Evaluation of the Surveillance System in Bidibidi Refugee Settlement, Yumbe District, Uganda, Mar 2017
Authors: Jimmy Ogwal1, Susan Kizito1, Benon Kwesiga1, Alex Riolexus Ario1; Affiliation: 1Uganda Public Health Fellowship Program
Summary
Influx of refugees from Southern has stressed a fragile public health system leading to poor sanitation/ hygiene, insufficient safe drinking water, and an increased risk of disease outbreaks and malnutrition. We evaluated the disease surveillance system in Bidibidi refugee settlement in Yumbe District to identify strengths, weaknesses, and recommend areas for improvement. We evaluated the surveillance system attributes using the updated CDC guidelines for public health surveillance. Only 4% of health workers were trained on Integrated Disease Surveil- lance and Response (IDRS) guidelines by Ministry of Health with 12% of health facilities having treatment guidelines. There were 64 suspected cases of cholera but only 4 were notified for investigation as per Integrated Disease Surveillance and Response (IDRS) guidelines. Positive predicative value was 50%. We found weak surveil- lance system in terms of flexibility, acceptability, simplicity, sensitivity, timeliness and poor completeness. We recommended IDSR trainings for the DRRT; availing of standard MoH surveillance tools and strengthening of case investigation and reporting.
Introduction
Fresh political clashes in South Sudan in June 2016 led to a large influx of refugees to Uganda through various en- try points in Northern Uganda. According to UNHCR, at the peak of the influx, approximately 2218 refugees arrived daily(6). In response to the growing need, Uganda’s Office of the Prime Minister (OPM) and the UNHCR identified several locations for additional refugee camps and one of these was Bidibidi settlement camp located in the Yumbe District in Northern Uganda with a capacity of 180,000 refugees. Influx of refugees from Southern has stressed a fragile public health system leading to poor sanitation/hygiene, insufficient safe drinking water, and an increased risk of disease out- breaks and malnutrition. Although international standards for establishment of health surveillance in an emergency setting are available, we needed to assess the existing surveillance system, identify gaps and recommend areas of improvement.
Method
We conducted the study in Bidibidi settlement camp located in the Yumbe District, in the West Nile region of Northern Uganda. We evaluated the surveillance system attributes using CDC guidelines for public health surveillance(1). 24 clusters (Villages) were selected from the 5 zones using sampling proportionate to size.
All Village Health Teams from the selected clusters and health facility in-charges were interviewed using structured questionnaires. Facility registers and reports were reviewed for availability and quality.
Results
The available system does not provide the opportunity for disease notification at community level, confirmation and response to outbreak as the health facilities do not report their data to the national DHIS2.
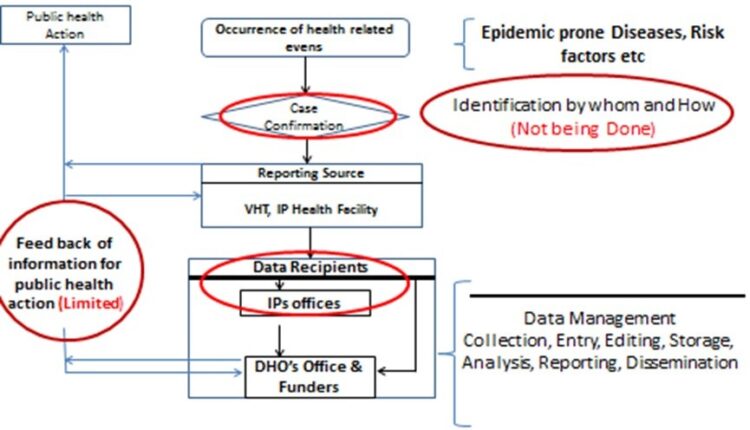
Simplicity and acceptability: There are multiple reporting tools being used for reporting. UNHCR and its implementing partners used tools that were different from the standard IDSR tools approved by Ministry of Health. This affected the simplicity and acceptability of the surveillance since there were multiple reporting tools and structures being used.
Flexibility: Given that different tools were being used by different health facilities for data capture and reporting with different variables, the system was not flexible. Age grouping was different across the facilities and from that of Ministry of Health recommended tools.
Sensitivity: The system does not fit the WHO four steps of integrated disease surveillance and response of detection, reporting, investigation and public health actions. The diseases or conditions were being diagnosed without reference to the IDSR case definitions.
Representativeness: The analysis of the data was not being done at the facility level and occurrences of the diseases of epidemic nature at the community level were not being reported. The aggregation of conditions by location and time was not possible. This left the representativeness of the system on the distribution of disease inadequate.
Predictive value positive: This emphasizes the confirmation of cases reported through the surveillance system. The positive predicable value (PPV) for cholera is 50% and 5 cases of measles where suspected but none was reported either to Yumbe District or the DHIS2. The case fertility rate for cholera was 31 per 1000 people.
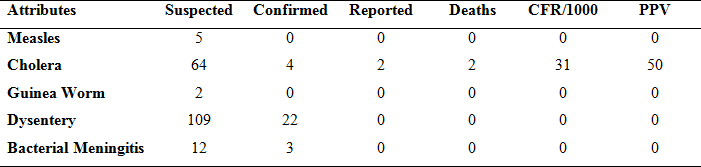
Quality: In the camp facilities, 16% respondents were trained in outbreak investigations. 84% of the health facilities do not have both clinical and integrated disease surveillance and response guidelines. 75% do not have the required laboratory supplies necessary for sam- ple taking and transportation.
Timeliness: Health care providers in the settlement (76%) send their data first to their head offices (partner agencies) before submission to the district health office. For diseases which are supposed to be reported immediately, like cholera and measles for public health action, it takes more than two days to reach Yumbe district health office.
Discussion
The available surveillance system in Bidibidi settlement camp demonstrated inability to detect, control, prevent and response to public health emergencies. A useful surveillance system contributes to the prevention and control of adverse health events especially in emergency settings with over stretched health and social services. Increased sensitivity may afford a greater opportunity for identifying epidemics and under- standing the natural course of health events in a community. Similarly improved timeliness allows control and prevention activities to be initiated early.
Having a representative surveillance system will better characterize the epidemiologic characteristics of a health event in a defined population(12). In Bidibidi settlement camp, more emphasis has been put on the care and treatment of events by the various implementing partners with very limited emphasis on surveillance. As a result many out- breaks were never noticed such the most recent measles outbreak where no case was reported but captured in the registers.
Conclusion
The surveillance system in Bidibidi settlement camp is not in line with the WHO standards which are being used by Ministry of Health. It does not provide room for detection, prevention and control of public emergencies. The system was found not to be simple, insensitive and with limited flexibility to achieve the surveillance goals.
We recommend that the surveillance system in the camp should be harmonized with that of ministry of health through proper coordination to facilitate timely detection, reporting and investigation of public health events.


Comments are closed.