Highlights of the COVID-19 outbreak in Uganda, March to June 2020
Quarterly Epidemiological Bulletin : April to June 2020 Volume 5 Issue 2 Article No. 1
Authors: Maureen Nabatanzi1, Daniel Eurien1, Godfrey Nsereko1, Benon Kwesiga1, Daniel Kadobera, Bernard Lubwama2, Alex Riolexus Ario1, Julie Harris3
Affiliations;
1Uganda Public Health Fellowship Program, Kampala, Uganda
2Integrated Epidemiology, Surveillance and Public Health Emergencies Department, Ministry of Health, Uganda
3US Centers for Disease Control and Prevention, Kampala, Uganda
Summary
On 21 March 2020, Uganda’s Ministry of Health (MoH) confirmed the country’s first case of COVID-19. The initial response included: institutional quarantine of suspected cases, contact tracing and follow up, and stepping up efforts in alert verification and testing. To strengthen social distancing recommendations and reduce movement of people, public transportation was banned and use of private cars limited to a maximum carriage of three persons. Despite these interventions, Uganda registered 696 confirmed cases, including 20 health workers by 13 June, and 165 local infections by 5 June 2020. The local infections were in 30 districts. We recommend strengthening of COVID-19 surveillance in all districts of Uganda.
Highlights of the COVID-19 outbreak in Uganda
On 21 March 2020, Uganda’s Ministry of Health (MoH) confirmed the country’s first case of COVID-19. The index case-patient had returned from a high-risk country and was identified through routine screening at Entebbe International Airport. Subsequently, most of the initial cases were among travelers from high risk countries and truck drivers. However, there was a shift in the confirmed cases to trans-border truck drivers and their contacts in and around the country’s points of entry (PoEs).
As of 12 June 2020, 696 confirmed cases had been reported (Figure 1). There was a surge in cases in May. Between 30 May and 5 June, 264 new COVID-19 cases were registered compared to the 156 from 23rd to 29th May. At 69%, this was the highest weekly increase in cases the country had had since the outbreak begun. Of the 264 cases confirmed between 30 May and 5 June week, 120 (45%) were trans-border truck drivers.
As of 5 June, a total of 20 health care workers tested positive for COVID-19, 16 of them were identified from health facilities and four were among the response teams. There is evidence of increasing local infections. By 5 June, Uganda had 165 known local infections in 30 districts. The most affected districts were: Amuru (36, 22%), Kampala (21, 13%) and Kyotera (20, 12%).
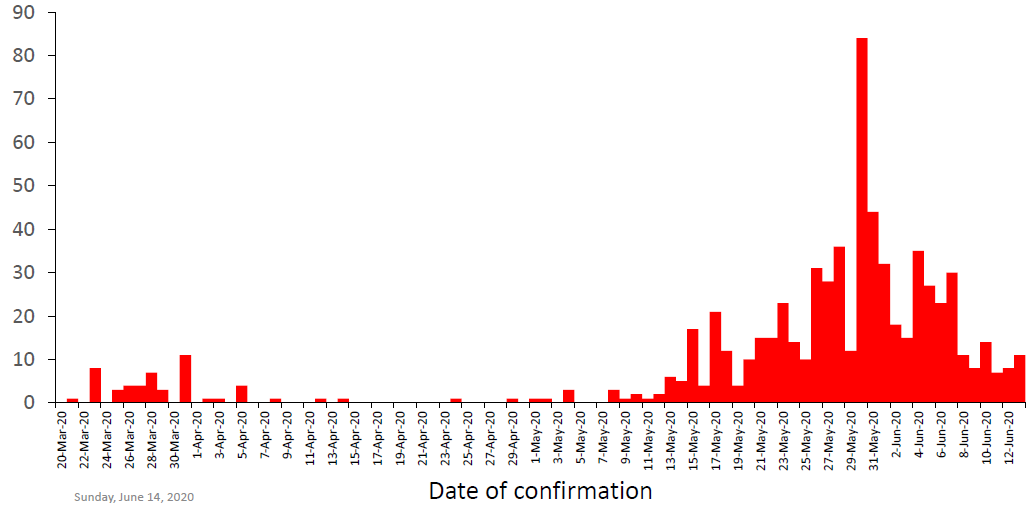
Figure 1: Curve of COVID-19 cases by date of confirmation, Uganda, 20 March-13 June 2020
Public health interventions
The initial response to the outbreak included: institutional quarantine of suspected cases, contact tracing and follow up, and stepping up efforts in alert verification and testing. To strengthen social distancing recommendations and reduce movement of people, public transportation was banned and use of private cars limited to a maximum carriage of three persons. Private transport for non-essential workers was suspended and passengers coming into Uganda by air, land or water were stopped. Pedestrians from neighbouring countries were also prohibited from entry into the country. In addition, public gatherings in bars, churches, theatres were banned and schools and universities were closed (Figure 2).
Response activities
The Ministry of Health strengthened screening and laboratory sample testing for COVID-19. Mandatory testing included: all persons crossing into Uganda at various PoEs, contacts and suspected cases. As of 5 June, a total of 131,714 samples had been collected and tested for COVID-19. Tracing and follow up of contacts of confirmed cases enabled the prompt identification, isolation and testing of exposed persons. As of 5 June, the cumulative number of contacts listed were 6,493, a total of 5,376 (75%) of the listed contacts had completed the 14 days of follow-up while 1,117 (25%) contacts were still under follow up. Institutional quarantine was used to prevent further transmission of COVID-19 from exposed persons to unexposed community members. Between 20 March and 5 June, 4,119 persons were quarantined at 68 quarantine centres for 14 days. Of these 4,119, 125 (3%) tested positive for COVID-19. Confirmed case-patients were managed at Uganda’s 16 regional referral hospitals and Mulago national referral hospital. As of 13 June, Uganda had registered 240 recoveries out of the 696 confirmed cases (34%) and no deaths.
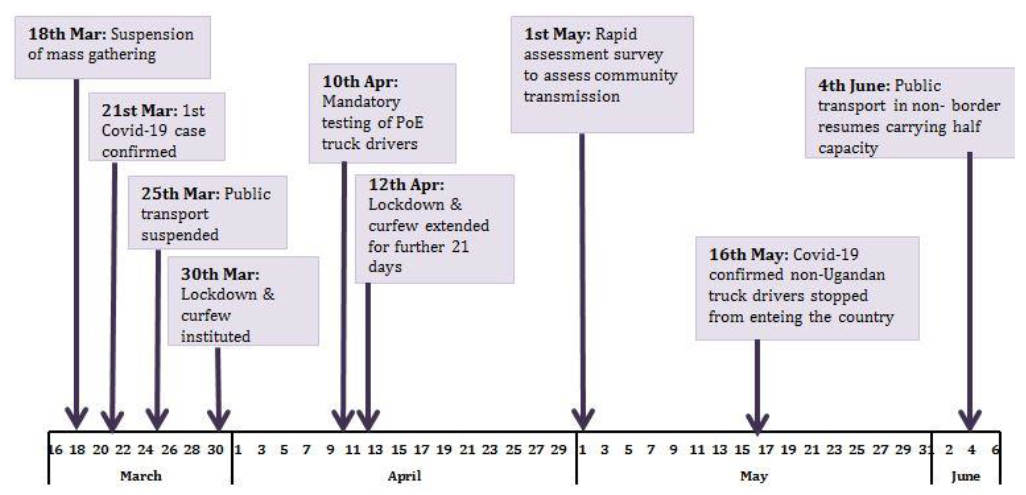
Figure 2: Chronology of COVID-19 public health interventions in Uganda, March-June 2020
Conclusion and recommendations
The COVID-19 outbreak in Uganda is shifting from predominantly imported to more local infections. There is need for case investigations to enable immediate identification and categorization of hot spots for effective response. The increase in detected local infections also implies that all districts must heighten COVID-19 surveillance. Districts with high risk of local transmission should be supported in strengthening surveillance.
References
- Uganda COVID-19 Analytical Report Week 30th May to 5th June 2020
- Uganda COVID-19 Surveillance Update, 14th June 2020
- Uganda COVID-19 Situation Report 116, 12th June 2020
Read and Download pdf Article below;


Comments are closed.