High level of compliance to handwashing during the early phase of COVID-19 epidemic in Uganda: A nationwide cross-sectional survey
Authors: Richard Migisha1*, Bob Omoda Amodan1, Lilian Bulage1, Elizabeth B. Katana1, Joseph N. Siewe Fodjo2, Robert Colebunders2, Alex Riolexus Ario1, 3, and Rhoda K. Wanyenze4 Affiliations: 1Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda, 2Global Health Institute, University of Antwerp, Doornstraat 331, 2610 Antwerp, Belgium, 3Ministry of Health, Kampala, Uganda, 4School of Public Health, College of Health Sciences, Makerere University, Kampala, Uganda *Correspondence: rmigisha@musph.ac.ug
Summary
The World Health Organization recommends frequent handwashing with soap and water as the cheapest and most essential intervention in preventing the spread of COVID-19. We assessed the level of compliance to handwashing and associated factors among Ugandans in the first two months of the outbreak in the country to inform prevention measures.
We abstracted data from the International Citizen Project (ICP), a cross-sectional nationwide online survey conducted between 16th and 30th April 2020 using a self-administered questionnaire. We collected data on socio-demographic characteristics, the impact of COVID-19 on daily life, adherence to and satisfaction with personal and community preventive measures, and acceptability of these measures. Handwashing compliance was defined as washing hands with soap and water for a minimum of 20 seconds, after touching surfaces, or having been in a public place. We performed multivariable logistic regression to identify factors associated with non-compliance to handwashing.
In total 1,726 participants responded with a mean age (SD) of 36 (±11) years (range: 12-76 years); most (59%) were male, and lived in apartments (84%). Nearly all participants (99.7%) had heard about COVID-19. Among the 1,726 participants assessed for handwashing compliance, 1,662 (96%) complied; only 64 (3.7%; 95%CI: 2.9-4.7%) were non-compliant.
Respondents who stayed in huts/shacks or who were homeless (aOR=6.1, 95%CI: 2.0-18; P=0.002), and those who had not heard about COVID-19 (aOR=13, 95%CI: 2.4-72, P=0.003) were more likely to be non-compliant. Individuals with a high level of satisfaction with handwashing as an appropriate COVID-19 preventive measure were less likely to be non- compliant (aOR=0.26, 95%CI: 0.15-0.45, P<0.001).
The level of compliance to handwashing was very high in the first two months of COVID-19 epidemic in Uganda. Poor housing conditions, low level of awareness about COVID-19, and perceived low level of satisfaction with handwashing as an appropriate COVID-19 preventive measure were associated with non-compliance to handwashing. We recommend continued risk communication and public education especially targeting individuals with poor housing to sustain the high compliance to handwashing. There is need to avail handwashing facilities to individuals with poor housing conditions during the epidemic so as to improve epidemic control.
Introduction
Coronavirus disease 2019 (COVID-19), the respiratory disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) remains a major health threat globally, and has overstretched health systems in many countries. In Uganda, the disease outbreak was first reported on March 21, 2020(1).
The disease may be transmitted from person-to-person through respiratory droplets and contact with infected surfaces. Frequent diligent handwashing with soap and water was recommended as key preventive strategy for COVID-19 in the early phase of the pandemic. Soap breaks down the outer layer of the virus. In addition, the slippery and mechanical motion that arises from handwashing with soap causes the virus to rip off from the skin surface(2). Handwashing has been viewed as an important intervention in the fight against the pandemic for a number of reasons: firstly, soap and water are cheap and readily available; secondly, handwashing is simple to practice by most individuals independently.
Despite the prescribed benefits of proper and frequent handwashing during the pandemic, compliance from individuals across many countries varied owing to the behavioral nature of the intervention(3). Whereas information dissemination and public education are necessary to change behavior, they may not necessarily be sufficient(3). We assessed the level of compliance to handwashing with soap and water, and associated factors, in the first two months of the COVID-19 epidemic in Uganda.
Methods
We abstracted data from the International Citizen Project (ICP), a cross-sectional nationwide online survey that assessed adherence to preventive measures and their impact on the COVID-19 outbreak conducted between 16th and 30th April 2020 using a self-administered questionnaire.
The ICP survey collected data on socio-demographic characteristics; the impact of COVID-19 and associated restrictions on daily life, professional life, and personal well-being; adherence to and satisfaction with personal and community preventive measures; and acceptability of these measures. The questionnaire was circulated via WhatsApp, email, Facebook, and Twitter platforms. Individuals who got the questionnaire were asked to disseminate it further, share it with other persons in their networks.
For this study, we abstracted data on socio-demographic characteristics including age, sex, education, location, marital status, housing conditions, and professional life during the COVID- 19 lock down. During the survey, frequency of handwashing was assessed using a close-ended question with the frequencies specified as a number per day. Additionally, participants were asked to respond (‘yes’ or ‘no’) whether they practiced handwashing after touching surfaces or being in public. Handwashing compliance was defined as, washing hands with soap and water for a minimum of 20 seconds, after touching surfaces, or having been in a public place (4, 5).
In addition, we abstracted data on participants’ awareness of COVID-19, whether they smoked cigarettes or not, whether they had underlying medical conditions (e.g., diabetes, hypertension, HIV), and their level of satisfaction with the level of handwashing as an appropriate COVID19 preventive measure. The level of satisfaction with the handwashing as an appropriate COVID-19 preventive measure was assessed using a 5-item Likert scale (1=very dissatisfied to 5=very satisfied). Participants with scores of 1-3 were considered to have low level of satisfaction, while those with scores 4-5 were considered to have high level of satisfaction(6).
Data were extracted and cleaned using MS Excel 2019, thereafter exported to STATA 13 (Statacorp, College Station. Texas) for analysis. Our outcome of interest was compliance to handwashing with ‘yes’ coded as ‘0’ and ‘no’ coded as ‘1’. We first described participants’ characteristics of the study participants, and compared their distribution among individuals who complied with handwashing and those who did not comply, using Chi-square or two-tailed Fischer’s exact test. We then performed univariable and multivariable logistic regression to identify factors associated with non-compliance to handwashing.
Results
Characteristics of study participants
Overall, 1,726 participants responded with a mean age (SD) of 36 (±11) years (range: 12-76 years). Most of the participants were male (59%), married/living with partners (58%), and lived in apartments (84%). Nearly all participants had ever heard about COVID-19 (99.7%), and were Ugandans (97%) (Table 1). The distribution of sex (P=0.030), nationality (P=0.011), housing conditions (P<0.001), participants who had ever heard about COVID-19 (P=0.033), smoking and level of satisfaction with handwashing as an appropriate COVID-19 preventive measure (P<0.001) was statistically significant between participants who did not comply and those who complied with handwashing (Table 1).
Table 1: Characteristics of study participants by hand washing compliance status
| Hand washing compliance | ||||
| Characteristic | Overall (N=1726) |
No (n=64) |
Yes (n=1662) |
P. No (n=64) |
| Age in years, mean(SD) | 35.9 (±10.6) | 36.0 (±10.6) | 35.5 (±9.7) | 0.069 |
| Sex, n (%) | 0.03 | |||
| Female | 711 (41.2) | 18 (28.1) | 693 (41.7) | |
| Male
Nationality, n (%) |
1015 (58.8) | 46 (71.9) | 969 (58.3) |
0.011 |
| Ugandan | 1679 (97.3) | 59 (92.2) | 1620 (97.5) | |
| Non-Ugandan | 47 (2.7) | 5 (7.8) | 42 (2.5) | |
| Level of education, n (%) | 0.627 | |||
| University graduate | 797 (46.2) | 32 (50.0) | 765 (46.0) | |
| Tertiary (Certificate/Diploma) | 863 (50.0) | 29 (50.0) | 863 (50.2) | |
| Secondary | 63 (3.7) | 3 (4.7) | 60 (3.6) | |
| Primary | 2 (0.1) | 0 (0.0) | 2 (0.1) | |
| None | 1 (0.1) | 0 (0.0) | 1 (0.1) | |
| Marital status, n (%) | 0.773 | |||
| Single | 725 (42.0) | 28 (43.8) | 697 (41.9) | |
| Married/living with partner
Residence, n (%) |
1001 (58.0)
|
36 (56.3)
|
965 (58.1)
|
0.713 |
| Rural/village | 189 (11.0) | 8 (12.5) | 181 (10.9) | |
| Kampala City Centre | 334 (19.4) | 8 (12.5) | 326 (19.6) | |
| Kampala suburb | 329 (19.1) | 14 (21.9) | 315 (19.0) | |
| Other town center | 688 (39.9) | 27 (42.2) | 661 (39.8) | |
| Other town suburb
Housing conditions, n (%) |
186 (10.8)
|
7 (10.9)
|
179 (10.8)
|
<0.001 |
| Apartment | 1444 (83.7) | 46 (71.9) | 1398 (84.1) | |
| Room | 259 (15.0) | 13 (20.3) | 246 (14.8) | |
| Hut/shack/homeless | 23 (1.3) | 5 (7.8) | 18 (1.1) | |
| Ever heard about COVID-19 epidemic, n (%) | 0.001 | |||
| Yes | 1720 (99.7) | 61 (95.3) | 1569 (99.8) | |
| No | 6 (0.4) | 3 (4.7) | 3 (0.2) | |
| Occupation, n (%) | 0.206 | |||
| Jobless | 124 (7.2) | 4 (6.3) | 120 (7.2) | |
| Self-employed | 284 (16.5) | 13 (20.3) | 271 (16.3) | |
| Student | 209 (12.1) | 12 (18.8) | 197 (11.8) | |
| Private employed | 731 (42.4) | 19 (29.7) | 712 (42.8) | |
| Government employed | 378 (21.9) | 16 (25.0) | 362 (21.8) | |
| Currently smoking, n (%) | 0.033 | |||
| No | 1686 (97.7) | 60 (93.8) | 1626 (97.8) | |
| Yes | 40 (2.3) | 4 (6.3) | 36 (2.2) | |
| Underlying medical condition, n (%) | 0.528 | |||
| No | 1426 (82.6) | 51 (79.7) | 1372 (82.7) | |
| Yes | 300 (17.4) | 13 (20.3) | 287 (17.3) | |
| Level of satisfaction with hand washing as a preventive measure, n (%) | <0.001 | |||
| Low | 1511 (87.5) | 42 (65.6) | 1469 (88.4) | |
| High | 215 (12.5) | 22 (34.4) | 193 (11.6) | |
Compliance to handwashing and frequency during the early phase of COVID-19 epidemic in Uganda
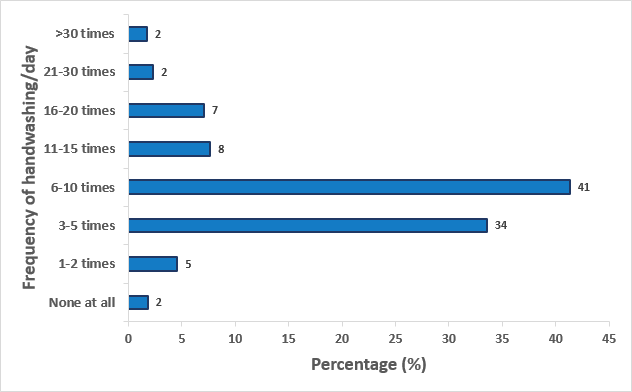
Among the 1,726 participants assessed for compliance to handwashing with soap and water, 1662 (96%) complied; the remaining 64 (3.7%; 95%CI: 2.9-4.7%) were not compliant. Of the total 1,726 participants, most washed their hands 6-10 times/day (41%), followed by 3-5 times/day (34%); Only 31 participants (1.8%) did not wash their hands at all; 30 participants (1.7%) washed their hands more than 30 times/day (Figure 1).
Factors associated with non-compliance to handwashing during the early phase of COVID-19 epidemic in Uganda
In multivariable analysis, individuals who had significantly higher odds of non-compliance were those who stayed in huts/shacks or who were homeless (aOR=6.1, 95%CI: 2.0-18; P=0.002) and individuals who had not heard of COVID-19 (aOR=13, 95%CO: 2.4-72, P=0.003). Individuals with high level of satisfaction with handwashing as an appropriate COVID19 preventive measure were less likely to be non-compliant to handwashing (aOR=0.26, 95%CI: 0.15-0.45, P<0.001).
Discussion
We assessed the level of compliance to handwashing with soap and water and associated factors in the first two months of the COVID-19 outbreak in Uganda. Nearly all (96%) of the respondents were compliant to handwashing; poor housing conditions (being homeless, or staying in huts/shacks) and not being aware of COVID-19 were associated with non-compliance. Respondents who were highly satisfied with handwashing as an appropriate COVID-19 prevention measure were less likely to be non-compliant.
A recent demographic and health survey in Uganda, prior to the COVID-19 pandemic, reported handwashing compliance of 44% among household members whose households had soap and water available(7). The high level of compliance to handwashing with soap and water observed in this study emphasizes the fact that COVID-19 could have reinforced handwashing behavior(8). This may be attributed to the extensive messaging on different media platforms, emphasizing the importance of handwashing in the pandemic. Consistent with our findings, a study among Polish adolescents also reported a significant improvement in handwashing compliance with soap and water during the COVID-19 pandemic(9). Sustaining the high level of compliance to handwashing in Uganda will require sustained health promotion efforts aimed at improving hygiene, through mass media and social media in the different phases of the epidemic and in the post-COVID-19 era.
Our findings demonstrated that individuals who were homeless or staying in poor housing conditions were more likely to be non-compliant to handwashing with soap and water. Poor housing conditions is an indicator of poor socioeconomic status which is often coupled with water insecurity; under these circumstances of water scarcity, the scarce water is prioritized for other domestic needs such as cooking(10). The water insecurity most common in poor housing conditions in low-income countries may undermine the COVID-19 response efforts in the developing countries, and make water-insecure areas (e.g., slums) epicenters for disease transmission(10). We therefore recommend that designated handwashing points be availed in areas with poor housing conditions so that handwashing with soap and water is more easily accessible to all Ugandans given the wide health benefits of handwashing.
Our study revealed that respondents who had never heard about COVID-19 were more likely to be non-compliant to handwashing with soap and water. Persons unaware of a disease always have low knowledge levels about the disease; the low knowledge ultimately influences the perception of disease severity. According to the Health Belief Model (HBM), persons with perceived severity and susceptibility of being afflicted with life-threatening diseases including COVID-19 are more likely to practice personal preventive measures such as handwashing and facemasks use(11). Although awareness about COVID-19 was nearly universal among our study population, the fact that respondents who were not aware about the disease were less likely to practice handwashing, calls for the need to continue sensitization and risk communication among Ugandans. Similarly, respondents who were not highly satisfied with handwashing as an appropriate COVID19 preventive measure were less likely to be compliant. This is consistent with previous findings from research about the influence of perception of social campaigns by the general public on individual preventive measures(12). It is believed that the attitude towards public health measures practiced in a given society may influence one’s behavior and readiness to accept such interventions(12).
Although our study generated valuable nationwide data on handwashing frequency and adherence to handwashing with soap and water by the Ugandan population, it is important to mention the study limitations. First, the study relied on self-report of handwashing behavior, making it susceptible to social-desirability bias. However, this was minimized by making the questionnaire self-administered. Second, data were collected online via internet; individuals who had no access to internet connection were unable to participate in our study. Therefore, our study sample is not a good representation of the general population in Uganda, and may have overestimated the prevalence of handwashing compliance.
Conclusions and recommendations
The level of compliance to handwashing with soap and water was much higher in the Ugandan population in the first two months of COVID-19 epidemic, compared to ‘normal times’. Poor housing conditions, low level of awareness about COVID-19, and perceived level of satisfaction with handwashing by the public were associated with non-compliance to handwashing. We recommend continued risk communication and public education to sustain the high compliance to handwashing. There is need to avail designated handwashing points to individuals with poor housing conditions during the epidemic so as to improve epidemic control.
Disclaimer
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the Makerere University School of Public Health, the Ministry of Health Uganda, and Global Health Institute, University of Antwerp.
References
- Migisha R, Kwesiga B, Mirembe BB, Amanya G, Kabwama SN, Kadobera D, et al. Early cases of SARS-CoV-2 infection in Uganda: epidemiology and lessons learned from risk-based testing approaches– March-April Globalization and Health. 2020;16(1):1-9.
- Roser M, Ritchie H, Ortiz-Ospina E, Hasell J. Coronavirus pandemic (COVID-19). Our world in 2020.
- Lunn PD, Belton CA, Lavin C, McGowan FP, Timmons S, Robertson Using Behavioral Science to help fight the Coronavirus. Journal of Behavioral Public Administration. 2020;3(1).
- Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Medica: Atenei 2020;91(1):157.
- Organization WH. Hand hygiene: why, how & when. World Health Organization online resource, retrieved 2009;10:2015.
- Amodan BO, Bulage L, Katana E, Ario AR, Fodjo JNS, Colebunders R, et al. Level and Determinants of Adherence to COVID-19 Preventive Measures in the First Stage of the Outbreak in International journal of environmental research and public health. 2020;17(23):8810.
- Statistics UBo. Uganda demographic and health survey 2016. UBOS and ICF Kampala, Uganda and Rockville, Maryland, USA; 2018.
- Alzyood M, Jackson D, Aveyard H, Brooke COVID‐19 reinforces the importance of handwashing. Wiley Online Library; 2020.
- Głąbska D, Skolmowska D, Guzek D. Population-based study of the influence of the COVID-19 pandemic on hand hygiene behaviors—Polish adolescents’ COVID-19 experience (PLACE-19) study. 2020;12(12):4930.
- Stoler J, Jepson WE, Wutich A. Beyond handwashing: Water insecurity undermines COVID-19 response in developing Journal of Global Health. 2020;10(1).
- Sim SW, Moey KSP, Tan NC. The use of facemasks to prevent respiratory infection: a literature review in the context of the Health Belief Singapore medical journal. 2014;55(3):160.
- Duplaga M. Perception of the Effectiveness of Health-Related Campaigns among the Adult Population: An Analysis of Determinants. International journal of environmental research and public 2019;16(5):791.
Reference this page as below
Richard Migisha1*, Bob Omoda Amodan1, Lilian Bulage1, Elizabeth B. Katana1, Joseph N. Siewe Fodjo2, Robert Colebunders2, Alex Riolexus Ario1, 3, and Rhoda K. Wanyenze4. High level of compliance to handwashing during the early phase of COVID-19 epidemic in Uganda: A nationwide cross-sectional survey. Kampala. Uganda National Institute of Public Health. 2021 March 31st. Available from:https://uniph.go.ug/high-level-of-compliance-to-handwashing-during-the-early-phase-of-covid-19-epidemic-in-uganda-a-nationwide-cross-sectional-survey.

