Epidemiological Characteristics and Trend of Suspected Measles, Uganda, 2011 – 2018
Author: Sandra Nabatanzi1*, Benon Kwesiga1, Issa Makumbi2, Lilian Bulage1, Alex R. Ario1 | Affiliations: 1Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda 2Public Health Emergency Operations Center, Ministry of Health, Kampala, Uganda
Summary
Uganda is working towards measles elimination by 2020, measles elimination is the absence of endemic measles transmission or no more cases of measles caused by indigenous virus in a defined geographical area, for ≥12 months in the presence of a well-performing surveillance system. Though the WHO recommends measles vaccination coverage of 95%, Uganda’s coverage was only 80% in 2016, and the country continues to experience measles outbreaks. We characterised suspected measles cases in Uganda during 2011- 2018 to identify trends and inform programming. We analysed secondary data on suspected measles cases obtained from the District Health Information System (DHIS2), from 6455-2018. A suspected measles case was any person with fever, maculopapular generalized rash, and cough, coryza, or conjunctivitis, or any per- son in whom a clinician suspected measles. We calculated the overall incidence of suspected measles during the study period and disaggregated it by year, age-group, sex, and region. We evaluated trends using logistic regression. The overall incidence of measles was 1.3/1,000. Females (1.1/1,000) and males (1.0/1,000) were similarly affected. Children <5 years (9.2/1,000) were more affected than persons ≥5 years (0.6/1,000). Overall, Kampala region was the most affected during the study period, with a cumulative incidence of 27/1,000; Karamoja region was least affected (2.3/1,000). Overall, incidence of suspected measles declined 70% (p<0.0001) from 2012-2013, and increased gradually over the subsequent years. Trend analysis identified 24% (p<0.0001) overall increase during the study period. Suspected measles incidence increased in Uganda during the last decade, with Kampala region and children <5 years being the most affected. Uganda is off track for measles elimination. We recommend intensification of regular mass measles-rubella vaccination and further studies to investigate factors affecting low vaccination rates and further identify hotspots for targeted interventions.
Introduction
Measles is a highly contagious viral infectious disease that belongs to the family of paramyxovirus that is spread through air by droplets and direct contact with nasal or throat secretions of an infected person (1). Measles is the leading cause of vaccine-preventable childhood deaths globally. According to World Health Organization (WHO), measles deaths decreased by 84% between 2000 and 2016. In 2016, 7 million people were infected with measles from developing countries in Africa and Asia (2). The WHO recommends 95% measles coverage vaccination in order to interrupt transmission and prevent outbreaks. The Measles vaccine is known to be highly effective, safe, and relatively cost effective (3, 4). In 2016, the measles vaccination coverage in Uganda was 80% (3). In 2011, the African region adopted the measles elimination goal to be reached by 2020. The targets set for measles elimination were; measles incidence of less than 1 case per million population at national level, at least 95%. At least 95% measles immunization coverage at national level and in all districts; measles immunization coverage at national level and in all districts, minimum 95% coverage in all scheduled measles SIAs and outbreak response immunization activities, at least 80% of districts investigating one or more suspected measles cases within a year and non-measles febrile rash illness rate of at least 2 per 100,000 population at National level (6).The activities for measles control and elimination include Routine immunization (RI), supplemental immunization activities (SIA), management of cases, outbreak response and surveillance (7). In Uganda, it is the mandate of Uganda National Expanded Program on Immunization (UNEPI), Ministry of Health’s to conduct routine immunization of children. The Measles Vaccine is administered at 9 months and mass Measles vaccination campaigns are carried out every 3 years nationwide. Measles surveillance in Uganda is done through the Integrated disease surveillance and response (IDSR) platform. Measles is one of the priority diseases reported from health facilities in the country. Maintaining adequate measles vaccination coverage in Uganda is still a challenge leading to several measles outbreaks in the country. In order to inform current progress towards the 2020 elimination goal, we characterised suspected measles cases in Uganda during 2011-2018 to identify trends and inform programming.
Methods
We analyzed secondary data on suspected measles cases obtained from the District Health Information System (DHIS2), from 2011-2018. A suspected measles case was any person with fever, maculopapular generalized rash, and cough, coryza, or conjunctivitis, or any person in whom a clinician suspected measles. We calculated the overall incidence of suspected measles during the study period and disaggregated it by year, age-group, sex, and region. We evaluated trends using logistic regression.
Results From 2011 to 2018, a total of 294,770 patients with suspected measles were diagnosed across 7,155 health facilities in Uganda. The overall incidence of measles was 1.3/1,000. Females (Incidence=1.1/1,000) and males (Incidence=1.0/1,000) were similarly affected during the study period. Children under 5 years (9.2/1,000) were more affected than persons above 5 years (0.6/1,000).
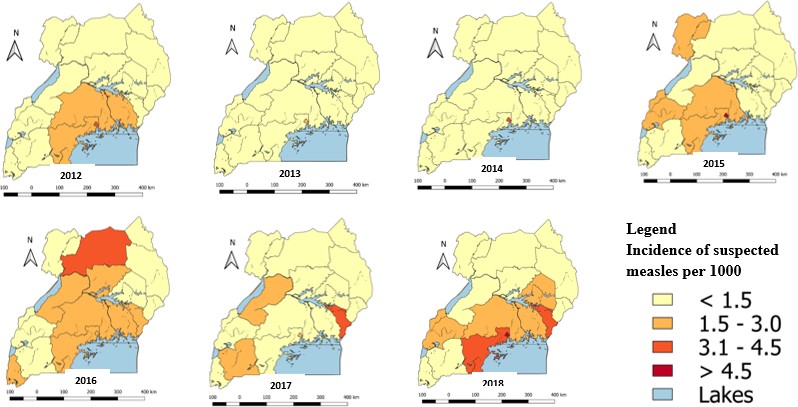
Overall, Kampala region was the most affected out of the 15 regions during the study period, with a cumulative incidence of 27/1,000. Karamoja region was least affected (2.3/1,000). However, during 2016, Acholi region (3.3/1,000) was the most affected followed by Kampala (2.6/1,000). During 2017, Bukedi region (3.0/1,000) was the most affected, followed by Kampala (2.6/1,000) (Figure 1).
Discussion
Surveillance data between January 2011 and December 2018 showed an overall gradual increase in suspected measles incidence in Uganda. A sharp decline was recorded in 2013 in all regions. Kampala was the most affected and females were similarly affected compared to Overall, incidence of suspected measles declined by 70% (p<0.0001) from 2012-2013, and increased gradually over the subsequent years. Trend analysis identified 24% (p<0.0001) overall increase during the study period (Figure 2).

males. The gradual increase in suspected measles in Uganda suggests gaps in vaccination coverage which facilitates continued transmission. In 2012, a mass measles vaccination was conducted country wide which could explain the drastic decline in suspected measles cases in 2013. However, the benefits of the vaccination lasted for a short period of time which was followed by surges in the subsequent years. Following the mass measles vaccination campaign in 1999-2000 in Uganda, a 39% reduction in measles cases was noted and the impact lasted 15-22 months(9). Similarly in West Africa and South Africa the numbers of measles cases reduced 6 months after mass measles vaccination and 12 months following the campaigns, however an in- crease in cases was noticed at 21 months (2). Mass campaigns in Uganda are carried out every 5 years, the number of susceptible individuals builds up quickly hence transmission is sustained. The Ministry of Health conducted the last mass measles- rubella vaccination in October 2019, in order to maintain high and sustained coverage in the community,
we recommend intensification of routine vaccination (3). The most affected age-group was < 5 which is consistent with a study carried out in Kamwenge District, Uganda during a measles outbreak which found higher attack rates of 13% among 0-5 year children (4). In South Africa, measles incidence was highest among infants (61/10,000) and second highest among children 1 to 4 years (7.3/10,000) (10). We recommend catch up and follow up mass vaccination campaigns yearly and 3-5 years respectively to interrupt transmission.
Kampala was the most affected region during the study period. Kampala is an urban area and a capital City of Uganda with a great deal of trade and travel. The City has an area 189 km2 with an estimated population of 1,650,000 in 2019 with a 4% growth rate. High population density was associated with high measles incidence in South Africa. Geographical clustering of unvaccinated children in Texas, United Sates was associated with spread of measles (11). Kampala being the capital city, there is close proximity of people travelling to and from other areas including neighbouring countries. The immigration of susceptible individuals may also lead to outbreaks. The cover- age of measles in Kampala is 83%, (3). Areas with high population density need focused and more frequent follow on vaccination due to the quick build-up of susceptible cases (10).
Limitations and strengths
Data analyzed for this study was collected from a passive surveillance system hence the results are subject to reporting biases like under reporting caused by delays and failure to submit monthly reports by the health facilities. Some patients do not seek care at the health facilities leading to loss in reporting numbers hence possible underestimation of the burden of measles.
Conclusion
Suspected measles incidence increased in Uganda during the last decade, with Kampala region and children <5 years being the most affected. Uganda is off track for measles elimination. Measles elimination means absence of endemic measles transmission or no more cases of measles caused by indigenous virus in a defined geographical area, for ≥12 months in the presence of a well-performing surveillance system (12). We recommend intensification of regular mass measles- rubella vaccination and further studies to investigate factors affecting low vaccination rates and further identify hotspots for targeted interventions.
References
1. World Health Organization. WHO | Measles [Internet]. WHO. [cited 2019 Aug 9]. Available from: http://www.who.int/ immunization/diseases/measles/en/
2. World Health Organization. Measles surveillance data [Internet]. www.who.int. [cited 2019 Aug 8]. Available from: http:// www.who.int/immunization/newsroom/measles-data-2019/en/
3. Uganda Bureau of Statistics Kampala, Uganda. Uganda Demo- graphic Health Survey 2019 [Internet]. Available from: https:// www.ubos.org/onlinefiles/uploads/ubos/pdf%20documents/ Uganda_DHS_2016_KIR.pdf
4. Fine PEM. Herd Immunity: History, Theory, Practice. Epidemiol Rev. 1993 Jan 1;15(2):265–302.
5. Gay NJ. The theory of measles elimination: implications for the design of elimination strategies. J Infect Dis. 2004 May 1;189 Suppl 1:S27-35.
6. Masresha BG, Fall A, Luce R, Shibeshi M, Kaiser R, Dosseh A, et al. Measles elimination in the African Region: Progress and chal- lenges. Afr Health Monit. 2015 Mar 1;
7. Gastañaduy PA, Banerjee E, DeBolt C, Bravo-Alcántara P, Sa- mad SA, Pastor D, et al. Public health responses during measles out- breaks in elimination settings: Strategies and challenges. Hum Vaccines Immunother. 2018 Jul 11;14(9):2222–38.
8. Ministry of Health, Uganda. National Technical Guidelines for Intergrated Disease Surveillance and Response [Internet]. [cited 2019 Aug 9]. Available from: https://health.go.ug/
9. Nanyunja M, Lewis RF, Makumbi I, Seruyange R, Kabwongera E, Mugyenyi P, et al. Impact of mass measles campaigns among chil- dren less than 5 years old in Uganda. J Infect Dis. 2003 May 15;187 Suppl 1:S63-68.
10. WHO | Identifying high-risk areas for sporadic measles out- breaks: lessons from South Africa [Internet]. [cited 2019 Oct 16]. Available from: https://www.who.int/bulletin/volumes/91/3/12- 110726/en/
11. Sinclair DR, Grefenstette JJ, Krauland MG, Galloway DD, Frankeny RJ, Travis C, et al. Forecasted Size of Measles Outbreaks Associated With Vaccination Exemptions for Schoolchildren. JAMA Netw Open. 2019 Aug 21;2(8):e199768–e199768.
12. Vaidya SR. Commitment of measles elimination by 2020: Challenges in India. Indian Pediatr. 2015 Feb;52(2):103–6.


Comments are closed.