An outbreak of scabies in a fishing community in Hoima District, Uganda, February−June, 2022
Authors: Rebecca Akunzirwe1*, Brian Agaba1, Saudah Luyima1, Lilian Bulage1, Benon Kwesiga1, Richard Migisha1, Robert Kaos Majwala2,3, Peter Chris Kawungezi1, Jane Frances Zalwango1, Daniel Kadobera1, Alex Riolexus Ario1,4 Institutional affiliations: 1Uganda Public Health Fellowship Program-Uganda National Institute of Public Health, Kampala, Uganda, 2Global Health Security Department, Baylor, Kampala, Uganda, 3Department of Epidemiology, Surveillance and Public Health Emergencies, Ministry of Health, Kampala, Uganda, 4Uganda National Institute of Public Health *Correspondence: Email: rakunzirwe@musph.ac.ug, Tel:+256772229130
Summary
Background: Scabies is endemic in most tropical areas. On May 21, 2022, the Ugandan Ministry of Health was notified of >1,000 cases of scabies in Hoima District. We investigated to assess the scope of the outbreak and identify associated factors.
Methods: We defined a suspected scabies case as the onset of an itchy pimple-like skin rash or crusting from January 2021 to July 2022 in a resident of Hoima District. We reviewed medical records, performed active community case-finding, and computed attack rates by age, sex, and village per 1,000 population. Using logistic regression, we compared exposures among 101 case-patients and 99 unmatched controls living in Rwentale Landing Site in Hoima during June 2022.
Results: We found 2,236 suspected cases in Hoima District. Children aged 5–14 years were more affected (AR=64/1,000) than persons aged ≥15 years (AR=8/1,000) (p<0.001). Males (AR=27/1,000) were more affected than females (AR=15/1,000) (p<0.001). Of the 54 affected villages, Rwentale Village had the highest attack rate (AR=233/1,000 population). Rwentale Village includes a fishing area known as Rwentale Landing Site where 1,119 (50%) cases in Hoima District were identified. At this landing site, cases began in April 2022 shortly after the end of the peak fishing and trading season. Being aged 5–14 years (AOR=4.9, 95%CI: 2.0–12), being male (AOR=2.4, 95%CI 1.1–5.1), living with another case (AOR=3.1, 95%CI: 1.5–6.2), and sharing three or more personal care items (towel, beddings, clothes, or sponges) (AOR=2.2, 95%CI: 1.1–4.6) were associated with case status.
Conclusion: This scabies outbreak was likely initiated by person-person interactions during peak fishing and trading months at a landing site and propagated by close household interactions. We recommend community sensitization on scabies, especially before fishing and trading seasons, for early prevention of future outbreaks.
Introduction
It is estimated that more than 200 million persons globally suffer from scabies at any time, accounting for 0.21% of disability-adjusted life years from all conditions (1, 2). The highest rates occur in hot tropical climates where the disease is endemic (3, 4). Scabies, an extremely itchy skin condition, is caused by the human itch mite Sarcoptes scabiei var. hominis (4). Disruptions in the skin barrier from excessive scratching predispose persons with scabies to bacterial superinfection (commonly, Streptococcus pyogenes and Staphylococcus aureus) that can result in complications, including pyoderma, impetigo, cellulitis, rheumatic heart disease, and kidney disease (5, 6).
The acute symptoms and secondary consequences associated with scabies infestation cause severe socioeconomic hardship for those who have it, their families, communities, and the healthcare system (1, 7). The price of medications, institutional outbreaks brought on by hospitalization of cases, and lost productivity are the primary direct financial expenses of scabies (1, 7). Owing to the morbidity and financial burden associated with scabies, the World Health Organization (WHO) recently designated scabies as a Neglected Tropical Disease (NTD) to emphasize the urgency of giving the illness top priority in low- and middle-income countries (8).
Direct contact with infested skin, is the main method of scabies transmission (8). Transmission may also occur through contact with contaminated personal care items like clothing, bedding, and towels. The primary contributing factors to scabies infestation are overcrowding, poor sanitation, and poverty (4, 9, 10). As such, the incidence of the disease may increase during natural or man-made disasters.
In Uganda, there have been five reported outbreaks of scabies from 2020 to 2022, two of which were in Hoima District (11-15); in 2020, more >2,000 persons were affected (14). On May 21, 2022, the Ministry of Health (MoH) received an alert from the Hoima District Health Office of a suspected outbreak of scabies. More than 1,000 persons from 16 villages had reportedly been affected. We investigated to determine the scope of the outbreak and identify risk factors to inform evidence-based control and prevention interventions.
Methods
Study setting
Hoima District is located in the Mid-western region; approximately 220 kilometres from Kampala, Uganda’s capital. A total of 400,000 individuals reside in the district’s 13 sub-counties, 54 Parishes, and 643 localities (16). Hoima District stretches to the national boundary of the Democratic Republic of Congo in the Western and is covered by Lake Albert and other water bodies.
Although subsistence farming is the major economic activity in Hoima District, at Lake Albert which covers 38% of the district, fishing is key (10). There are two fishing seasons: one in February to March and another in November to December. The social and economic growth of the sub-counties of Kigorobya, Buseruka, Kabwoya, and Kyangwali have been significantly impacted by fishing (10). There are 22 boat landing locations, and they act as important markets. The principal boat landing areas are in Tonya, Bugoma, and Nkon parishes (10).
Case definition and finding
We defined a suspected scabies case as the onset of an itchy pimple-like skin rash, or crusting from January 2021-July 2022 in a resident of Hoima District, Uganda. Using a scabies case investigation form developed for this outbreak, we obtained data on patient demographic information (age, sex, parish, and sub-county of residence) and clinical information. With the help of community health workers, we also conducted an active community case search in the affected sub counties. We first oriented the community health workers on case definitions, and we then went door to door identifying cases.
Descriptive epidemiology
We assessed the distribution of cases over time by constructing epidemic curves. We computed attack rates by person (age and sex) and place characteristics (sub county and village) using the Uganda Bureau of Statistics revised population projection from 2015 to 2030 for 146 districts (16). We also drew a choropleth map of the district indicating the most affected sub counties.
Hypothesis generation interviews
We conducted key informant interviews with four village leaders, and eight healthcare workers to identify possible factors associated with the outbreak. We conducted hypothesis-generating interviews of ten conveniently sampled scabies cases in the most affected village using a scabies case investigation form developed for this outbreak. We explored about the number of persons per household, the number of personal care items shared, personal hygiene, being infested with scabies before, and having visitors during the peak fishing and trading months.
Case-control study
We conducted an unmatched case-control study at the most affected village to test our generated hypotheses. We defined a scabies case as the onset of an itchy pimple-like skin rash or crusting in a resident of the Rwentale landing site from June 1 to 30, 2022. A control was the absence of the above symptoms in a resident of the Rwentale landing site from April to June 2022. This was done considering two incubation periods (two months) to minimize the chance of recruiting infested persons that were in the incubation period.
We estimated the sample size using the formula for comparison of two proportions (17). We assumed a 5% level of significance and 80% power. Using sex as a significant factor, with 0.72 of cases and 0.52 of controls exposed and an odds ratio of 2.69 (10), a minimum of 144 participants was computed . We further adjusted for 10% non-response, increasing the sample size to 160 participants. However, we increased this sample size to 200 to improve power to detect differences between exposures for cases and controls.
We obtained data on age, sex, number of shared personal care items, number of visitors that were living with participant in their household from February to March 2022 (the peak fishing and trading months), living with a scabies case-person in the same household during two months before symptom onset and personal hygiene. We assessed personal hygiene using an adapted Global Health Survey Hygiene (GSHS) questionnaire (18) (Table 1). The GSHS questionnaire assesses ten core areas including hygiene, that are leading causes of morbidity and mortality among children and adults globally (18).The maximum possible score was 12; a score of 6 or more was graded as good personal hygiene while a score of 5 or less was graded as poor personal hygiene (19) (Table 1).
Table 1: Personal hygiene assessment questions and scores
| Activity | Score |
| Number of times brushing teeth | |
| Irregularly | 0 |
| Once daily | 1 |
| Two or more times daily | 2 |
| Number of times taking bath with soap | |
| Irregularly | 0 |
| Once daily | 1 |
| Two or more times daily | 2 |
| Hand washing before eating with soap | |
| Yes | 2 |
| No | 0 |
| Hand washing after toilet with soap | |
| Yes | 2 |
| No | 0 |
| Wearing clean clothes | |
| Yes | 1 |
| No | 0 |
| Hair combed | |
| Yes | 1 |
| No | 0 |
| Are nails cut | |
| Yes | 1 |
| No | 0 |
| Are nails clean | |
| Yes | 1 |
| No | 0 |
For each case-person, a control was chosen. A list of all 312 affected households obtained from the chairperson and community health workers was used as the sampling frame. A sampling interval was generated by dividing the total number of affected households by the number of cases to be selected from the village. A computer-generated random number was used to get the first household from which the interval was applied to get to the next household.
As such, every third household was sampled from the list of affected households. We obtained one case from each household. If more than one case was found in a household, we randomly selected the case. The household participants were told to choose from random slips of paper, and then the one with the lowest number was enrolled as the case. The procedure was repeated to obtain controls. However, because there were only 102 households that did not have a case, controls were enrolled consecutively.
Data were exported to and analyzed using Stata version 14.0 (Stata Corporation, College Station, Texas, USA). A stratified analysis based on case status was carried out for descriptive analysis of baseline characteristics of the study population. The distribution of participants’ categorical characteristics (age, sex, having visitors during the peak fishing and trading months, personal hygiene, living with a scabies case patient, number of personal care items shared) was summarized as frequencies, proportions, and percentages and presented in form of contingency tables.
To determine factors associated with scabies infestation, odds ratios between individual predictors and scabies infestation at the bivariate level were assessed and those that were hypothesized to be associated with case status as well as those with a p-value <0.2 were considered for the multivariable analysis.
The presence of Interaction was assessed using the log-likelihood test by comparing full and reduced models. Confounding variables were assessed by comparing odds ratios of scabies infestation of unadjusted models and adjusted models. Variables that caused a difference between the odds ratios of both models of at least 10% were considered confounders. Variables with a p-value less than 0.05 were regarded as statistically significant, confounding variables as well as those that caused significant interaction were to be left in the model, however, these were not found. The goodness of fit of the regression model to the data was assessed using the Hosmer-Lemeshow test.
Ethical considerations
This outbreak investigation was in response to a public health emergency and was therefore determined to be non-research. The MoH gave a directive to investigate this outbreak and the office of the Center for Global Health, US Center for Disease Control and Prevention determined that this activity was not human subject research and that its primary intent was for public health practice or disease control.
The authors sought permission to conduct the investigation from District Health authorities of Hoima District. Permission was also sought from the administrators of the health facilities to access data about patients who had been visited the facility or been admitted with a scabies diagnosis. The authors sought verbal informed consent from the respondents who were at least 18 years old as well as those that were below 18 years of age and emancipated. The authors also sought assent from children below 18 years of age who were not emancipated and informed verbal consent from their parents or guardians. Data which was collected did not contain individual personal identifiers as a way of ensuring confidentiality
Results
Descriptive epidemiology
We line listed 2,236 suspected scabies cases in Hoima District from January 2021 to July 2022. The overall attack rate of scabies in Hoima District was 21/1,000 population with no deaths. Children 5 to 14 years old were the most affected (64/1,000), followed by children <5 years (36/1,000), and least affected was persons ≥15 years (8/1,000). Males (27/1,000) were more affected than females (15/1,000).
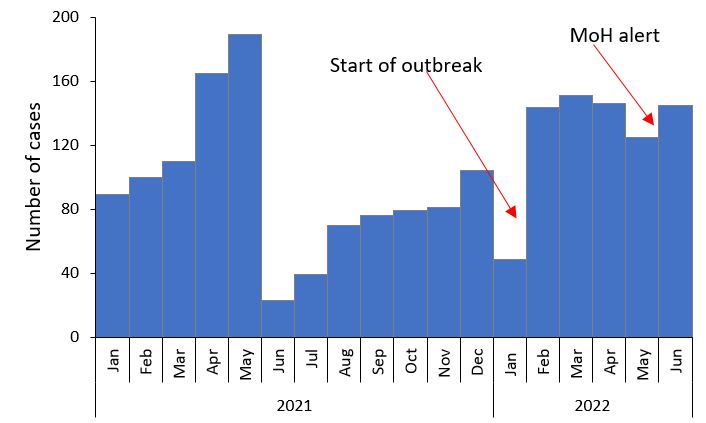
The epidemic curve showed peaks in the number of scabies cases from January to May in 2021 and February to June in 2022. Although the outbreak in 2022 started in February, the Ministry of Health was alerted on May 28, 2022 (Figure 1).
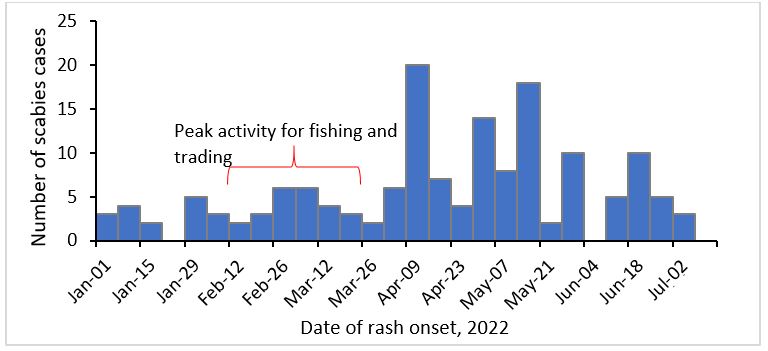
The epidemic curve for Rwentale village, Buseruka sub-county (the most affected area), Hoima District revealed a propagated outbreak with probable periods of exposure occurring between February 26 to March 5, 2022. This coincided with the peak fishing and trading activity which occurs from early February to April (Figure 2).
In Hoima District, Buseruka Sub-county, which has the principal landing site, had the highest attack rate (97/1,000) (Figure 3A, 4B).
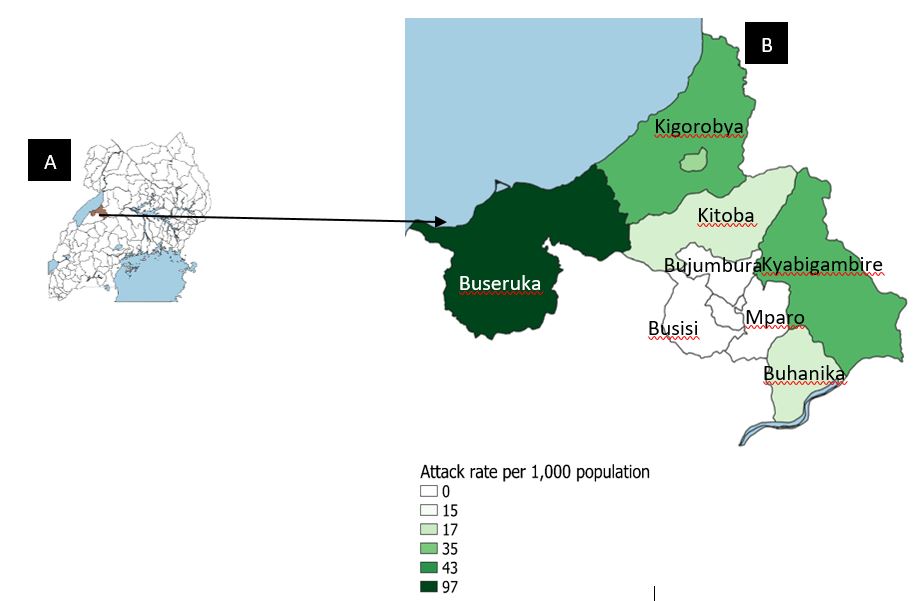
Figure 3B: Attack rates per 1,000 persons by sub county, Hoima District, January 2021─June 2022
Of the seven villages in Buseruka sub-county, Rwentale landing site village was most affected (A/R 233/1,000 persons), followed by Fofo (205/1,000 persons), Kyakaboga B (111/1,000 persons), Resettlement (50/1,000 persons), Hoimo (11/ 1,000 persons), Tonya B (7/1,000 persons), and Kyakaboga A (6/1,000 persons).
Hypothesis generation interview findings
Key informant findings
Three major themes emerged as drivers for the scabies outbreak in Rwentale Village: poor personal hygiene, increased interaction during business seasons, and sharing personal care items.
Increased human interaction during business seasons
During business seasons, there were many people that gathered from different areas and this was likely why the cases increased.
A participant noted, “You see, during the business season.. when the fishing season comes, many people come here, some come with the disease… people mix a lot… that is why I think the people with this disease are many now.” Village leader
Poor personal hygiene
The participants said that there were increased cases due to poor personal cleanliness. They believed that the illness was from organisms in the soil and dirty water. Thus, persons that did not bathe regularly, wash their clothes, or had dirty hair likely harboured the organism.
A participant noted, “It is this tribe X who do not bathe, they never wash their clothes… even when they bathe, they use water from the lake which has the organism that brings this disease.” Village leader, Rwentale Village
Sharing personal care items
The participants noted that sharing personal care items was likely a driver of the outbreak.
A participant said, “Our people are very communal people, they share everything.. even towels, basins. As they share these things, they pass on the parasite to other people..” Healthcare worker
Structured interview findings
Of the 10 case-persons interviewed, 9(90%) reported sharing personal care items, 8(80%) had poor personal hygiene, 8(80%) had been infested with scabies before, and 8(80%) had visitors during February to March (the peak fishing and trading months).
We hypothesized that having visitors during the peak fishing and trading seasons, poor personal hygiene, and sharing personal care items were associated with case status.
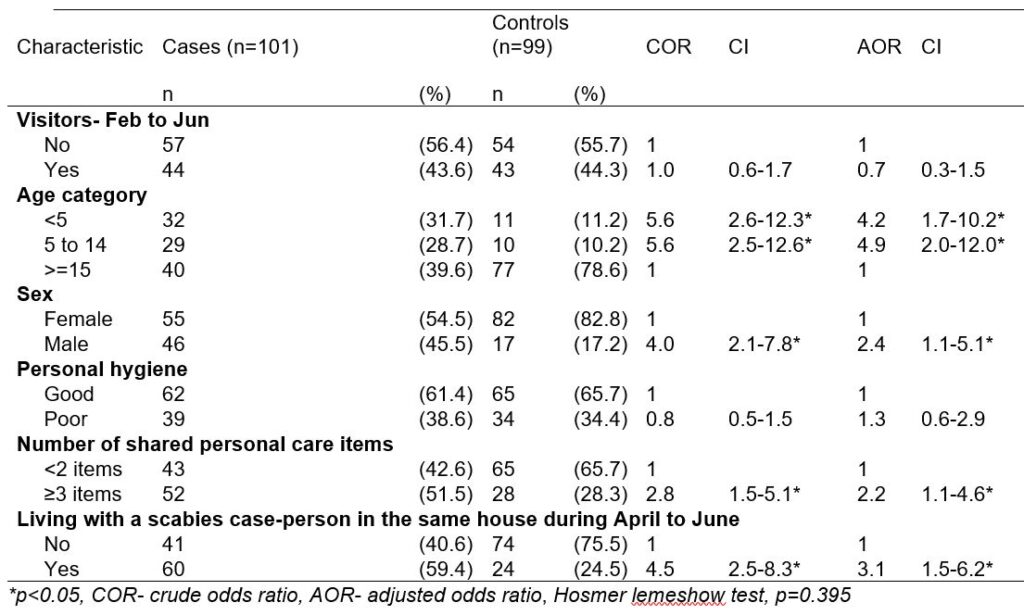
Case-control study findings
The case-control study had 101 cases and 99 controls. Among the cases, 40 (39.6%) and compared to 77(78.6%) of controls were 15 years or older. In multivariable analysis, being aged <5 years (OR=4.2, 95%CI: 1.7-10) and 5 to 14 years (AOR=4.9, 95%CI: 2.0-12), having shared four personal items compared to two (AOR=8.9, 95%CI: 2.2-36.2), being male (AOR=2.4, 95%CI: 1.1-5.1), and having a previous scabies diagnosis (AOR=3.1, 95%CI: 1.5-6.2) were associated with case-status (Table 3).
Table 3: Factors associated with Scabies Infestation among residents of Rwentale Village, Hoima District, June 2022
Discussion
We investigated the Scabies outbreak in Hoima District, Uganda in June 2022. The outbreak in Hoima District started in February 2022 yet the Ministry of Health only received the alert on May 28, 2022. The most affected sub-county was Buseruka, while the most affected village in Buseruka was Rwentale Landing Site Village. The scabies outbreak in Rwentale Village started in April approximately two months after the peak fishing and trading months. Being <15 years old, male, living with another case, and sharing personal care items with persons infested with scabies were associated with case status.
Although the most recent outbreak in Hoima District started in February 2022, the Ministry of Health received an alert on May 28, 2022. In Uganda, there is no formal scabies-specific surveillance system. Scabies is reported generically as a skin disease in the health unit outpatient monthly report. Without a scabies-specific surveillance system, it may be difficult to monitor the true burden of the disease and changes in its occurrence (20).
Buseruka was the most affected sub-county in Hoima District. This is likely because of its location as a border sub-county. The most affected village, Rwentale, is located in Tonya parish which is a principal landing area. Rwentale, being the most active landing site village and densely populated, likely had more person-to-person interactions which facilitated the spread of scabies (4, 21). The outbreak in Rwentale Landing Site started in April 2022. This was approximately two months after the peak fishing and trading activity occur at the landing site, which brings high levels of business and visitors to the area (4). The two months period following peak fishing and trading activity coincided with the incubation period for scabies infestation (4).
Males had about thrice the odds of contracting scabies compared to females, just like highlighted by studies conducted in similar resource-limited settings including Ethiopia (10, 22-24). This is likely because men dominate commercial activities in Uganda (25). As such, they may participate more than females in commercial activities during the peak fishing and trading months (26). This means more person-to-person interaction which drives the spread of scabies. It could also be because males are less likely to be concerned with personal cleanliness than females. Compared to females, men tend to take less care of themselves and preserve cleanliness because they are generally less concerned with cleanliness and beauty (27-29).
Although scabies infestation can occur in any age group, it is more common in younger ages (4). In our investigation, children 5 to 14 years were the most affected age group. Persons less than 15 years had up to 5 times the odds of contracting scabies compared to those 15 years and older. This is likely because of greater socialization, personal contact and sharing of personal items within these age groups (30). Similar findings have been reported in Ethiopia, Norway, and Ghana (31-34).
Living with a scabies-infested person increased the odds of contracting scabies. This is likely because sharing a house with an infested person means that there is likely greater physical contact as well as sharing personal items with them (9). In a meta-analysis of 12 studies in Ethiopia in 2020, persons who had contact with a scabies case-patient had higher odds of being infested with scabies compared to those that had no contact with a scabies case patient (9).
Persons who shared three or more personal care items had about three times the odds of being a scabies case patient compared to those that shared two personal items or less. Personal items can spread the scabies mites if these have been in contact with a person who has scabies. Adult mites can exit the stratum corneum, attach to clothing, and live outside the human body for about three days, long enough to transmit scabies (27). In a systematic review of 14 studies in boarding schools in 2020, sharing of personal items was significantly associated with being a scabies case-patient (35). Other studies have reported similar findings (27, 36).
We did not find number of people in the household to be associated with case status. This is in contrast a meta-analysis and systematic review of twelve studies in Ethiopia where there was a 3.1 increased odds of scabies infestation among persons in large family size households compared to smaller family size households (37). This could be because Rwentale Village was a densely populated area hence this exposure is likely similar among the cases and controls.
Limitations
This study had some limitations. First, the assessment of personal hygiene was by self-report. This could have biased the association between scabies case status and personal hygiene toward the null. Secondly, we asked the participants about having had visitors from February to March which could have resulted in imperfect recall. Lastly, we were unable to obtain laboratory confirmation of case-status. This could have led to misclassification bias.
Conclusion
The outbreak in Rwentale landing site village was likely propagated by increased human interaction during the peak fishing and trading months. Sharing personal care items shared, living with an infested person in the same household, being <15 years and being male were associated with case-status. We recommended that community leaders and health workers consider educating communities about scabies transmission, especially during the peak fishing and trading months. The MoH may consider establishing a scabies-specific surveillance system to understand the true magnitude of the problem, and hence plan for appropriate interventions. Finally, mass drug administration of ivermectin may be considered as an effective control measure of scabies in communities with a prevalence of at least 5% (38).
Public health actions
Following the dissemination of our findings, a health sensitization program focused on educating the community about scabies cause, mode of spread, prevention and treatment in collaboration with the community health workers and village heads was conducted.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
We thank the Ministry of Health for permitting us to respond to this outbreak. We thank the Hoima District local government for granting permission and overall guidance to the team.
Copyright and licensing
All material in the Uganda Public Health Bulletin is in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The lancet. 2016;388(10053):1545-602.
- Karimkhani C, Colombara DV, Drucker AM, Norton SA, Hay R, Engelman D, et al. The global burden of scabies: a cross-sectional analysis from the Global Burden of Disease Study 2015. The Lancet infectious diseases. 2017;17(12):1247-54.
- Ahmed AE, Jradi H, AlBuraikan DA, ALMuqbil BI, Albaijan MA, Al-Shehri AM, et al. Rate and factors for scabies recurrence in children in Saudi Arabia: a retrospective study. BMC pediatrics. 2019;19(1):1-6.
- World Health Organisation. Scabies 2020 [Available from: https://www.who.int/news-room/fact-sheets/detail/scabies.
- Engelman D, Cantey PT, Marks M, Solomon AW, Chang AY, Chosidow O, et al. The public health control of scabies: priorities for research and action. The Lancet. 2019;394(10192):81-92.
- Parks T, Smeesters PR, Steer AC. Streptococcal skin infection and rheumatic heart disease. Current opinion in infectious diseases. 2012;25(2):145-53.
- Fischer K, Holt D, Currie B, Kemp D. Chapter 5 – Scabies: Important Clinical Consequences Explained by New Molecular Studies. In: Rollinson D, Hay SI, editors. Advances in Parasitology. 79: Academic Press; 2012. p. 339-73.
- World Health Organisation. WHO Informal Consultation on a Framework for Scabies Control 2020 [Available from: https://apps.who.int/iris/bitstream/handle/10665/333154/9789240008069-eng.pdf.
- Azene AG, Aragaw AM, Wassie GT. Prevalence and associated factors of scabies in Ethiopia: systematic review and Meta-analysis. BMC Infectious Diseases. 2020;20(1):380.
- Ejigu K, Haji Y, Toma A, Tadesse BT. Factors associated with scabies outbreaks in primary schools in Ethiopia: a case-control study. Res Rep Trop Med. 2019;10:119-27.
- NEWS DESK. Scabies outbreak affects more than 1000 in Hoima district, Uganda. Outbreak News Today. 2022.
- URN. Scabies outbreak hits hundreds in Tororo. 2021.
- Mugangha Kolyangha. 250 admitted after scabies outbreak in Pallisa. The Monitor. 2022.
- Okello Emmanuel. Number of People Infested by Scabies Rise to 2000. URN. 2020.
- Okodi D. Abim district battles fresh infestation of scabies. URN. 2020.
- Uganda Bureau of Statistics. Revised Subcounty Population Projections From 2015 To 2030 For 146 Districts 2014 [Available from: https://www.ubos.org/revised-subcounty-population-projections-from-2015-to-2030-for-146-districts/.
- Park HM. Hypothesis testing and statistical power of a test. 2015.
- World Health Organisation. GSHS core questionnaire modules (2021) 2021 [Available from: https://www.who.int/publications/m/item/gshs-core-questionnaire-modules-(2021).
- Naik KR, Srinivasan K, Raviprabhu G, Reddy K, Prameela B. A cross sectional, analytical study of personal hygiene related morbidities of children residing in welfare hostels, Tirupati town, Andhra Pradesh, India. 2020.
- World Health Organization. Thirteenth meeting of the WHO strategic and technical advisory group for neglected tropical diseases, 15-17 September 2020. 2020.
- Ministry of Health. HOIMA DISTRICT Investment Profile 2021 [Available from: https://www.ugandainvest.go.ug/wp-content/uploads/2021/08/Hoima-2021.pdf.
- Amro A, Hamarsheh O. Epidemiology of scabies in the west bank, Palestinian territories (occupied). International Journal of Infectious Diseases. 2012;16(2):e117-e20.
- Haar K, Romani L, Filimone R, Kishore K, Tuicakau M, Koroivueta J, et al. Scabies community prevalence and mass drug administration in two F ijian villages. International journal of dermatology. 2014;53(6):739-45.
- Nazari M, Azizi A. Epidemiological pattern of scabies and its social determinant factors in west of Iran. Health. 2014;2014.
- Rietveld AM, van der Burg M, Groot JC. Bridging youth and gender studies to analyse rural young women and men’s livelihood pathways in Central Uganda. Journal of Rural Studies. 2020;75:152-63.
- Ellis A, Manuel C, Blackden CM. Gender and economic growth in Uganda: Unleashing the power of women: World Bank Publications; 2006.
- Trasia RF. Scabies in Indonesia: Epidemiology and prevention. Insights in Public Health Journal. 2020;1(2):30-8.
- Al-Rifaai JM, Al Haddad AM, Qasem JA. Personal hygiene among college students in Kuwait: A Health promotion perspective. Journal of education and health promotion. 2018;7.
- Kumwenda S. Challenges to hygiene improvement in developing countries: IntechOpen London, UK; 2019.
- Lassa S, Campbell M, Bennett C. Epidemiology of scabies prevalence in the UK from general practice records. British Journal of Dermatology. 2011;164(6):1329-34.
- Wochebo W, Haji Y, Asnake S. Scabies outbreak investigation and risk factors in Kechabira district, Southern Ethiopia: unmatched case control study. BMC research notes. 2019;12(1):1-6.
- Sara J, Haji Y, Gebretsadik A. Scabies outbreak investigation and risk factors in east Badewacho district, Southern Ethiopia: unmatched case control study. Dermatology research and practice. 2018;2018.
- Amato E, Dansie LS, Grøneng GM, Blix HS, Bentele H, Veneti L, et al. Increase of scabies infestations, Norway, 2006 to 2018. Eurosurveillance. 2019;24(23):190020.
- Amoako YA, Phillips RO, Arthur J, Abugri MA, Akowuah E, Amoako KO, et al. A scabies outbreak in the North East Region of Ghana: The necessity for prompt intervention. PLoS neglected tropical diseases. 2020;14(12):e0008902.
- Ismah Z, Fahlepi R, Ayukhaliza DA, Lestari C, Siregar SM. Identify Factors Associated with Scabies Aged 6-19 Years Old in The Boarding School. J-Kesmas: Jurnal Fakultas Kesehatan Masyarakat (The Indonesian Journal of Public Health). 2021;8(2):51-6.
- Marmara D, Mulugeta H, Thygerson S, Ermias A. Scabies among children in Ethiopia. International Journal of Public Health. 2022;11(3):989-97.
- Azene AG, Aragaw AM, Wassie GT. Prevalence and associated factors of scabies in Ethiopia: systematic review and Meta-analysis. BMC infectious diseases. 2020;20:1-10.
- World Health Organisation. Target Product Profiles (TPP) for the development of new diagnostic tools to start and stop mass drug administration for scabies 2022 [Available from: https://www.who.int/publications/i/item/9789240045026.


Comments are closed.