Determinants of resilience at the workplace among healthcare workers at the epicenter of the Sudan Ebola Outbreak Response, Uganda, 2022
Authors: Robert Zavuga*1, Peter Chris Kawungezi1, Brian Agaba1, Richard Migisha1, Daniel Kadobera1, Benon Kwesiga1, Peter Edward Okello1, Lilian Bulage1, Freda Loy Aceng2, Emmanuel Batiibwe3, Alex Riolexus Ario1 Institutional affiliations: 1Uganda Public Health Fellowship Program-Uganda, National Institute of Public Health, Kampala, Uganda, 2Department of Integrated Epidemiology, Surveillance and Public Health Emergencies, Ministry of Health, Kampala, Uganda, 3Mubende Regional Referral Hospital, Mubende, Uganda *Correspondence: rzavuga@musph.ac.ug, +256772655723
Summary
Background: Resilience is an individual’s ability to cope with stress after an adverse event. On September 20, 2022, the Uganda Ministry of Health (MoH) declared an outbreak of Sudan ebolavirus (SUVD). As a result, Healthcare workers (HCWs) at the epicenter of the SUVD outbreak response in Mubende and Kassanda districts may have been exposed to several workplace stressors. We assessed the level and determinants of resilience at the workplace amongst HCWs at the epicenter of the SUVD outbreak in Uganda.
Methods: We conducted a cross-sectional survey amongst 400 HCWs who were present from September 20, 2022─January 23, 2023 in the three health facilities that provided care to SUVD case-patients in Mubende District (Mubende Regional Referral Hospital and Madudu Health Center III) and Kassanda District (Kikandwa Health Center III). We defined resilience as the HCW’s ability to cope with workplace stress during the SUVD outbreak. We collected data using a structured questionnaire with variables on social demographic and occupation characteristics, risk perception towards SUVD, and level of resilience. We used the Connor-Davidson Resilience Scale (CD-RISC-10) to measure resilience, which was dichotomized into ‘not resilient’ (score of 1-29) and ‘resilient’ (score of 30-40). A 4-point Likert-type scale was used to assess risk perception towards SUVD, comprising of 11 statements of concern. We used logistic regression to identify factors associated with resilience
Results: The 400 HCWs interviewed had a mean age of 35.3 (range: 20-58) years; 222 (56%) were male and had a median work experience of 8 years (range:1-38). 110 (27.5%) of the HCWs were support staff, 72(18%) were nurses, and 344 (86%) worked >40 hours per week. Majority of HCWs 307(77%) were not resilient. The commonest concerns arising from HCWs were: fear of contracting SUVD 356 (89%) and stigma at the workplace 356 (89%) and there was no difference in resilience between respondents with one concern and those with more than one concern. Resilience was associated with age >40 years (adjusted odds ratio (AOR)=2.1; CI: 1.3-3.5), work experience of >10 years (AOR=2.2; CI: 1.1-4.7), working for >40 hours per week (AOR 6.8 CI: 2.1-22.7), living >10km away from the workplace (AOR 4.5 CI: 1.3-15.6), working as a permanent staff (AOR 3.6 CI: 1.3-9.7), and receiving Ebola specific counselling services (AOR 3.3 CI: 1.7-6.5).
Conclusion: Most HCWs who worked at the epicentre of the SUVD outbreak in Uganda were not resilient to stress. Resilience was associated with older age and more work experience, working for long hours, living further away from the workplace, being a permanent staff member, and receiving counselling services. HCWS were mainly concerned about the risk of contracting SUVD and stigma at the workplace. To address these issues, the MoH may consider adopting workplace policies aimed at addressing HCWs’ concerns, measures that reduce risk perception, and provision of psychological counselling to HCWs during such outbreaks.
Introduction
Worker resilience refers to an individual’s ability to cope with stressful work-related situations, to remain focused and interested in their duties, and to ‘bounce back’ easily after adverse events [1]. This is especially important for healthcare workers (HCW), as the strain of work can lead to negative effects not only on the individual but also on their employee performance and the quality of patient care [2]. Stressors among workers at healthcare facilities can range from universal events such as work overload, conflict at the workplace, or aggression from supervisors, to healthcare-specific issues such as fear of acquiring infections from the hospital or grief from seeing dying patients [3, 4]. If left unchecked, highly stressful environments may lead to long-term and persistent psychological effects such as anxiety or panic disorders [5]. Resilience enables HCWs to cope with their work environment and maintain a healthy mental state despite the presence of stressful factors.
During ebola outbreaks, the healthcare system can experience extreme pressure due to sudden increased demand for medical resources, specialized equipment and isolation units, as well as disruption of routine health services. These pressures can have a negative impact on the mental health and resilience of the health workforce [6, 7] who may experience stressors such as limited availability of personal protective equipment (PPE), fear of infection and spread to family members, death of coworkers, lack of provision of risk allowances, and increased working hours and workload [6, 8, 9].
On September 20, 2022, the Uganda Ministry of Health (MoH) declared an outbreak of Sudan ebolavirus (SUDV) in Mubende District. This subsequently spread to Kassanda District, with the first case confirmed on October 13, 2022. Thus, these two districts became the epicenters of the outbreak, which later spread to other districts, including Kampala, Masaka, Jinja, Kyegegwa, Bunyangabu, Kagadi, and Wakiso [10]. By the end of the outbreak on January 11, 2023, among 142 confirmed cases, 19 were healthcare workers, seven of whom died [10]. We assessed the level and determinants of resilience at the workplace among HCWs at the epicenter of the SUVD outbreak response in Uganda to provide recommendations to the Ministry of Health (MoH) for psychosocial support for frontline HCWs during similar epidemics.
Methods
Study setting, design, and participants
We conducted cross-sectional survey of all HCWs at Mubende Regional Referral Hospital (MRRH), Kikandwa HCIII, and Madudu HCIII who worked for at least one day during the SUVD response period (September 20, 2022─January 11, 2023). These health facilities were selected due to their direct involvement in the response to SUDV outbreak. They were the referral centers where suspected SUVD cases were sent for isolation and treatment. The survey was conducted from February 27─March 24, 2022, six weeks after the end of the SUDV outbreak was declared.
MMRH, is a government-owned referral hospital located in Mubende District, which serves 8 districts in the north-central region of Uganda, and has 175 beds and 386 HCWs. Madudu HCIII, located in Mubende District, and Kikandwa HCIII, located in Kassanda District, are sub-county level health facilities, each with 15 beds and 21 health workers. MRRH and Madudu HCIII had formal Ebola Treatment Units (ETU)s established while Kikandwa HCIII, is located in a town which had a high number of SUVD (48/142) confirmed cases, and served as an isolation center for suspected patients while they awaited evacuation.
We defined a HCW as a person listed under the International Standard Classification of Occupations by the International Labor Organization as a healthcare professional. These included medical doctors, dentists, nursing and midwifery professionals, premedical practitioners, pharmacists, psychologists, social workers, environmental, occupational, hygiene professionals, and support staff [11].
We collected data using an interviewer-administered structured questionnaire which we developed based on previous resilience studies carried out during disease outbreaks [12-14]. A total of 400 HCWs were interviewed from all the health facilities. We included HCWs who directly took part in patient care and those who were not directly involved in patient care.
Data collection instruments and study variables
Data collected from HCWs included age, sex, level of education, professional cadre, hours worked per week, years of experience, number of children, monthly income range, number of persons with whom the health worker resides, whether the HCW directly or indirectly cared for a suspected SUDV patient at the health facility, level of resilience as the outcome variable.
We defined resilience as the HCW’s ability to cope with workplace stress during the period of the SUVD outbreak. We measured resilience using the Connor-Davidson Resilience Scale (CD-RISC-10). The CD-RISC-10 is a tool that measures the ability to cope with stress and adversity using a 10-item questionnaire with a 5-point Likert-type scale. Responses included ‘not true at all’ (scored as 0), ‘rarely true’ (scored as 1), ’sometimes true’ (scored as 2), ‘often true’ (scored as 3) and ‘true nearly all the time’ (scored as 4). Participants rated the items based on how they recalled feeling during the SUDV outbreak. The CD-RISC-10 has been validated in low and middle-income countries (LMIC) and has been shown to have good validity and reliability among healthcare workers [15].
The risk perception of SUDV was assessed using 11 statements relating to fear of contracting SUDV, fear of spreading SUDV, workplace conditions, and stigma. Respondents rated each statement on a 4-point Likert-type scale, with ‘strongly agree’ being scored as 0, ‘agree’ as 1, ‘disagree’ as 2, and ‘strongly disagree’ as 3. The higher score, signified a higher the level of risk perception.
Data management and statistical analysis
We entered data into Excel and exported to STATA version 16 software for analysis. Continuous and normally distributed data (age) were presented as mean and standard deviation (SD), while continuous non-normally distributed data (work experience and distance from home and workplace were presented as medians with interquartile ranges. Categorical data (sex, marital status, employment status, having received SUVD training, having contracted SUVD, and having received SUVD counselling) were presented inform of frequencies and percentages. We grouped respondents according to their resilience score, that is; low resilience (scores 0-21, up to 25th percentile), moderate resilience (scores 22-29, above 25th percentile but below 75th percentile), and high resilience (scores 30-40, above 75th percentile) and this was based on categorization from previous studies [16].
We used logistic regression to identify the factors associated with resilience. The resilience scores were recategorized into a binary outcome, where low and moderate: score of (1-29) was categorized as non-resilient and high: score of (30-40) as resilient. Adjusted odds ratios and confidence intervals were computed for all variables in the model. Statistical significance was tested using a 95% confidence interval and a P value of < 0.05.
Ethical considerations
We conducted this study in response to a public health emergency and as such was determined to be non-research. The MoH authorized this study and the office of the Center for Global Health, US Center for Disease Control and Prevention determined that this activity was not human subject research and with its primary intent being for public health practice or disease control.
We obtained permission to conduct the investigation from the district health authorities of Mubende and Kassanda. Permission was also obtained from the Director of MRRH and the facility heads of Madudu and Kikandwa HCIIIs. We obtained written informed consent from all the respondents. They indicated their consent by checking an appropriate box for consent before proceeding with the interviews. Participants were assured that their participation was voluntary and that there would be no negative consequences for declining or withdrawing from the study (none declined or withdrew). Data collected did not contain any individual personal identifiers and information was stored in password-protected computers, which were inaccessible by anyone outside the investigation team.
Results
Characteristics of study participants
Among 429 HCWs working in MRRH, Madudu HCIII, and Kikandwa HCIII, 400 (93%) completed the survey, with the majority coming from MRHH (92%). The mean age of respondents was of 35.3 ± 8.2 years (range, 20-58 years), median distance from home to workplace was 3km (range 0.5-17km) and median work experience of 8 years (range:1-38 years). Approximately half of the respondents (56%) were male. Support staff (28%) and nurses (18%) comprised nearly half of the respondents. Three quarters of the participants participated in the SUVD response (Table 1).
Table 1: Characteristics of study participants
| Characteristic | Number | (%) |
| Health facility | ||
| MRRH | 367 | (92) |
| Madudu HC III | 22 | (6) |
| Kikandwa HC III | 11 | (2) |
| Age in years | ||
| 20-29 | 94 | (24) |
| 30-39 | 217 | (54) |
| 40-49 | 58 | (14) |
| >50 | 31 | (8) |
| Sex | ||
| Male | 222 | (56) |
| Female | 178 | (44) |
| Cadre of HCWs | ||
| Support staff | 110 | (28) |
| Nurses | 72 | (18) |
| Medical doctors | 49 | (12) |
| Midwives | 41 | (10) |
| Clinical officers | 38 | (10) |
| Laboratory staff | 33 | (8) |
| Pharmacy personnel | 18 | (4) |
| Psychosocial staff | 17 | (4) |
| Dental personnel | 11 | (3) |
| Public health personnel | 11 | (3) |
| Marital status | ||
| Married | 250 | (63) |
| Single | 142 | (35) |
| Divorced | 8 | (2) |
| Work experience | ||
| ≤5 years | 120 | (30) |
| 5–10 years | 174 | (44) |
| >10 years | 106 | (26) |
| With whom does HCW reside | ||
| Family | 253 | (63) |
| Alone | 127 | (32) |
| Friends | 20 | (5) |
| Distance from home to the workplace (km) | ||
| <5 | 320 | (80) |
| 5-10 | 63 | (16) |
| >10 | 17 | (4) |
| Employment status | ||
| Permanent staff | 316 | (79) |
| Short term contract | 31 | (8) |
| Intern | 37 | (9) |
| Student | 16 | (4) |
| Monthly salary range (UGX) | ||
| <1,000,000 | 140 | (35) |
| 1,000,000-3,000,000 | 218 | (55) |
| 3,000,000-5,000,000 | 33 | (8) |
| >5,000,000 | 9 | (2) |
| Hours worked per week | ||
| ≤40 hours | 41 | (14) |
| >40 hours and above | 259 | (86) |
| Received SUVD training | ||
| Yes | 315 | (79) |
| No | 85 | (21) |
| Contracted SUVD | ||
| Yes | 5 | (1) |
| No | 395 | (99) |
| Received counselling services | ||
| Yes | 115 | (29) |
| No | 285 | (71) |
**Support Staff included drivers, guards, cleaners, and administrators
Level of resilience amongst healthcare workers working at the epicenter of the Ebola outbreak, Uganda 2022 (N=400)
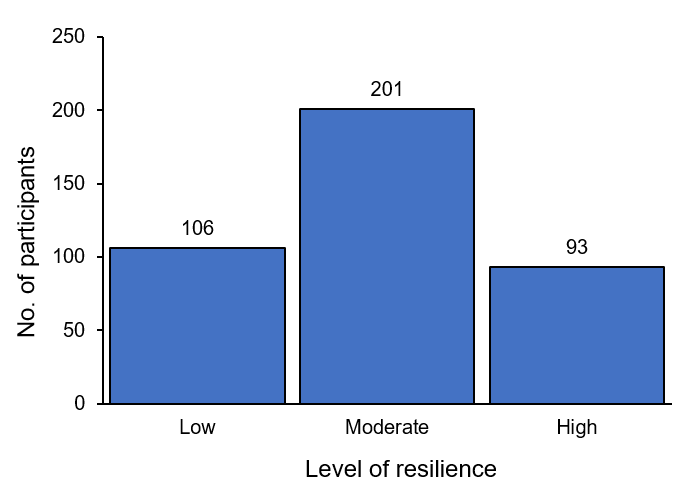
The overall mean resilience score was 25.2 ± 6.1. Half of the respondents 201 (50%) scored as having ‘moderate resilience’, 106 (27%) scored as ‘low resilience’, and 93 (23) scored as ‘high resilience’ (Figure 1).
Concerns of healthcare workers working at the epicenter of the SUVD outbreak, Uganda, 2022 (N=400)
The greatest concerns were about fear of exposure to SUVD. Three hundred and fifty-six (89%) felt they were at risk of contracting SUVD at their workplace. Most (89%) of respondents were concerned about stigma and felt that their workmates would avoid them if they contracted SUVD; 88%, felt that there were no adequate infection prevention and control (IPC) measures at the health facilities while 80% felt that their families would avoid them if they contracted SUVD. Most (68%) respondents felt that there was inadequate PPE at the health facilities while 64% considered resigning due to the SUVD outbreak (Table 2). Most respondents (88%) had more than one concern. There was no difference in resilience between respondents with one concern and those with more than one concern (p=0.826).
Table 2: Concerns of healthcare workers working at the epicenter of the SUVD outbreak, Uganda 2022 (N=400)
| Statement of concern | Yes(n) | % | No(n) | % |
| I felt that I was at risk of contracting SUVD at my workplace | 356 | 89 | 44 | 11 |
| I think my workmates would avoid me if I contracted SUVD | 356 | 89 | 44 | 11 |
| I feel that there were no adequate IPC measures available | 351 | 88 | 49 | 12 |
| I think my family would avoid me if I contracted SUVD | 321 | 80 | 79 | 20 |
| I feel that there was no adequate PPE | 273 | 68 | 127 | 32 |
| I thought of resigning from my workplace due to the SUVD outbreak | 257 | 64 | 143 | 36 |
| I thought that avoiding reporting for duty would reduce my chances of contracting SUVD | 235 | 59 | 165 | 41 |
| I feel the health facility was not well staffed to handle the SUVD response | 182 | 46 | 218 | 54 |
| I felt that my workplace would not support me in case I contracted SUVD | 168 | 42 | 232 | 58 |
| I feel the health facility was not well equipped to handle the SUVD response | 150 | 38 | 250 | 62 |
| I feel my workmates who contracted SUVD did not get appropriate treatment | 128 | 32 | 272 | 68 |
Factors associated with resilience among healthcare workers working at the epicenter of SUVD outbreak, Uganda, 2022 (N=400)
At bivariate analysis, age, cadre of HCW, work experience, distance from home to health facility, employment status, monthly salary range, hours worked per week, and receiving SUVD counselling were statistically significant while name of health facility, sex, marital status, receiving SUVD training, whom the person resides with and contracting SUVD were not. In multivariable analysis, resilience was associated with age >40 years (AOR 2.1; CI: 1.3-3.5), having work experience of >10 years (AOR 2.2; CI: 1.1-4.7) and working for >40 hours per week (AOR 6.8 CI: 2.1-22.7). It was also associated with living >10km away from the workplace (AOR 4.5 CI: 1.3-15.6), working as permanent staff (AOR 3.6 CI: 1.3-9.7), and receiving Ebola-specific counselling services (AOR 3.3 CI: 1.7-6.5). (Table 3).
Table 3: Factors associated with resilience among healthcare workers working at the epicenter of SUVD outbreak, Uganda, 2022 (N=400)
| Level of resilience | Bivariate analysis | Multivariate analysis | ||||||
| Resilient (n=93) | Not resilient (n=307) | OR (95%CI) | P value | AOR (95%CI) | P value | |||
| n | (%) | n | (%) | |||||
| Age in years | ||||||||
| 20-29 | 9 | (10) | 85 | (28) | 1.0 | Ref | 1.0 | Ref |
| 30-39 | 27 | (29) | 190 | (62) | 1.2 (0.9-1.6) | 0.241 | 1.4 (0.7-5.4) | 0.707 |
| 40-49 | 32 | (34) | 26 | (8) | 1.5 (1.1-2.2) | 0.022* | 2.1 (1.3-3.5) | 0.002* |
| ≥50 | 25 | (27) | 6 | (2) | 1.4 (0.9-2.1) | 0.149 | 1.7 (1.6-2.3) | 0.040* |
| Cadre of HCWs | ||||||||
| Support staff | 26 | (28) | 84 | (27) | 1.0 | Ref | 1.0 | Ref |
| Nurses | 12 | (13) | 60 | (20) | 1.7(0.5-1.8) | 0.322 | 2.2 (0.3-2.1) | 0.623 |
| Medical doctors | 9 | (10) | 40 | (13) | 1.3 (0.8-2.7) | 0.131 | 1.9 (0.7-3.4) | 0.078 |
| Midwives | 10 | (11) | 31 | (10) | 1.2 (0.3-7.1) | 0.094 | 1.4 (0.2-6.3) | 0.093 |
| Clinical officers | 11 | (12) | 27 | (9) | 2.1 (0.9-3.3) | 0.072 | 1.6 (0.8-2.2) | 0.138 |
| Laboratory staff | 7 | (8) | 26 | (8) | 0.9 (0.6-1.5) | 0.189 | 0.3 (0.1-7.1) | 0.075 |
| Pharmacy personnel | 3 | (3) | 15 | (5) | 1.7 (0.8-2.9) | 0.671 | 2.4 (0.2-3.3) | 0.327 |
| Psychosocial staff | 5 | (5) | 12 | (4) | 2.7 (1.7-1.3) | 0.031* | 2.2 (0.8-1.2) | 0.059 |
| Dental personnel | 4 | (4) | 7 | (2) | 0.4 (0.3-1.9) | 0.231 | 0.1 (0.7-6.6) | 0.423 |
| Public health personnel | 6 | (6) | 5 | (2) | 3.1 (1.2-5.5) | 0.011* | 2.9 (0.1-4.7) | 0.082 |
| Work experience | ||||||||
| ≤5 years | 28 | (30) | 92 | (30) | 1.0 | Ref | 1.0 | Ref |
| 5–10 years | 21 | (23) | 153 | (50) | 1.3 (0.3-1.7) | 0.083 | 1.1 (0.5-2.5) | 0.08 |
| >10 years | 44 | (47) | 62 | (20) | 1.4 (1.2-1.9) | 0.028* | 2.2 (1.1-4.7) | 0.04* |
| Distance from home to the workplace (km) | ||||||||
| ≤5 | 66 | (71) | 254 | (83) | Ref | – | Ref | – |
| 5-10 | 17 | (18) | 46 | (15) | 1.4 (0.8-2.6) | 0.264 | 0.8 (0.4-1.7) | 0.528 |
| >10 | 10 | (11) | 7 | (2) | 5.5 (2.0-15.0) | 0.001* | 4.5 (1.3-15.6) | 0.019* |
| Employment status | ||||||||
| Short contract staff | 21 | (23) | 10 | (3) | 1.0 | Ref | 1.0 | Ref |
| Permanent staff | 47 | (51) | 269 | (88) | 4.4 (1.5-12.8) | 0.007* | 3.6 (1.3-9.7) | 0.012* |
| Intern | 14 | (15) | 23 | (7) | 3.3 (1.0-10.3) | 0.042* | 3.0 (0.7-8.8) | 0.144 |
| Student | 11 | (11) | 5 | (2) | 2.2 (0.6-8.5) | 0.266 | 2.5 (0.7-8.8) | 0.159 |
| Monthly salary range (UGX) | ||||||||
| <1,000,000 | 21 | (23) | 119 | (39) | Ref | Ref | ||
| 1,000,000-3,000,000 | 52 | (56) | 166 | (54) | 2.7 (1.8-7.1) | 0.037* | 3.7 (0.4-3.2) | 0.677 |
| 3,000,000-5,000,000 | 17 | (18) | 16 | (5) | 3.9 (0.2-11.2) | 0.667 | 1.7 (0.1-9.8) | 0.326 |
| >5,000,000 | 3 | (3) | 6 | (2) | 1.9 (0.5-1.4) | 0.821 | 2.5 (0.7-1.8) | 0.083 |
| Hours worked per week | ||||||||
| ≤40 hours | 4 | (5) | 37 | (17) | Ref | – | Ref | – |
| >40 hours | 77 | (95) | 182 | (83) | 3.9 (1.3-11.4) | 0.012* | 6.8 (2.1-22.7) | 0.002* |
| Received SUVD counselling services | ||||||||
| No | 46 | (49) | 239 | (78) | Ref | – | Ref | – |
| Yes | 47 | (51) | 68 | (22) | 3.6 (2.2-5.8) | <0.000* | 3.3 (1.7-6.5) | <0.000* |
Discussion
We assessed the level and determinants of resilience at workplace among HCWs working at the epicentre of the September 2022 SUVD outbreak in Uganda. The majority of the respondents were not resilient to stress. Resilience was associated with older age, more work experience, working for long hours, living further away from the workplace, working as permanent staff, and having received counselling services. The HCW’s main concern was the risk of contracting SUVD and stigma at the workplace if they had contracted the disease. This study demonstrates opportunities to improve the services to HCWs and boost their resiliency as they provide healthcare in emergency outbreak responses.
Majority of the HCWs were not resilient to stress. The work environment during an outbreak setting is chaotic and stressful for HCWs[17] and this affects their mental health and resilience. In our study, majority of the HCWs (89%) felt that they were at risk of contracting SUVD, (88%) felt that there weren’t adequate IPC measures while (68%) felt that there weren’t adequate PPEs at the workplace. Additionally, 89% of HCWs felt that they would be stigmatized by fellow workmates in case they contracted SUVD. These workplace attributes could have contributed to low resilience amongst the HCWs.
Studies have demonstrated that the availability of PPE, medical supplies, and implementation of IPC measures at workplaces during outbreak settings provide a part of a conducive workplace environment for HCWs and builds their resilience [18]. Low resilience was also reported in Italy amongst frontline HCWs during the COVID-19 pandemic[19]. The fear of getting infected and spreading the disease and colleagues are among the reasons that increased the risk of getting stress and low resilience. It is therefore important that during outbreaks, workplaces address the challenges that increase the risk perception of HCWs to getting infected at workplaces.
Older healthcare workers (>40 years) and those with longer work experience were more likely to be resilient. This may be because older people have been exposed to different stressors throughout their life and hence developed stress resistance traits or stress coping strategies. Studies have demonstrated that older people have a higher ability to bounce back and recover after physical and psychological adversity [20]. Findings of our study are consistent with those of other studies which reported that resilience was high among older people[21, 22].
Work experience plays an important role in resilience and coping with stress. HCWs who have stayed long on the job have cumulatively faced numerous work-related stressors during their career [23] and as a result, developed coping strategies to stress. An Iranian study amongst nurses during the COVID-19 outbreak demonstrated that nurses who had more work experience had a higher resilience [24].
Additionally, studies show that HCWs with little experience are more likely to be affected by the outcomes of low resilience like depression, burnout, and depression when faced with adversity [25, 26]. Old age and longer work experience could be protective factors in highly stressful events. Individuals with old age and long work experience can be utilized as positive role models and mentors during emergency outbreak responses.
Healthcare workers who worked longer hours were more resilient than their colleagues. During an outbreak response, there is an increased workload which necessitates working long hours, a high sense of urgency among HCWs and teamwork aimed at addressing and stopping the spread of the threat[27]. It could be possible that HCWs worked long hours in this outbreak response with support from workmates and this may have enabled them to build resilience.
In the current study, majority (86%) of HCWs worked for more than 40 hours a week during the response period. Although our study links high resilience to long working hours, several studies conducted during the COVID-19 pandemic demonstrated that working long hours is associated with negative mental health consequences like burnout, and exhaustion at the workplace which in turn affect an individual’s resilience to stress [28].
The difference in results could be that in our study the SUVD outbreak lasted for a short duration (4 months) while the COVID-19 response was long and protracted (more than 2 years) which could have inflicted prolonged emotional pressure on HWCs[29]. It is important to avoid working long hours even in emergency outbreak response situations. It is advisable that conducive work environments are created which promote teamwork and working in shifts during outbreaks.
Permanently employed staff were more resilient than other categories of employees. This could be because this category of employees has a higher sense of job security with less financial stress. Studies have shown that employees employed on a permanent basis have job security [30]. The phenomenon of job security can translate into a sense of feeling less stressed with a high degree of resilience. Consistent with other studies, job insecurity and lack of financial stability have been identified as some of the stressors amongst HCWs, especially during epidemics [31-33].
Job security is an important component of financial stability and a shield against some stressors which could affect an individual’s resilience. Although outbreak response situations attract diverse human resources with different skill sets, the utilization of staff with permanent contracts seems to be a protective factor against stress. Healthcare managers may utilize a good number of them during outbreak response situations.
Healthcare workers who lived a distance away from their workplaces were more resilient. This is consistent with a previous study in Ethiopia, which showed that high levels of stress and perceived risk of contracting diseases for HCWs during epidemics were linked to living near their workplace health facilities [34]. The findings of this study are in line with a study done in Peru which indicated that HCWs’ anxiety and mental distress decreased as the distance from the COVID-19 outbreak epicentre increased[35]. Several other studies further affirm that distance away from the epicentre during epidemics is a protective factor against mental health problems [36, 37]. This may be due to the ability to create physical space between themselves and their workplaces. Physical space is important as it gives provides protection against infection at the workplace but it could also encourage absenteeism. It is important for healthcare managers to put up measures that reduce the risk of contracting infection among HCWs while at the workplace.
Healthcare workers who received Ebola-related counselling services were more resilient than those who didn’t. Counselling plays an important role in building resilience and coping during times of adversity as it relieves depression, anxiety, stress and other mental health conditions [38]. Our findings are consistent with other studies which have shown that HCWs who receive counselling services have better psychological wellbeing and are more resilient in situations when bombarded with constant stressors [39]. This emphasises the importance of providing counselling services to HCWs during outbreak emergency responses.
Study limitations and strengths
We acknowledge some limitations in our study. First, the exclusive reliance on self-reported measures for resilience may have had a risk of response bias including the social desirability bias. Secondly, the cross-sectional nature of the study made it difficult to draw the association between the study variables in terms of cause and effect. Despite these limitations, our study conducted a census of all HCWs who worked at the SUVD epicentre. This gave the study high power. Additionally, findings from this study provides evidence to MoH about the key drivers of resilience amongst HCWs who worked at the epicentre of the SUVD outbreak. These can be used to design policies that support the establishment of resilient HCWs at workplaces and during future similar outbreaks.
Conclusion
Our findings suggest that majority of the HCWs were not resilient to stress. Factors associated with resilience included being aged above 40 years, having 10 or more years of work experience, permanent employment status, working long hours, staying away from the health facility and receiving counselling services.
We reveal several factors which healthcare managers can use to build resilience amongst health workers. We recommend that old age and experienced HCWs be used as positive role models and team leaders during disease outbreak situations to mentor junior and young colleagues. Additionally, strategies aimed at reducing the perceived risk of infection in the workplace, like timely availability of PPEs and strengthening IPC measures, provision of counselling and psychosocial support services, team building activities to promote interaction and communication between co-workers, and assurance of safety at the workplace could improve on resilience amongst HCWs during such outbreaks.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
We appreciate the HCWs who participated in this study. We are also grateful to the administration of MMRH, Kikandwa HCIII and Madudu HCIII for the support they provided during this investigation. We also appreciate Public Health Fellowship Program and the Ministry of Health, Public Health Emergency Operations Centre for the technical support and guidance offered during this study. Finally, we thank the US-CDC for supporting the activities of the Uganda Public Health Fellowship Program.
Copyright and licensing
All materials in the Uganda Public Health Quarterly Epidemiological Bulletin are in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Yılmaz EB: Resilience as a strategy for struggling against challenges related to the nursing profession. Chinese Nursing Research 2017, 4(1):9-13.
- Portoghese I, Galletta M, Coppola RC, Finco G, Campagna M: Burnout and workload among health care workers: the moderating role of job control. Safety and health at work 2014, 5(3):152-157.
- Vicente ADA, Shadvar S, Lepage S, Rennick JE: Experienced pediatric nurses’ perceptions of work-related stressors on general medical and surgical units: A qualitative study. International Journal of Nursing Studies 2016, 60:216-224.
- Enns CL, Sawatzky J-AV: Emergency nurses’ perspectives: Factors affecting caring. Journal of Emergency Nursing 2016, 42(3):240-245.
- Sun P, Wang M, Song T, Wu Y, Luo J, Chen L, Yan L: The Psychological Impact of COVID-19 Pandemic on Health Care Workers: A Systematic Review and Meta-Analysis. Frontiers in psychology 2021, 12:626547.
- Raven J, Wurie H, Witter S: Health workers’ experiences of coping with the Ebola epidemic in Sierra Leone’s health system: a qualitative study. BMC health services research 2018, 18:1-9.
- Ricci-Cabello I, Meneses-Echavez JF, Serrano-Ripoll MJ, Fraile-Navarro D, de Roque MAF, Moreno GP, Castro A, Ruiz-Pérez I, Campos RZ, Gonçalves-Bradley D: Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review. MedRxiv 2020:2020.2004. 2002.20048892.
- Paladino L, Sharpe RP, Galwankar SC, Sholevar F, Marchionni C, Papadimos TJ, Paul E, Hansoti B, Firstenberg M, Garg M et al: Reflections on the Ebola Public Health Emergency of International Concern, Part 2: The Unseen Epidemic of Posttraumatic Stress among Health-care Personnel and Survivors of the 2014-2016 Ebola Outbreak. Journal of global infectious diseases 2017, 9(2):45-50.
- Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, Di Pierro R, Madeddu F, Calati R: The Psychological Impact of Epidemic and Pandemic Outbreaks on Healthcare Workers: Rapid Review of the Evidence. Current Psychiatry Reports 2020, 22(8):43.
- UNICEF: Ebola disease caused by Sudan ebolavirus-Uganda-https://https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON433. In.; Jan 2023.
- Organization WH: The world health report 2006: working together for health: World Health Organization; 2006.
- Yıldırım M, Arslan G, Özaslan A: Perceived risk and mental health problems among healthcare professionals during COVID-19 pandemic: Exploring the mediating effects of resilience and coronavirus fear. International Journal of Mental Health and Addiction 2020:1-11.
- Giordano F, Cipolla A, Ungar M: Building resilience for healthcare professionals working in an Italian red zone during the COVID‐19 outbreak: A pilot study. Stress and Health 2022, 38(2):234-248.
- Migisha R, Ario AR, Kwesiga B, Bulage L, Kadobera D, Kabwama SN, Katana E, Ndyabakira A, Wadunde I, Byaruhanga A: Risk perception and psychological state of healthcare workers in referral hospitals during the early phase of the COVID-19 pandemic, Uganda. BMC psychology 2021, 9(1):1-9.
- Aloba O, Olabisi O, Aloba T: The 10-item Connor–Davidson Resilience Scale: Factorial structure, reliability, validity, and correlates among student nurses in southwestern Nigeria. Journal of the American Psychiatric Nurses Association 2016, 22(1):43-51.
- Chen H, Gao J, Dai J, Mao Y, Wang Y, Chen S, Xiao Q, Jia Y, Zheng P, Fu H: Generalized anxiety disorder and resilience during the COVID-19 pandemic: evidence from China during the early rapid outbreak. BMC Public Health 2021, 21:1-10.
- Forrester JD, Hunter JC, Pillai SK, Arwady MA, Ayscue P, Matanock A, Monroe B, Schafer IJ, Nyenswah TG, De Cock KM: Cluster of Ebola cases among Liberian and US health care workers in an Ebola treatment unit and adjacent hospital—Liberia, 2014. Morbidity and Mortality Weekly Report 2014, 63(41):925.
- Thatrimontrichai A, Weber DJ, Apisarnthanarak A: Mental health among healthcare personnel during COVID-19 in Asia: A systematic review. Journal of the Formosan Medical Association 2021, 120(6):1296-1304.
- Di Giuseppe M, Nepa G, Prout TA, Albertini F, Marcelli S, Orrù G, Conversano C: Stress, burnout, and resilience among healthcare workers during the COVID-19 emergency: the role of defense mechanisms. International journal of environmental research and public health 2021, 18(10):5258.
- Van Kessel G: The ability of older people to overcome adversity: a review of the resilience concept. Geriatric Nursing 2013, 34(2):122-127.
- Aldarmasi MA: Factors Associated With Resilience Among Healthcare Professionals During the COVID-19 Pandemic: A Cross-Sectional Study. Cureus 2022, 14(5).
- Eshel Y, Kimhi S, Lahad M, Leykin D: Individual, community, and national resiliencies and age: Are older people less resilient than younger individuals? The American Journal of Geriatric Psychiatry 2016, 24(8):644-647.
- McCann CM, Beddoe E, McCormick K, Huggard P, Kedge S, Adamson C, Huggard J: Resilience in the health professions: A review of recent literature. International Journal of Wellbeing 2013, 3(1).
- Afshari D, Nourollahi-darabad M, Chinisaz N: Psychosocial factors associated with resilience among Iranian nurses during COVID-19 outbreak. Frontiers in public health 2021:1092.
- Båtsman A, Fahlbeck H, Hildingsson I: Depression, anxiety and stress in Swedish midwives: A cross-sectional survey. European Journal of Midwifery 2020, 4.
- Jemal K, Deriba BS, Geleta TA, Tesema M, Awol M, Mengistu E, Annous Y: Self-reported symptoms of depression, anxiety, and stress among healthcare workers in Ethiopia during the COVID-19 pandemic: a cross-sectional study. Neuropsychiatric Disease and Treatment 2021:1363-1373.
- Mattila E, Peltokoski J, Neva MH, Kaunonen M, Helminen M, Parkkila A-K: COVID-19: anxiety among hospital staff and associated factors. Annals of Medicine 2021, 53(1):237-246.
- Ching SM, Ng KY, Lee KW, Yee A, Lim PY, Ranita H, Devaraj NK, Ooi PB, Cheong AT: Psychological distress among healthcare providers during COVID-19 in Asia: Systematic review and meta-analysis. PLOS ONE 2021, 16(10):e0257983.
- Murphy B: System Factors Influencing Stress in Healthcare Workers during the COVID-19 Pandemic: A Case Study and Scoping Review. The University of Iowa; 2022.
- Callea A, Urbini F, Ingusci E, Chirumbolo A: The relationship between contract type and job satisfaction in a mediated moderation model: The role of job insecurity and psychological contract violation. Economic and Industrial Democracy 2016, 37(2):399-420.
- Hamouche S: COVID-19 and employees’ mental health: stressors, moderators and agenda for organizational actions. Emerald Open Research 2020, 2.
- Mugisa T: Job insecurity and organizational commitment during the Covid-19 Pandemic among private High school teachers in Wakiso District in Uganda. Makerere University; 2022.
- Yılmaz Y, Üngüren E, Tekin ÖA, Kaçmaz YY: Living with infection risk and job insecurity during COVID-19: the relationship of organizational support, organizational commitment, and turnover intention. International journal of environmental research and public health 2022, 19(14):8516.
- Aliyi AA, Ketaro MK, Engida ZT, Argaw AM, Muhammed AH, Hassen MM, Abduletif AM, Shiferaw DS, Wodera AL, Ayene SH: Risk perception, community myth, and practices towards COVID-19 pandemic in Southeast Ethiopia: Community based crossectional study. Plos one 2022, 17(10):e0275331.
- Yáñez JA, Jahanshahi AA, Alvarez-Risco A, Li J, Zhang SX: Anxiety, distress, and turnover intention of healthcare workers in Peru by their distance to the epicenter during the COVID-19 crisis. The American Journal of Tropical Medicine and Hygiene 2020, 103(4):1614.
- Di Trani M, Mariani R, Ferri R, De Berardinis D, Frigo MG: From resilience to burnout in healthcare workers during the COVID-19 emergency: the role of the ability to tolerate uncertainty. Frontiers in Psychology 2021, 12:646435.
- Rosales-Vaca KM, Cruz-Barrientos OI, Girón-López S, Noriega S, More-Árias A, Guariente SMM, Zazula R: Mental health of healthcare workers of Latin American countries: A review of studies published during the first year of COVID-19 pandemic. Psychiatry Research 2022:114501.
- Arnout BA, Almoied AA: A structural model relating gratitude, resilience, psychological well‐being and creativity among psychological counsellors. Counselling and Psychotherapy Research 2021, 21(2):470-488.
- Minnie L, Goodman S, Wallis L: Exposure to daily trauma: The experiences and coping mechanism of Emergency Medical Personnel. A cross-sectional study. African journal of emergency medicine 2015, 5(1):12-18.


Comments are closed.