A cluster of COVID-19 at a secondary hospital, Kampala, Uganda, during phase four of the epidemic
Quarterly Epidemiological Bulletin: January -March, 2021 Volume 6 / Issue 1/Article No. 2 Authors: Elizabeth Katana1, 2, Alex Ndyabakira1, 2, Aggrey Byaruhanga1, Daniel A. Okello2, Ivan Kimuli4, Maureen Kesande3, Daniel Kadobera1 1Uganda Public Health Fellowship Programme, Kampala, Uganda. || Affiliation: 2Directorate of Public Health and Environment, Kampala Capital City Authority (KCCA), Kampala, Uganda, 3Infectious Diseases Institute, Kampala, Uganda, 4Makerere University Lung Institute, Kampala, Uganda.
Summary
As of August 03, 2020, Uganda had confirmed 1,203 cases with 5 deaths and several health workers had been confirmed with a cumulative total of 250. Following the reports of several clusters of cases at hospitals in Kampala, we described the cases of COVID-19 identified at a secondary hospital in Kampala during phase 4 of the epidemic. We conducted a descriptive study of cases that had a confirmed PCR positive test for COVID-19 at a secondary hospital in Kampala, August 19, to September 15, 2020. We described cases by demographic characteristics, symptoms, mortality, and distribution of overtime. Of the 32 confirmed cases, whose mean age was 39.1, ranging from 20 to 72 years, majority 21 (66%) were males, 25 (78%) were asymptomatic, 16 (50%) health workers, 17 (53%) were either health workers rotating in the ICU or patients admitted in the ICU at the time of sample collection, and mortality was 6%, occurring in the ICU. An equal proportion of health workers and patients were confirmed positive for COVID-19 at the hospital in the one-month period. Most cases were asymptomatic and either health workers rotating in the Intensive Care Unit (ICU) or patients admitted in the ICU at the time of sample collection. We recommended enforcement of Standard Operating Procedures (SOPs), continued surveillance and vigilance in the most at-risk hospital departments including the ICU.
Introduction
On March 11, 2020, COVID-19 was declared a global pandemic. As of August 03, 2020, Uganda had confirmed 1,203 cases with 5 deaths and several health workers had been confirmed with a cumulative total of 250. Initial health worker COVID-19 infections were first detected in May 2020 at Lira Hospital and the infection has since affected several health workers all over the country with many clusters and the highest numbers reported from Kampala hospitals(1). Following reports of several clusters of cases at hospitals in Kampala, we described the cases of COVID-19 identified at a secondary hospital and documented the response strategies undertaken by the hospital during phase 4 of the epidemic.
Methods
We conducted a descriptive study using both quantitative and qualitative approaches at a high-volume secondary hospital in Kampala, offering specialised services including general surgery, paediatrics, obstetrics, intensive care, and other supporting medical services. We defined a confirmed case as any health worker or patient that had a confirmed PCR positive test for COVID-19 at the secondary hospital from August 19, to September 15, 2020. We reviewed health facility records and collected data on COVID-19 symptom status, sex, age, date and site of sample collection at the hospital, date of COVID-19 test confirmation and the patient or health worker status. We also conducted Key Informant interviews with the hospital staff including management, made observations at the hospital, and generated information on the response strategies. We described cases by demographic characteristics, symptoms, mortality, distribution of overtime, and response strategies were performed. Content analysis was used to summarise findings from the interviews.
Results
Descriptive characteristics of confirmed COVID-19 cases at a secondary hospital in Kampala, August – September 2020
We identified 32 confirmed cases at the secondary hospital from August 19, to September 15, 2020. Of the 32 confirmed cases, whose mean age of was 39.1, ranging from 20 to 72 years, majority 21 (66%) were males, 25 (78%) were asymptomatic, 16 (50%) health workers, 17 (53%) were either health workers rotating in the Intensive Care Unit (ICU) or patients admitted in the ICU at the time of sample collection, and 2 (6%) were deceased, with the death occurring in the ICU.
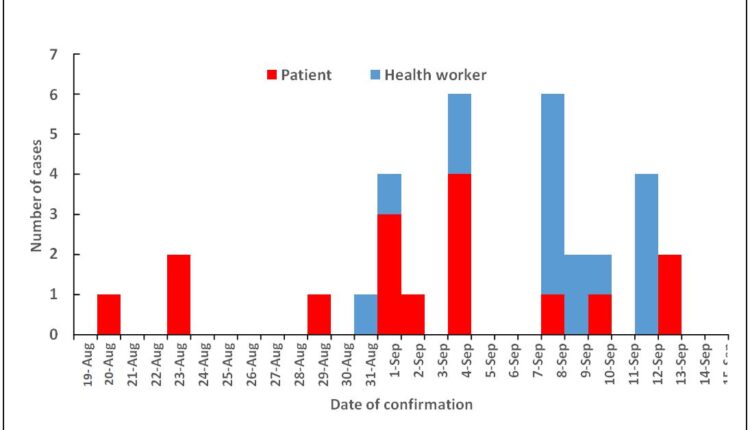
The outbreak started on August 20, 2020, almost three months after the first health worker in Uganda had been confirmed positive at Lira hospital in May 2020. The index case was a symptomatic patient who was seen and tested from the emergency room of the secondary hospital on August 19, 2020. COVID-19 was suspected in the emergency room and the sample was collected immediately. The index case was isolated at the secondary hospital before being referred to a tertiary facility after COVID-19 confirmation. None of the 31 cases was a contact to the index case. Almost two weeks later, on August 31, the first health worker was tested and confirmed positive from the wards of the secondary hospital. More health workers tested positive in the subsequent days with cases peaking between September 8th and 14th and predominantly from the ICU, though none of them was a contact to the first confirmed health worker (Figure 1).
Through interviews and observations, we documented the following strategies implemented by the hospital in response to the COVID-19 Outbreak
Establishment of a COVID-19 task force: This was set up at the hospital to oversee COVID- 19 related functions including Personal Protective Equipment (PPE) usage and stocks, facility-based contact tracing, maintaining the surveillance system including temperature checks and symptom monitoring, trainings for health workers, mandatory testing, and adherence to the Standard Operating Procedures (SOPs).
Minimising of staff rotation between hospital departments: The same group of health workers routinely rotated between the hospital departments. Predominantly, one group rotated between the ICU, and theatres while another between the out and inpatient departments. The hospital to review the rotation strategy in a way that reduced rotation of health workers between departments for at least a period of 3 weeks and enforce testing before rotations to other departments. Of note, some of the health workers took shifts in other city hospitals which made these efforts difficult.
Enforcement of mask use and physical distancing procedures at the hospital: Through observation, physical distancing was a challenge at the facility due to very limited waiting space at the OPD, nevertheless physical markings were put on seats to minimise crowding. Some health workers and patients were observed wearing masks incorrectly, a team of health workers on the hospital COVID-19 task force was assigned with ensuring compliance to mask use by both health workers and patients. The cafeteria being small, the health workers were encouraged to take their meals in shifts that could allow fewer people into the cafeteria at every hour.
Closure of the ICU: The ICU was deep cleaned, fumigated, and closed for two weeks, patients requiring intensive care were referred to Mulago National Specialised Hospital. Enforcement of adherence to SOPs in other departments including the theatre was ensured.
Infection Prevention and Control (IPC) trainings: A dedicated IPC committee with representatives from all the hospital departments was formulated and weekly IPC trainings for all the health workers were initiated. The trainings focused on ensuring that the health workers were routinely equipped with knowledge on the standard and required practices with regards to the COVID-19 preventive measures including hand washing, physical distancing, and mask use. The trainings also covered general IPC practices that should be observed in specific departments including the ICU, theatre, and wards. They also covered other general hospital IPC practises including waste management and disposal, quality control, scrubbing and draping, among others.
Mandatory COVID-19 testing: A test and treat policy was initiated for all the patients requiring an admission regardless of symptom status with the sample collection done by the hospital and the testing costs met by the patients while all health workers were required to test bi weekly with the costs met by the hospital management. The hospital developed a partnership with a COVID-19 testing laboratory to offer testing at a subsidised fee.
Immediate referral of confirmed COVID-19 cases: Upon confirmation of a positive PCR test for COVID-19 infection, cases including health workers were referred to a tertiary hospital for COVID-19 management.
Contact tracing and listing: a team on the hospital COVID-19 task force was entrusted with ensuring contacts were listed and traced with assistance from the surveillance teams from KCCA and MOH. However, it was noted that, given the high volume of patients seen at the hospital as well as movement and rotation of patients and staff between departments, and immediate referral of confirmed cases to tertiary hospital, it was difficult to list and test all the possible contacts of a confirmed case.
Discussion
Our investigation showed that an equal proportion of patients and health workers were confirmed positive in the one month. This is in agreement with previous assessments that have shown that the COVID-19 pandemic has placed a huge burden on hospitals globally with increased risk of nosocomial transmission and outbreaks to “non COVID” patients or residents including caretakers and health workers in hospitals(2).
The index case was asymptomatic patient seen in the emergency room of the secondary hospital. An investigation of an outbreak of COVID-19 in a South African hospital that also started in the emergency room found that it was due to lack of a separation between COVID-19 infected patients and other patients, low suspicion and awareness of the threat and frequent movements of both the patients and health workers within the hospital(3). After this outbreak occurred, the secondary hospital increased its vigilance with implementation and adherence to SOPs between staff and patients.
None of the subsequent cases had been listed as a contact to the index case. This could have resulted from the immediate referral of the index case to a tertiary hospital upon confirmation as COVID-19 positive and the frequent rotation of staff between hospital departments that made it difficult to trace all possible contacts to a confirmed case.
Rotation of health workers in the hospital departments posed a challenge to the outbreak response and also some could have been exposed from outside the hospital including working shifts in other hospitals around Kampala. Therefore, from our investigation, it was unclear if these were community or hospital acquired infections.
Most of the confirmed cases were either working or admitted in the ICU and all the deaths occurred in the ICU. Researchers have shown that ICUs are associated with a greatly increased risk of nosocomial infections and also the risk of occupationally acquired infections among health workers is highest, among ICU personnel(4). In addition to this, the ICU is where the most vulnerable patients are kept and also the most invasive procedures including mechanical ventilation are done(5).
Most of the confirmed cases were asymptomatic and had only been tested as contacts in response to the outbreak at the hospital. Similar to this, an outbreak investigation of COVID- 19 among hospital food service workers in USA found that the index case had continued working at the hospital with mild respiratory symptoms and serial asymptomatic testing had to be done to identify the additional cases(6).
Mandatory testing of all the patients prior to admission at the hospital and routine testing all health workers was adopted by the hospital. Expanding testing criteria to include widespread testing of patients, caretakers, and health workers regardless of presence of symptoms has been credited as being crucial in the response to viral respiratory outbreaks including SARS-COV-2(2). This outbreak highlights the importance of continued vigilance in the most at-risk areas within hospitals including ICUs and emergency rooms, and prompt implementation and monitoring of adherence to the recommended COVID-19 SOPs.
Limitations
Given the nature of the study design (a descriptive study), without analytical approaches, we were not able to establish why the outbreak occurred or how it came to be. However, this study casts light on the problems that can be faced by secondary hospitals in future similar outbreaks.
Conclusion
An equal proportion of health workers and patients were confirmed positive for COVID-19 at the hospital in the one-month period. Most cases were asymptomatic and either health workers rotating in the Intensive Care Unit (ICU) or patients admitted in the ICU at the time of sample collection. We recommended enforcement of Standard Operating Procedures (SOPs), continued surveillance and vigilance in the most at-risk hospital departments including the ICU.
References
- MOH, Uganda. Press Release Archives [Internet]. COVID-19 | Ministry of Health. [cited 2021 Apr 5]. Available from: https://health.go.ug/covid/category/press-release/
- Abbas M, Robalo Nunes T, Martischang R, Zingg W, Iten A, Pittet D, et al. Nosocomial transmission and outbreaks of coronavirus disease 2019: the need to protect both patients and healthcare Antimicrob Resist Infect Control. 2021 Jan 6;10(1):7.
- Hospital outbreak of COVID-19 in South Africa [Internet]. The Centre for Evidence-Based [cited 2021 Mar 28]. Available from: https://www.cebm.net/study/covid-19- hospital-outbreak-of-covid-in-south-africa/
- Maki DG, Crnich CJ, Safdar N. Nosocomial Infection in the Intensive Care Unit. Crit Care 2008;1003–69.
- Infection Control in the ICU [Internet]. Infection Control [cited 2021 Mar 28]. Available from: https://www.infectioncontroltoday.com/view/infection-control-icu
- Hale M, Dayot A. Outbreak investigation of COVID-19 in hospital food service workers. Am J Infect Control. 2021 Mar;49(3):396–7.
Reference this page as below
Elizabeth Katana1, 2, Alex Ndyabakira1, 2, Aggrey Byaruhanga1, Daniel A. Okello2, Ivan Kimuli4, Maureen Kesande3, Daniel Kadobera1. A cluster of COVID-19 at a secondary hospital, Kampala, Uganda, during phase four of the epidemic. Kampala. Uganda National Institute of Public Health. 2021 March 30th. Available from:https://uniph.go.ug/a-cluster-of-covid-19-at-a-secondary-hospital-kampala-uganda-during-phase-four-of-the-epidemic.


Comments are closed.