Achievements and Lessons Learned from the First Oral Cholera Vaccination in Uganda, July 2018
Author: Dativa Maria Aliddeki1*, Immaculate Ampeire2, Bernard Toliva Opar2, Henry Luzze2, Doreen Birungi1, Joyce Nguna1, Daniel Kadobera1, Alex Riolexus Ario1; Affiliations: 1. Uganda Public Health Fellowship Program, Kampala, Uganda, 2. UNEPI, Ministry of Health, Kampala, Uganda
Summary
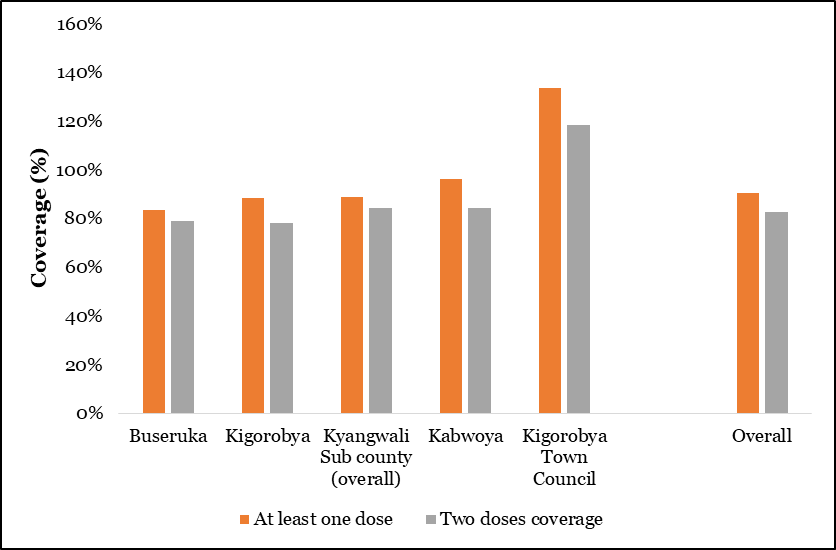
On 23 February 2018, Ministry of Health (MoH) Uganda declared a cholera outbreak in Hoima District coinciding with a level 3 humanitarian emergency in Uganda linked to areas in DRC that were experiencing active cholera outbreaks. Uganda implemented a comprehensive strategy to respond to this outbreak which included; provision of safe water; improvement of sanitation, health education, strengthening disease surveillance, among others. To further strengthen cholera prevention, Uganda conducted two reactive mass oral cholera vaccination campaigns in five hotspot sub-counties of Hoima District. A 97% coverage was achieved in round 1, followed by a 90% coverage in round 2 of the campaign. Of the 367,899 people targeted for vaccination, 305,065 received 2 doses of OCV, representing an 83% proportion of people fully protected from Cholera, for the next 3 -5 years in known cholera out break hotspots in Hoima District.
Background
On 15 February 2018, Ministry of Health (MoH) Uganda was alerted of a cholera out break in Hoima District which coincided with a Level3 humanitarian emergency in the Democratic Republic of Congo (DRC). This led to an influx of over 22,000 refugees into Uganda from areas in DRC that were experiencing active cholera outbreaks. MoH declared a cholera outbreak in Hoima District on 23rd February 2018. Uganda implemented a comprehensive strategy to respond to this outbreak including provision of safe water and improvement of sanitation, health education, strengthening disease surveillance, among others. To strengthen cholera prevention, Uganda planned reactive and proactive mass oral cholera vaccination campaigns in a phased manner, starting with Hoima District. The main objective was to reduce transmission and mortality due to cholera in hotspots of Hoima District by achieving 95% coverage of the target population.
Implementation strategy
We received 360,650 doses of OCV and planned a two round reactive vaccination campaign. We targeted 96% of the total population, i.e. all persons aged 1 year and above, in the five hotspot sub-counties of Kigorobya Town Council, Kigorobya, Buseruka, Kabwoya and Kyangwali. We used a combination of house to house house/mobile and static strategies. Round 1 was held from 2nd to 6th May 2018 and round two, from 27th June to 1st July 2018. We trained and deployed a teams of 15 national supervisors who worked with the district to plan and train the supervisors at district, sub-county, parish level and health workers. We trained district leaders and Village Health Teams (VHTs) to conduct community social mobilization. We deployed 3 person teams i.e. a health worker, health inspector and a VHT to vaccinate household members, conduct WASH assessments and conduct sensitization in each village. The parish supervisors provided daily logistics and also summarized vaccination data. Sub-county supervisors maintained functionality of the cold chain and distributed vaccines at all service points while district and central level supervisors provided overall support Achievements: A 97% coverage was achieved in round 1 and 90% coverage was achieved in round 2. Among the people vaccinated, 83% (305,065/367,899) received a second dose of the OCV, there by representing a proportion of the target population that is fully protected for the next 3 – 5 years ( Figure 1).
Lessons Learned
Planning: Involving the lowest level of the community comprehensively in bottom up planning strategy high lighted strategies for hard to reach populations in institutionalized settings like prisons. This prioritized populations in most need ( i.e. high risk communities in the five sub-counties identified as cholera hotpots) for phase 2 of the OCV roll out . The demand driven nature of the OCV campaign overwhelmed the vaccination teams in round one of the campaign.
Coordination: Supervision at parish, sub-county, district and national level with support from an international consultant provided a well planned , coordinated and quality assured vaccination campaign.
Funding
The MOH made timely transfer of funds to the district, which has been a challenge for past vaccine activities, for planning this vaccination campaign.
Cold-chain and logistics: The Euvichol PlusTM, a bivalent whole cell killed oral cholera vaccine, is given in 2 doses, with a minimum interval of 2 weeks not beyond 6 months. The 1.5ml plastic single dose vials packages limit wastages. It is also remains stable outside the cold chain up to 42°C (2,3). The bulk used in this campaign made proper waste disposal difficult for the static teams, due to the high turn up at the vaccination sites.
Social mobilization: We used mobile mega phones in fishing and refugee communities and found it more effective in comparison to radio announcements. Community level dialogues in resistant communities enabled participation in the campaign. Political involvement played a critical role in social mobilization during round 1 of the campaign. Local Council 5 Chairman, receive the vaccine first during the district launch of the OCV.
Surveillance
The vaccination teams conducted active case search at household level . This enabled household active case search. And immediate reporting of any new cases. This provided opportunity to build capacity of the Village Health Teams in cholera surveillance. Integrating of WASH in the OCV campaign: The campaign teams assessed and strengthen the Water, Sanitation and Hygiene (WASH) practices . This created opportunity for household sensitization, a strategy to be emulated in subsequent campaigns which are known to register only 65% protection against cholera (3).
Conclusion
In light of the planned phase 2 of OCV roll out in other hotspot districts, it is pertinent that the country builds on the experiences of phase 1 of the introduction to inform the implementation process. The program will have to compare the reactive and proactive contexts of OCV vaccination campaigns and develop guidelines for OCV use in the country.
References
1. WHO | Lessons learnt from 12 oral cholera vaccine campaigns in resource-poor settings [Internet]. WHO. [cited 2018 Sep 30]. Available from: http://www.who.int/bulletin/volumes/95/4/16-175166/en/
2. Luquero FJ, Grout L, Ciglenecki I, Sakoba K, Traore B, Heile M, et al. Use of Vibrio cholerae Vaccine in an Outbreak in Guinea. N Engl JMed. 2014 May 29;370(22):2111–20.
3. Final CHOLERA GUIDELINES 2017.pdf [Internet]. [cited 2018 May 17]. Available from: https://reliefweb.int/sites/reliefweb.int/files/resources/Final%20CHOLERA%20GUIDELINES%202017.pdf


Comments are closed.