endemics-epidemics-and-pandemics/.
- Ramlee S. MOSQUITO SPECIES AND OUTDOOR BREEDING PLACES IN RESIDENTIAL AREAS IN MALAYSIA. The Southeast Asian journal of tropical medicine and public health. 2013;Vol 44 No. 6 November 2013.
- Gadia CLB, Manirakiza A, Tekpa G, Konamna X, Vickos U, Nakoune E. Identification of pathogens for differential diagnosis of fever with jaundice in the Central African Republic: a retrospective assessment, 2008–2010. BMC Infectious Diseases. 2017;17(1):735.
- WHO. Yellow fever. 2022.


Comments are closed.