Acute Haemorrhagic Conjunctivitis Outbreak Caused by Enterovirus Type C in Luzira Prisons, Kampala, Uganda, March–April 2024
Authors: Hannington Katumba1*, Charity Mutesi1, Emmanuel Mfitundinda1, Joanita Nalwanga1, Owens Joyce Kobusingye1, Daniel Wenani1, Loryndah Olive Namakula1, Emmanuel Okiror Okello1, Janet Lubega Kobusinge1, Gertrude Abbo1, Annet Mary Namusisi1, Bridget Ainembabazi1, Patrick Kwizera1, Wilfred Opeli2, Winnie Agwang2, Esther Nabatta2, Tracy Rutogire2, Ritah Namusoosa2, Samuel Lugwana2, Richard Migisha1, Benon Kwesiga1, Samuel Gidudu2, Doreen Gonahasa1, Alex Riolexus Ario1; Institutional affiliations: 1Uganda Public Health Fellowship Program-Field Epidemiology Training Program - Uganda National Institute of Public Health, 2Uganda Public Health Fellowship Program-Laboratory Leadership Program - Uganda National Institute of Public Health; Correspondence*: Tel: +256 777 538 911, Email: hkatumba@uniph.go.ug
Summary
Background: On February 25, 2024, an inmate with suspected Acute Haemorrhagic Conjunctivitis (AHC) was remanded at Kampala Remand Prison (KRP) from Kansanga Police Post. A notification was subsequently sent to the Ministry of Health (MoH) on March 7, 2024, having noted a rise in the number of cases to 314 by Mar 6, 2024. We investigated to determine the cause and extent of the outbreak, identify risk factors for its spread and to recommend evidence-based interventions to control the outbreak and prevent future similar outbreaks.
Methods: We investigated the outbreak in 4 prisons of Luzira: KRP, Murchison Bay Prison (MBP), Luzira Upper Prison (LUP), and Luzira Women Prison (LWP). We defined a suspected case as onset of redness in one or both eyes with one or more of the following: tearing, discharge, grainy sensation, itching, pain, or swelling, in a resident Luzira Prison from February 1 to April 3, 2024. A confirmed case was any suspected case with a positive Polymerase Chain Reaction (PCR) result for Enterovirus type C. We found cases through medical records review and active case search among inmates. We collected 10 conjunctival swabs for PCR testing. We calculated the overall and prison-specific attack rates (AR). We assessed the prison environment, case management, and compared 200 cases to 200 controls in a case-control study to evaluate the risk factors. We identified risk factors associated with spread logistic regression.
Results: A total of 1,935 cases were recorded with 4 confirmed to have been caused by Enterovirus Type C and no deaths recorded. The mean age was 30 years (SD=9.4) and the overall AR was 23% (1,935/8,518). The most affected prison was MBP with an AR of 41% (1,229/3,000) followed by KRP at 33% (610/1,835). Infected inmates were continuously admitted into KRP and a plea bargain meeting in KRP attended by inmates from the other prisons triggered the spread of the outbreak in MBP. Cases were being managed through application of Tetracycline Eye Ointment (TEO) and short isolation periods (3 days). Sharing of eye medication (aOR:5.3, CI=2.8-9.9) increased the risk for the spread of infection while frequent handwashing reduced odds of getting AHC (aOR:0.51, CI=0.09-2.8).
Conclusion: Enterovirus Type C was the cause of AHC in this prison setting, introduced by infected inmates. Plea-bargains, and sharing eye medications likely propagated the outbreak. We recommended immediate screening of new arrivals, reporting suspected cases to health facility staff, prompt isolation, and organizing separate plea-bargains to minimize inter-prison interactions, so as to mitigate future risks.
Introduction
Conjunctivitis is a disease characterised by inflammation of the eye mucous membranes, which can be attributed to different aetiologies. These include viral bacterial, allergic, parasitic, and non-specific causes. Despite these many causes, viruses are responsible for about 80% of acute conjunctivitis. Outbreaks of conjunctivitis are mostly attributed to two main groups of viruses (Adenoviruses and Enteroviruses), particularly enterovirus type D (EV70) and Enterovirus type C (Coxsackievirus CVA24), which causes Acute Haemorrhagic Conjunctivitis (AHC)(1) . This disease, commonly known as ‘red eye’ is a is particularly characterized by inflammation and reddening of the eye membranes, pain, tearing, and eye discharge, usually over a short incubation period of 12 to 48 hours.
Acute Haemorrhagic Conjunctivitis (AHC) is more common in tropical regions due to favourable climatic and environmental conditions, such as Uganda. Acute Haemorrhagic Conjunctivitis is highly contagious, spreading rapidly among persons through direct contact, or indirectly through sharing of beddings, clothes, eye glasses, and eye medications. Outbreaks are more common in congested settings such as schools, military barracks, prisons, and refugee camps (2–4).
In Uganda, the first reported outbreak of AHC was in June 2010 in 26 districts (5) followed by another outbreak that occurred in Gulu District in November 2016 among inmates in a prison. Both outbreaks were caused by Coxsackievirus CVA24.
On February 25, 2024, an inmate suspected of having AHC was remanded at Kampala Remand Prison from Kansanga police post. A notification was subsequently sent to the Ministry of Health (MoH) on March 7, 2024. We investigated to determine the cause and extent of the outbreak, identify risk factors for its spread and to recommend evidence-based interventions to control the outbreak and prevent future similar outbreaks.
Methods
Outbreak setting
The outbreak occurred in Luzira Prisons located in Nakawa division in south eastern Kampala, Uganda. It is a prison for both males and females. It is complex of 4 different prisons, namely; Kampala Remand Prison, Murchison Bay Prison, Luzira Upper Prison, and Murchison Bay Women Prison. The prison was initially designed to accommodate 1,700 inmates but currently has close to 8,000 inmates.
Kampala Remand prison is a dynamic prison, meant for 600 inmates, but currently accommodating about 1,840 inmates. Daily, about 250 inmates exit the prison to attend court sessions, some inmates are released from court, and on return new crime suspects are remanded. The prisoners sleep in wards, equivalent to dormitories. The prison has 12 prison wards and one Health Centre (HC) III.
Murchison Bay Prison hosts approximately 3,000 inmates despite its intended capacity being only 600 inmates. It houses the referral hospital (Murchison Bay Hospital) for all Uganda prisons. The referral hospital has a dedicated ophthalmic clinical officer, despite the ophthalmic clinic lacking basic diagnostic tools.
Luzira Upper Prison (maximum security), is designed for inmates with sentences of 20 years or more. By the time of this investigation, the prison had 3,013 inmates. Luzira Women’s Prison in Uganda’s maximum-security prison for females, accommodating 670 at the time of the investigation.
Case definition and case finding
We defined a suspected case as onset of redness in one or both eyes with one or more of the following: tearing, discharge, grainy sensation, itching, pain, or swelling, in a resident Luzira Prison from February 1, 2024 to April 3, 2024. A confirmed case was a suspected case with a positive PCR result positive for Enterovirus type C. We found cases through medical records at the health facilities located within the respective prisons in Luzira. We also actively searched for cases from among inmates with the help of health workers, and the “ward doctor”, who are the equivalent of Village Health Teams (VHTs) at the community level. We then generated a line list.
Descriptive epidemiology
We computed attack rates (AR), stratified by prison based on the population at the time when Azithromycin prophylaxis was administered. We described cases by clinical manifestations, likely exposures, and also constructed an epidemic curve to show the distribution of cases over time.
Environmental assessment
We assessed for factors that could have been associated with the introduction of conjunctivitis into the prisons and its propagation among inmates. We assessed the flow of prisoners, availability, and functionality of handwashing facilities, and isolation of identified cases.
Case management
We assessed how the eye medication was administered and the duration of isolation of identified cases.
Laboratory investigations
We collected 10 samples (conjunctival swabs) from suspected cases and sent them to Uganda Virus Research Institute (UVRI) for Polymerase Chain Reactions (PCR) testing and gene sequencing.
Hypothesis generation
We generated hypotheses from the descriptive epidemiology and hypothesis generating discussions with ‘doctor wards’, health facility staff, and prison officers in charge of welfare and reception, about potential risk factors for transmission of conjunctivitis. The interviews included questions on the flow of prisoners, sleeping next to someone sick, movement outside current prison, isolation of infected inmates, availability of handwashing facilities, administration of eye medication, and receiving visitors.
Case control study
We compared exposures of 200 cases to those of an equal number of controls randomly selected and matched by prison. We defined a control as any resident of Luzira prison with no history of redness in one or both eyes and none of the following signs; eye itching, discharge, swelling, tearing, or discharge since February, 2024 to March 18 2024. Controls were similarly interviewed using the structured questionnaire. We identified possible risk factors associated with spread using logistic regression.
Ethical considerations
This outbreak investigation was in response to a public health emergency. Ministry of Health (MoH) gave administrative clearance to investigate this outbreak. The office of the Centre for Global Health, US Centre for Disease Control determined this investigation to be non-research since its primary intent was public health control of a disease.
Additionally, we obtained administrative clearance from the Uganda Prisons Headquarters before conducting the investigation. We obtained verbal consent from all respondents with guidance of the prison administration. All cases identified during case-finding were referred to the prison health facility staff for further management.
Results
Descriptive epidemiology
A total of 1,935 cases were affected by AHC in all the 4 prisons by April 2, 2024 with no deaths. Of these, 4 were confirmed to be caused by Enterovirus type C. The mean age of case-patients was 30 years (SD=9.4)
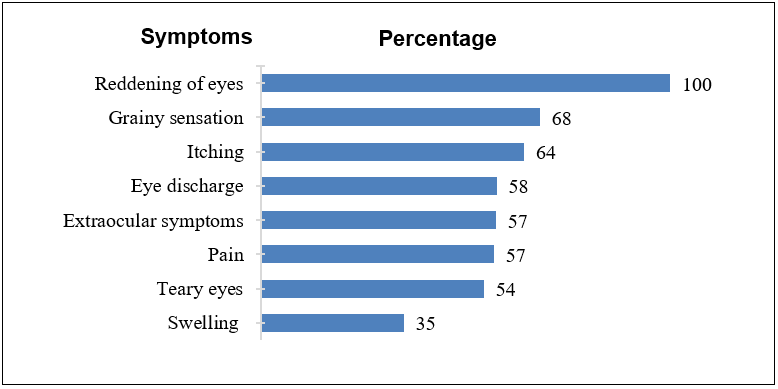
All the case-patients reported having presented with reddening of eyes (Figure 1).
The overall AR was 23% (1,935/8,518), with males being most affected (97%, n=743) compared to females (3%, n=20). Murchison Bay Prison with 1,229 cases (AR: 41/100) was the most affected prison (Table 1).
Table 1: Attack rates by prison during an outbreak of acute haemorrhagic conjunctivitis, Luzira Prison, Kampala, Uganda, February 1- April 2, 2024
| Prison Name | Cases | Total population | Attack rate (AR/100) |
| Murchison Bay Prison | 1,229 | 3,000 | 41 |
| Kampala Remand Prison | 610 | 1,835 | 33 |
| Murchison Bay Women’s Prison | 83 | 670 | 12 |
| Luzira Upper Prison | 13 | 3,013 | 0.4 |
| Total | 1,935 | 8,518 | 23 |
This outbreak started with admission of infected inmates at Kampala Remand Prison from February 28, 2024. The index case was identified by health workers on March 1, 2024. Kampala Remand Prison hosted a plea bargain meeting on March 5, 2024, attended by inmates from Murchison Bay Prison (Figure 2).
This was an event conducted within the confines of specific prisons with legal representatives present, convene inmates from various prisons. Prophylaxis with Azithromycin tablets was administered to inmates on March 8 and 9, 2024. Sharing of topical eye treatments between infected and non-infected inmates started on March 12. On March 15, there was a peak in the number of resident cases. This sharing of eye medication was discontinued on March 19 and inmates’ medication was administered separately by the “doctor ward”. Immediate isolation protocols for newly-admitted inmates were initiated thereafter. Infected inmates continued to be admitted into KRP beyond the time of the investigation (Figure 2), and the overall AR in Kampala Remand Prison was 33/100.
The initial case reported in Murchison Bay Prison involved a prisoner referred to the Prison Hospital on March 1 and 3, who was promptly isolated upon admission. On March 5, a plea bargain meeting convened at Kampala Remand Prison, with attendance from inmates representing Murchison Bay and Upper Prison. Subsequently, cases of conjunctivitis emerged among inmates at Murchison Bay Prison on March 6. As a preventive measure, oral Azithromycin prophylaxis was administered on March 12, followed by the distribution of tetracycline eye ointment (TEO) two days later. TEO served both as prophylaxis for those without symptoms and as a treatment for affected individuals. Despite these interventions, the number of cases steadily increased over time, marked by multiple peaks in incidence (Figure 2).
Starting from March 26, additional public health measures were implemented. These included providing Continuous Medical Education (CME) sessions for healthcare workers and laboratory staff, conducting health talks for inmates, and promptly isolating and treating identified cases upon detection. These public health measures preceded a noticeable decline in the number of reported cases (Figure 2).
Women’s Prison Luzira
The index case here was identified on March 16, 2024, as an inmate who attended court 2 days earlier (March 14, 2024), and reported to have shared a bus with an infected inmate from Murchison Bay on her way and from court (Figure 2).
Luzira Upper Prison
The data obtained from Luzira Upper Prison indicated that cases of conjunctivitis were routinely recorded in the health facility records. The first suspected case of AHC was detected on March 11 (Figure 2).
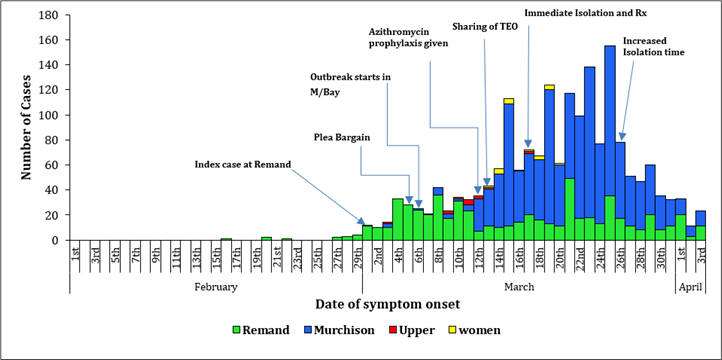
Overall, the outbreak in Murchison Prison was preceded by that in Remand Prison, and by April 3, a total of 1,935 suspected cases had been reported to the prison health facilities (Figure 2).
Environmental and case management assessment findings
Kampala Remand Prison every day transports 150 – 200 inmates to attend different court sessions. In contrast, the maximum-security prison (Upper prison) transports an average of 80 inmates to courts daily and these are usually to different courts from those which inmates from both Kampala remand and Murchison Bay prison go to.
Some inmates are released from court, while at the same time, new inmates are remanded. Murchison Bay Prison receives prisoners referred from other prisons for medical attention at Murchison Bay Prison hospital. There was a plea bargain session at Remand prison where some inmates from Murchison Bay attended.
We observed the presence of tap and tank water at the gate and at entry points of the prison wards. Some handwashing points both soap and water while others had only water. In some prison wards, water was pre-mixed with liquid soap.
In the earlier days of the outbreak, cases were isolated and treated. Later, the number of cases were so high that isolation was no longer possible. Identified cases were treated from the prison wards where inmates resided. Treatment was being administered topically by the “doctor ward” using their hands to all inmates in spite of the disease status of the inmates. This was not observed in both the Upper prison and the women’s prison. By this time, only those that had severe eye discharges were isolated. Isolation initially lasted only up to 3 days in Murchison Bay prison. However, in upper prison, isolation was sustained until prisoners recovered fully from the infection.
Hypothesis generation findings
Based on the laboratory and the environmental assessment findings, we hypothesized that receiving Azithromycin prophylaxis helped prevent development of new cases among inmates. Sharing eye medication was associated with propagation of the outbreak among inmates. Poor hand hygiene was associated with increased transmission of AHC among inmates.
Case control investigation findings
We noted that sharing of eye medication (aOR:8.3, CI:3.8-18) was significantly associated with acquiring the infection among inmates, while more frequent hand washing reduced the odds of getting conjunctivitis (aOR:0.11, CI:0.03-0.37). Notably, there was no difference in odds between those who received Azithromycin prophylaxis and those who did not (aOR:0.4, CI:0.34-5.8) (Table 2).
Table 2: Factors associated with acute haemorrhagic conjunctivitis among inmates during an outbreak, Luzira prisons, Uganda, March–April 3, 2024
Discussion
This investigation confirmed an outbreak of AHC in Luzira Prison among inmates, attributed to Enterovirus Type C. The outbreak primarily affected Murchison Bay Prison, initially spreading from Remand Prison. Despite prophylactic antibiotic administration, new cases continued to arise. In the Women’s Prison, the outbreak originated from an index case who shared a bus with an infected inmate from Murchison Bay on their way to court. Sharing eye medications increased the odds of conjunctivitis among Luzira Prisons inmates.
The outbreak was attributed to Enterovirus type C, and this is consistent with other findings from other outbreak findings indicating that Enteroviruses EV70 and CA24V are responsible for most AHC outbreaks (2,6–9). It was observed that cases resolved within a span of 4-5 days with no severe complications documented. Our findings do not differ from students in a resident school that suffered from AHC and averagely spent 6 days unwell (3).
The variation in attack rates among prisons can be attributed to the distinct operational and functional characteristics of each facility. Remand Prison, for instance, experiences a continuous influx of new inmates from various police cells and courts of law on a daily basis, with remanded individuals frequently leaving to attend court hearings. This dynamic environment likely contributed to the initial case and the ongoing spread of conjunctivitis within the prison.
The outbreak in Murchison Bay Prison ensued following the outbreak in Remand Prison, potentially attributed to inmates from Murchison Bay participating in a plea-bargain meeting held at Kampala Remand Prison. These gatherings, conducted within the confines of specific prisons with legal representatives present, convene inmates from various prisons. The close proximity and crowding inherent in these assemblies likely facilitated disease transmission from infected individuals in Remand Prison to those in Murchison Bay, underscoring the significant role such events play in propagating illness within carceral environments. To mitigate the risk of future outbreaks, prison authorities could consider implementing screening measures for Acute Hemorrhagic Conjunctivitis (AHC), thereby excluding affected individuals from participation in such assemblies including plea-bargain meetings (10).
Upon the outbreak’s emergence, the prison administration swiftly implemented control measures, including the prophylactic administration of antibiotics like Azithromycin and Tetracycline Eye Ointment. However, these measures failed to curb the outbreak’s spread; laboratory samples later confirmed the causative agent to be a virus. Notably, the administration of eye medication (Tetracycline Eye Ointment and Chloramphenicol) may have inadvertently facilitated the outbreak’s propagation among inmates. Prison ward leaders referred to as “doctor wards,” were administering eye medication to infected and non-infected inmates alike, using the same tubes and initially applying TEO directly to inmates’ eyes with their hands. This direct contact likely propagated the outbreak’s spread from infected to uninfected inmates. Sharing eye medications has been demonstrated to propagate outbreaks of conjunctivitis. Additional data highlight increased risk of AHC spread through sharing topical eye treatments, emphasizing the need to discourage such practices (10, 11). Given these findings, it is imperative to minimize contact between infected and non-infected inmates. Implementing screening protocols and promptly isolating and treating individual cases are pivotal steps in mitigating the rapid spread of infection within prison settings.
Initially, all identified cases were isolated. However, as the number of cases grew substantially, it became impractical to isolate every individual until recovery due to space constraints. The prison’s capacity is already stretched, being approximately 300% over its initial design capacity for inmates. Consequently, isolation was restricted to individuals exhibiting symptomatic signs, with a limited duration of 3 days or less. After this period, sick inmates were returned to their respective prison wards. The remaining cases were managed within the overcrowded wards, leading to unavoidable close contact between infected and unaffected inmates. Sleeping close to infected inmates and subsequent sharing blankets among inmates was associated with increased odds of developing AHC. This concurs with other studies in Brazil, USA and China, where AHC spreads through sharing fomites with infected persons (10–13).
Particularly in Kampala Remand Prison, it was commonplace for inmates to be released even after less than a week of incarceration, and “doctor wards” are not exempt. This rapid turnover posed challenges for trained personnel in identifying cases, reporting them, and administering eye medication effectively. Many trained individuals were released shortly after their training, leaving insufficient time to adequately train and orient new staff. Consequently, there was significant variability in the application of eye medication by different personnel within the prison.
Despite this issue, we observed that there was sufficient provision of handwashing stations throughout the prisons. Our findings indicated that frequent handwashing was beneficial in mitigating the spread of infection. Frequent hand washing with soap and water prevented infection spread, consistent with findings from previous studies conducted in the USA and India (6,11–13).
Study limitations
The main limitation of this investigation pertains to the scope of our study, as we were unable to provide a comprehensive depiction of the outbreak’s evolution and scope across various prisons. Our focus was primarily on the outbreak within the Luzira prisons, and thus, we did not explore potential clusters in other prison facilities or communities (e.g., schools). Consequently, we cannot definitively determine whether these clusters were epidemiologically linked to the outbreak in Luzira prisons. The absence of such epidemiological insights limits our ability to develop evidence-based control measures more effectively.
Conclusion
In conclusion, our investigation confirmed Enterovirus type C as the causative agent of the conjunctivitis outbreak in Luzira Prison. The outbreak exhibited varying impacts across the different prisons, with Kampala Remand Prison being the most affected. This can be attributed to its dynamic nature, where inmates are regularly discharged and new ones are detained from various police cells and courts on a daily basis. The outbreak in Murchison Bay was a spill-over from Remand Prison owing to prisoner mixing during a plea-bargain mass meeting. Despite the prophylactic administration of antibiotics during the outbreak, the viral nature of the infection hindered the desired effect of preventing further transmission among inmates. Sharing of topical eye medication contributed to the rapid propagation of conjunctivitis among inmates. While frequent hand washing reduced risk of getting the infection.
Public health actions
During our investigation, we conducted sensitization sessions for inmates on the importance of proper hand hygiene. We also provided training for “doctor ward” on the correct administration of eye ointments and drops, emphasizing the need to promptly report and refer suspected cases to health facilities. We discussed and worked closely with prison administration and health facility staff to implement immediate measures. All cases identified during case-finding were referred to prison health facility staff for further management. Following the dissemination of our findings, the isolation time was increased from 3 days to 5-7 days.
Continuing medical education (CME) sessions were conducted for healthcare workers, and clinical and laboratory staff were trained on sample collection, storage, and referral procedures. An assessment of prison laboratory capacity for outbreak readiness was conducted by the LLP team, and recommendations for improvement were provided to prison authorities and partners.
To disseminate our findings, a preliminary report of the findings was presented to the Uganda Prison Services Headquarters and the Public Health Commission.
Recommendations
We recommend that communal events such as plea bargain could in future be held for each individual prison to prevent transmission of disease from one prison to another.
We also recommend a strong emphasis on personal hand hygiene; water and soap, preferably pre-mixed, should be made readily available at all possible hand washing points throughout the prisons.
Mass prophylactic administration of antibiotics may be considered only when a bacterial cause has been confirmed.
On entry, all inmates would better be screened for signs conjunctivitis, and the identified cases promptly reported to the health facility and isolated, for at least 5 days. In Murchison Bay and Women’s prison, new inmates could be quarantined for 5 days before they are made to mix with other inmates.
We further recommend separation of topical eye medication between infected and non-infected inmates, coupled with continuous surveillance and reporting suspected cases to health facility staff.
Finally, the prison authorities could consider appointing “Dr Wards” who are convicts, especially in Kampala Remand Prison. This is because of the high turnover of inmates, where by a “doctor ward” is likely to be released after a short duration of incarceration, meaning a new “doctor ward” has to be trained in surveillance and reporting of cases on his ward.
Conflict of Interest
The authors declared no conflict of Interest
Author Contribution
All authors participated in investigation, design of data collection and entry tools and cleaning and review of the bulletin draft. HK led the investigation team and took the lead in drafting the bulletin. CM, EM, LON, and BA participated in data analysis. RM, BK, DG and SG supervised the outbreak investigation and reviewed the bulletin draft to ensure intellectual content and scientific integrity. RM, BK, and ARA reviewed the final bulletin for intellectual content and scientific integrity.
Acknowledgements
We extend our sincere gratitude to the Kampala Capital City Authority/Kampala Metropolitan Area Emergency Operations Center team for their prompt notification to the Ministry of Health, facilitating swift response measures. We also wish to express our appreciation to Dr Aida Ajambo and the entire Public Health Commission of the Uganda Prison Service for their exemplary coordination efforts and responsive administrative support, enabling us to access the inmates effectively.
Copyright and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Wright PW SG. Acute Viral Conjunctivitis. Am Fam Physician. 1992;
- Madurapandian Y, Rubeshkumar P, Raju M, Janane A, Ganeshkumar P, Selvavinayagam TS, et al. Case report: An outbreak of viral conjunctivitis among the students and staff of visually impaired school, Tamil Nadu, India, 2020. Front public Heal [Internet]. 2022 Aug 5 [cited 2024 Apr 5];10. Available from: https://pubmed.ncbi.nlm.nih.gov/35991078/
- Crum NF, Barrozo CP, Chapman FA, Ryan MAK, Russell KL. An outbreak of conjunctivitis due to a novel unencapsulated Streptococcus pneumoniae among military trainees. Clin Infect Dis [Internet]. 2004 Oct 15 [cited 2024 Apr 5];39(8):1148–54. Available from: https://pubmed.ncbi.nlm.nih.gov/15486838/
- Martin M, Turco JH, Zegans ME, Facklam RR, Sodha S, Elliott JA, et al. An outbreak of conjunctivitis due to atypical Streptococcus pneumoniae. N Engl J Med [Internet]. 2003 Mar 20 [cited 2024 Apr 5];348(12):1112–21. Available from: https://pubmed.ncbi.nlm.nih.gov/12646668/
- Ayoub EA, Shafik CF, Gaynor AM, Mohareb EW, Amin MA, Yassin AS, et al. A molecular investigative approach to an outbreak of acute hemorrhagic conjunctivitis in Egypt, October 2010. Virol J [Internet]. 2013 [cited 2024 Apr 5];10. Available from: https://pubmed.ncbi.nlm.nih.gov/23531270/
- Tavares FN, Costa E V., Oliveira SS, Nicolai CCA, Baran M, Da Silva EE. Acute hemorrhagic conjunctivitis and coxsackievirus A24v, Rio de Janeiro, Brazil, 2004. Emerg Infect Dis. 2006;12(3):495–7.
- Boro P, Gongo T, Ori K, Kamki Y, Ete N, Jini M, et al. An outbreak of acute hemorrhagic conjunctivitis due to Coxsackievirus A24 in a residential school, Naharlagun, Arunachal Pradesh: July 2023. Indian J Med Microbiol. 2024;48(February).
- Nakwire L. Acute hemorrhagic conjunctivitis outbreaks caused by coxsackievirus-a24 in three prisons gulu district uganda 2017 [Internet]. Available from: https://uniph.go.ug/acute-hemorrhagic-conjunctivitis-outbreaks-caused-by-coxsackievirus-a24-in-three-prisons-gulu-district-uganda-2017/
- (CDC) C for DC and P. Notes from the field: acute hemorrhagic conjunctivitis outbreaks caused by coxsackievirus A24v — Uganda and southern Sudan, 2010. MMWR Morb Mortal Wkly Rep [Internet]. 2010 [cited 2024 Apr 2];59(32):1024. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5932a4.htm
- CDC. Preventing Pink Eye (Conjunctivitis) [Internet]. National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases. 2019 [cited 2024 Apr 3]. Available from: https://www.cdc.gov/conjunctivitis/about/prevention.html
- de Mesquita Costa CC, e Sá LHS, Mendes LP, Júnior RLC, da Rocha CS, Santos MB, et al. Outbreak of acute conjunctivitis in the eriod 2017-2018 in Recife, Brazil. Rev Bras Oftalmol [Internet]. 2021 Apr 21 [cited 2024 Apr 3];80(1):12–6. Available from: https://www.scielo.br/j/rbof/a/CH96cMxSTjw6mpHwMn7x53v/?format=html&lang=en
- Weir E. Weep, oh mine eyes: An outbreak of bacterial conjunctivitis. C Can Med Assoc J. 2002;166(10):1305.
- Liu J, Zhang H. Epidemiological Investigation and Risk Factor Analysis of Acute Hemorrhagic Conjunctivitis in Huangshi Port District, Huangshi City. Hindawi Comput Math Methods Med [Internet]. 2022 [cited 2024 Apr 3];2022. Available from: https://doi.org/10.1155/2022/3009589


Comments are closed.