INCIDENCE OF PRETERM BIRTHS ADMISSIONS ON THE RISE IN UGANDA: IMPLICATIONS FOR THE HEALTH CARE SYSTEM
Quarterly Epidemiological Bulletin: January–March, 2021 Volume 6 / Issue 1/Article No. 3 Authors: Job Morukileng1, Wilberforce Mugwanya2, Robert Mutumba2, and Maureen Katusiime1 Affiliations: 1Uganda Public Health Fellowship Program, Kampala, Uganda; 2Ministry of Health Uganda, Reproductive Health Department, Kampala, Uganda Corresponding Author: Morukileng Job, jmorukileng@musph.ac.ug
Summary
Premature birth is a growing concern globally. Complications of preterm births are the single largest cause of neonatal deaths and the second leading cause of deaths among children aged <5 years globally. There is paucity of literature on the current trend of preterm births in Uganda. In this study, we described the trends and distribution of preterm births in Uganda between 2015-2019 for advocacy and targeting of interventions.
We conducted a countrywide descriptive analysis of preterm birth admissions data,2015- 2019 period Uganda. Preterm birth is defined as birth that occurs before 37 weeks of gestation. We abstracted data from the District Health Information System (DHIS2), disaggregated into national, regional, and district levels. We calculated the annual incidence rates by dividing the number of preterm births admissions by the total live birth (LB). We obtained the mean annual incidence rates by adding yearly incidence rates for the five years of study and dividing by five. We used line graphs to demonstrate the trend of incidence at national and regional levels and used choropleth maps to show district level distribution of incidence. We tested significance of the observed trends using logistic regression.
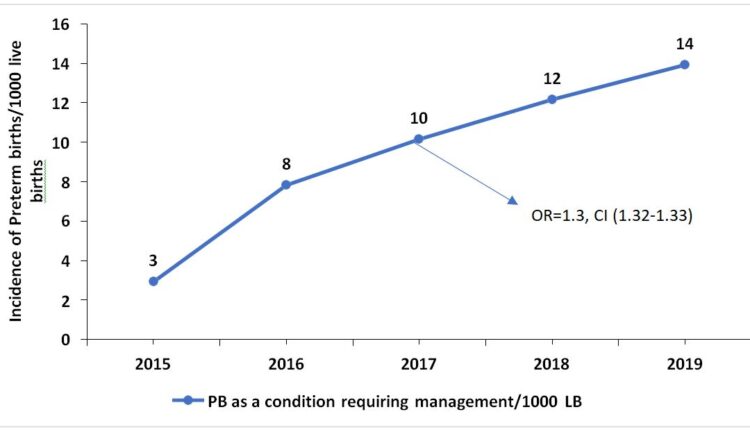
Nationally, the incidence rate of preterm births admissions/1,000 LB has significantly been increasing (OR=1.3, CI=1.32-1.33) by an annual average of 45.6%. Consistent with the national trend, the incidence rate significantly increased in all the four regions of Uganda. However, the central had the highest mean annual incidence of 12/1000 livebirths while the north and east had the lowest mean annual incidence rate of 7/1000 livebirths. We also observed minimal regional clustering in the distribution of incidence in Uganda.
The incidence of preterm births admissions is on the rise and is distributed across the country. As incidence rises, the Ministry of Health needs to understand the level of readiness of the health facilities to manage preterm births and plan accordingly as well as conduct further studies to understand contributors to the increasing trend for focused interventions.
Background
Premature birth is a growing concern globally[1]; with many countries reporting increasing trend [2]. Preterm Birth is birth that occurs before 37 weeks of pregnancy, sub-categorized as extremely preterm (<28 weeks), Very preterm (28 to <32 weeks) and moderate to late preterm (32 to <37 weeks)[3]. Every year, an estimated 15 million babies are born too early and approximately 1 million children die each year due to complications of preterm birth globally[4].
Whereas 60-85% of preterm births occur in Africa and South Asia[3, 5], preterm birth is a global problem. In lower-income countries (LICs), 12% of babies are born too early compared with 9% in higher-income countries (HICs). Within countries, poorer families are at higher risk of preterm birth. Disparities exist in survival rates of preterm babies around the world[3]. In LICs, half of the babies born at or below 32 weeks die due to failure to provide feasible, cost-effective care, such as warmth, breastfeeding support, and basic management of infections and breathing difficulties while in HICs, almost all these babies survive[6].
Although the causes of preterm birth are unknown in about 50% of the cases, preterm birth can be caused by problems with the fetus, the mother, or both. Among the causes are the placental abruption, incompetent cervix, hormonal imbalances and infections. Untreated urinary infections and bacterial vaginosis are said to double the risk of premature birth.
Other risk factors for premature birth are anemia, slow maternal weight gain, too soon or too late pregnancy, stressful work habits, smoking, drinking alcohol, and using drugs like cocaine [7]. Maternal risk factors for preterm birth include having a previous premature birth, being pregnant with twins or multiples babies and chronic conditions such as diabetes and high blood pressure[3]. Many mothers of twins and multiple babies go into premature labour spontaneously; about half of all twin pregnancies deliver at 36 weeks or less and a half of triplets deliver before 32 weeks of pregnancy[7]. Others may need to have premature labour induced because of complications during pregnancy or caesarean birth, whether for medical or non-medical reasons[3].
Uganda has a high preterm births rate of 14 per 1000 live births[4]. These preterm births are directly responsible for 8/27 neonatal deaths per 1,000 live births in Uganda[8] and remains among the top three causes of death during the neonatal period in Uganda[9]. Preterm birth underlies neonatal complications such as immature lungs, difficulty regulating body temperature, infections, poor feeding and slow weight gain. These complications lead to death or longer, more intense nursery care and sometimes surgery[10], implying that these babies need to be delivered under the care of a skilled health care provider to increase their chances of survival.
However, in Uganda, 1 in 4 deliveries do not occur in a health care setting or under skilled health care personnel. Nevertheless, among babies delivered by skilled health care personnel, only 1 in 2 receive postnatal check-up within two days of delivery[11]. Survival rates for preterm babies are critically reduced if delivery occurs outside the health care facility. Current, local data are crucial to inform priorities and drive scale-up of effective interventions for preterm birth. However, there is paucity of literature about the current trends of premature births and its distribution in Uganda. We described the trends and distribution of preterm births in Uganda between 2015-2019 for advocacy and targeting of interventions.
Methods
We conducted a nationwide descriptive analysis of preterm birth (birth before 37 weeks of gestation) data among newborns from 2015 to 2019 in Uganda using the District Health Information System (DHIS2). According to the World Health Organisation (WHO), a preterm birth is defined as birth that occurs before 37 weeks of gestation[1]
The preterm birth data are routinely generated at health facilities in Outpatients department (OPD) and inpatient department (IPD). The data from OPD and IPD registers are aggregated into a health facility monthly report (paper form) which is initially submitted to health sub-district, then to the district health offices. At district health office, the data from the paper-based reports submitted by health facilities is entered into DHIS2 (web-based reporting) which can be accessed by at Ministry of Health (MoH) and other stakeholders.
We abstracted data from DHIS2 data elements “108-6 Premature baby as condition that requires management (preterm births admissions)” and “105-2.2d Deliveries in unit, (live births)” we disaggregated the data into national, regional, and district levels.
We calculated the incidence rates for preterm births admissions for each level (national, regional and district level), by dividing the total preterm births admitted during the year by the total live births that year and multiplying by 1000. Mean annual incidence rates were obtained by adding annual incidence rates for the five years of study by five.
We drew line graphs by plotting preterm incidence against the period in years to present the trend of incidence rates for national and regional levels and used choropleth maps (generated using district specific incidences of preterm births in Quantum Geographic Information System (QGIS)) to present the distribution of the preterm births admissions at district level. We tested the significance of the trends of preterm births admissions at national and regional levels over the five years of study using logistic regression analysis.
Results
Temporal trends of incidence rate of preterm births admissions, Uganda, 2015-2019
At the national level, there were a total of 2,678 preterm Birth admissions and 914,387 LBs in 2015; 7,508 preterm birth admissions and 959,078 LBs in 2016; 10,561 preterm birth admissions and 1,040,265 LBs in 2017; 13,662 preterm birth admissions and 1,123,279 LB in 2018 and 15,391 preterm birth admissions and 1,176,931 LBs in 2019.
The mean national incidence of preterm birth admissions in Uganda was 9.4/1,000 livebirth. The incidence has steadily been increasing by an average of 45.6% annually from 2015 to 2019 (OR=1.3, CI=1.32-1.33) (Figure 1).
Temporal trend of incidence rate of preterm birth admissions at regional level, Uganda, 2015-2019
Consistent with the national trend, we observed a statistically significant (Table 1) increase in the incidence rates of preterm birth admissions/1,000 LB/year in all the four regions of Uganda, with eastern region being the only region to register a declining incidence between 2018 and 2019. Central region registered the highest mean annual incidence rate of 12 preterm birth admissions/1,000 LB over the 5years, while eastern and northern regions registered the lowest mean incidence rate of 7 preterm birth admissions/1,000 LB in the five years (Figure 2).
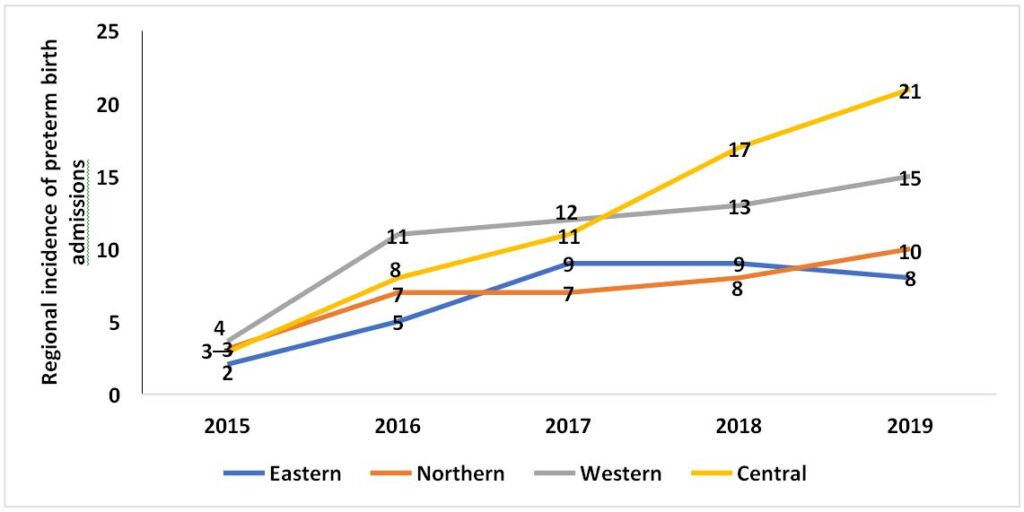
| Region | Odds Ratio | 95% CI | P-Value |
| Central Region 2015/2019 | 1.5 | 1.49-1.52 | 0.000 |
| Eastern Region 2015/2019 | 1.3 | 1.26-1.30 | 0.000 |
| Northern Region 2015/2019 | 1.2 | 1.20-1.24 | 0.000 |
| Western region 2015/2019 | 1.2 | 1.20-1.25 | 0.000 |
Table 1: Significance of the trends of incidence of preterm births admissions at regional level, Uganda, 2015-2019
Spatial distribution of preterm births admission incidence rates at the district level, Uganda, 2015-2019
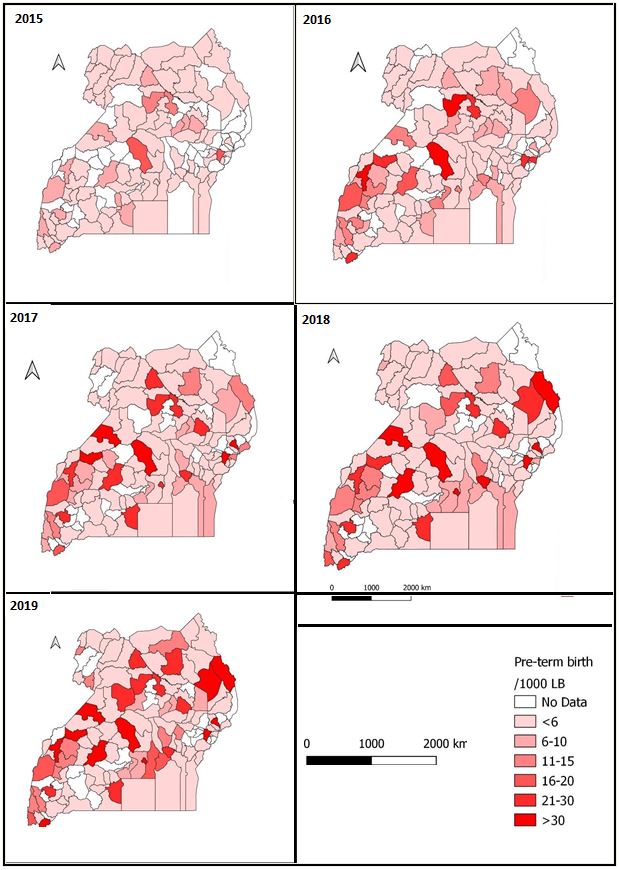
The geographic distribution of preterm birth admissions/1,000 LB in Uganda indicates minimal clustering of high burdened districts in particular regions. Nevertheless, we observe more of the districts with >30 preterm birth admissions/1,000 LB/year in the western and central regions. The years with the highest burden were 2017, 2018, and 2019 (Figure 3).
Discussion
We analysed the trends and geographic distribution of preterm births in Uganda from 2015 to 2019 period. Our study findings show a significant and steadily increasing trend of preterm birth admissions from 2015 and 2019. Similarly, regional trends show a steady and significant increase over the study period. Our study finding is consistent with the findings in over 60 countries in the world with reliable trends that have shown an increasing rate over the past two decades. [3, 4]. The reasons for the increasing trend in Uganda are not clearly understood. However, studies elsewhere have associated the increasing trend to increased use of fertility drugs, twin pregnancies, previous preterm birth, and several other factors [3, 7, 11, 12]. Managing extremely preterm newborns requires well-equipped health facilities and skilled health personnel. The increasing incidence therefore implies a need for the Ministry of Health (MoH) to do an assessment of the current level of preparedness of the health system to manage preterm birth and plan and prepare accordingly in terms of equipment and skills. There is also a need to determine the predictors of preterm birth for better preparedness and management.
Our results show that preterm birth is generally distributed all over the country with minor variations across regions. This result may be explained by the fact that the causes of preterm birth are multifaceted and that about 50% of the preterm birth occur with no known exposures[3]. As such, the preterm birth can occur to anyone-anywhere-anytime. This finding suggests planning a country wide programme such as, equipping and skilling all regional referral hospitals in the country.
Preterm birth as a condition that requires management has been steadily increasing. The increasing number of preterm births requiring management at the facility will require additional space and resources for management. The ministry of health and health implementing partners need to closely monitor the trend of preterm births and forecast future trends to aid planning for space, equipment, and capacity building.
The study depended on secondary data limited to available data variables which may not allow for detailed exploration of the problem including the risk factors for the increasing preterm births. Further studies requiring primary data will need to be conducted for in- depth understanding of the problem.
The incidence of preterm births admissions is on the rise and is distributed across the country. We recommend the MoH to assess the current level of preparedness of the health system to manage preterm birth and to plan and prepare accordingly in terms of equipment and skills. Quality of care improvement projects should be initiated in facilities admitting preterm babies to ensure that the care delivered is of quality and improves chances of survival. We also recommend further studies to determine the predictors of preterm birth for better assessment and identification of mothers at risk of preterm birth for preparedness and timely management.
References
- World Health Organization, Born too soon: the global action report on preterm birth.
- Martin, J.A., et al., Births: final data for 2005. National vital statistics reports, 2007. 56(6): p. 1-103.
- Soon, B.T., The global action report on preterm birth. Geneva: World Health Organization,
- Blencowe, H., et al., National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and The lancet, 2012. 379(9832): p. 2162-2172.
- Beck, S., et al., The worldwide incidence of preterm birth: a systematic review of maternal mortality and Bulletin of the World Health Organization, 2010. 88: p. 31-38.
- Preterm birth factsheet, accessed 30/09/2020, available at https://www.who.int/news-room/fact-sheets/detail/preterm-birth. 19 February 2018.
- About kids Health. Preterm Babies, accessed on 30/09/2020, available at https://www.aboutkidshealth.ca/Article?contentid=1758&language=English.
- Ministry of Health, Situation analysis of newborn health in Uganda: current status and opportunities to improve care and survival. Kampala: Government of Uganda. Save the Children, UNICEF, WHO; 2008. Accesed on 1/10/2020, available at https://www.healthynewbornnetwork.org/hnn-content/uploads/Situation-Analysis-of- Newborn-health-in-Uganda.pdf
- Kananura, R.M., et al., The neonatal mortality and its determinants in rural communities of Eastern Reproductive health, 2016. 13(1): p. 13.
- Ministry of Health, Reproductive Maternal, Newborn and Child Health Sharpened Plan for Uganda, accessed on 30/09/2020, available at http://speed.musph.ac.ug/wp- content/uploads/2015/05/Committing-to-Maternal-and-Child-Survival_A-Promise- pdf November 2013.
- Uganda Bureau of Statistics (UBOS) and ICF, Uganda Demographic and Health Survey 2016. Kampala, Uganda and Rockville, Maryland, USA: UBOS and ICF.
- Wagura, P., et al., Prevalence and factors associated with preterm birth at kenyatta national BMC Pregnancy and Childbirth, 2018. 18(1): p. 107.
Reference this page as below
Job Morukileng1, Wilberforce Mugwanya2, Robert Mutumba2, and Maureen Katusiime1. Incidence of Preterm Births Admissions on the Rise in Uganda: Implications for the Health Care System. Kampala. Uganda National Institute of Public Health. 2021 March 31st. Available from: :https://uniph.go.ug/incidence-of-preterm-births-admissions-on-the-rise-in-uganda-implications-for-the-health-care-system.


Comments are closed.