Trends and distribution of maternal sepsis, Uganda, 2018-2022
Authors: Lawrence Tumusiime¹*, Edith Namulondo¹, Benon Kwesiga¹, Richard Migisha¹, Daniel Kadoberaᶾ, Irene Mwenyango², Robert Mutumba², Richard Mugahi², Alex Riolexus Ario¹; Institutional affiliations: ¹Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala Uganda; ²Reproductive Health Department, Ministry of Health, Kampala, Uganda; Correspondence*: +256779712458, ltumusiime@uniph.go.ug
Summary
Background: Maternal sepsis (MS) is a pregnancy-related life-threatening condition that occurs after infection during pregnancy, childbirth, after delivery, or after an abortion. In low-income countries, MS causes 10% of preventable maternal deaths. In 2016, MS caused 13% of maternal deaths in Uganda. In 2019, the Ministry of Health set a target of reducing the proportion of sepsis-attributable maternal deaths to 8% by 2024. We assessed the trends and distribution of maternal sepsis incidence, maternal deaths attributable to sepsis, and maternal sepsis case-fatality rate, Uganda, 2018-2022, to inform programming.
Methods: We calculated MS cases per 10,000 live births per year from 2018–2022 at district, regional, and national levels, using the District Health Information System version 2 (DHIS2) data, 2018–2022. We also calculated MS deaths per 100 maternal deaths, and MS deaths per 100 MS cases. The Mann-Kendall test was used to evaluate the significance of linear trends.
Results: Overall, 24,285 new MS admissions were reported from 2018–2022. The national MS incidence was 43/10,000 live births, with the Acholi region being the most affected (71/10,000). MS rates declined from 48/10,000 live births in 2018 to 37/10,000 in 2022 (p=0.02). Significant regional declines occurred in 6 (Kigezi, Tooro, North central, South central, Ankole, and Kampala) of 15 regions; increases occurred in Teso (p=0.049). Maternal deaths attributable to sepsis declined from 22% in 2018 to 8.6% in 2022 (p=0.005), and the average case-fatality was 1.8%.
Conclusion: There was a significant decline in maternal sepsis incidence and maternal deaths attributable to sepsis from 2018 to 2022, with the maternal deaths attributable to sepsis target nearly achieved in 2022. This reduction in maternal deaths attributable to sepsis was due to a decrease in maternal sepsis incidence, rather than case-fatality rates. A study to understand the high MS admission incidence in Acholi region may support interventions to continue to reduce MS in Uganda.
Background
Pregnant and postpartum women easily develop infections that rapidly progress to sepsis (1). Maternal sepsis is a pregnancy-related life threatening condition characterized by an organ dysfunction due to infection during pregnancy, childbirth, after delivery, or after an abortion (2). Maternal sepsis presents with the following signs and symptoms; higher or lower temperature, mental confusion, sleepiness, difficulty in rousing, severe pain, or discomfort(2).
While sepsis affects people of all ages, some groups are more likely to be affected. These include very young children, older adults, and those with a weakened immune system such as pregnant women, HIV patients, and malnourished individuals among others(3). Physiological, immunologic, and mechanical changes that occur in pregnancy make pregnant women more susceptible to infections than non-pregnant women and may obscure signs and symptoms of infection and sepsis, resulting in a delay in the recognition and treatment of sepsis(4). Sepsis is a medical emergency that requires urgent attention and rapid treatment for survival. Sepsis can be treated and, in many instances, lives are saved by using existing and proven protocols(5). Many individuals fully recover from sepsis, while others may have long-lasting effects, such as amputations or organ dysfunction, like kidney failure. When poorly managed or undetected, maternal infections can result in to sepsis, mortality, or disability for the mother, and an increased likelihood of early neonatal infection (4). Additionally, maternal infections can have serious impacts on the health of women and neonates including chronic pelvic inflammatory disease, ectopic pregnancy, and infertility (6). The risk of sepsis can be reduced by preventing or quickly identifying and managing infections. This includes practicing good hygiene, staying current with vaccinations, and seeking treatment when infections are suspected(7).
Globally, over a million neonatal deaths have been reported to be attributed to maternal sepsis annually(8). Even though effective prevention, early identification, and adequate management of maternal sepsis can contribute to reducing the burden of sepsis as an underlying and contributing cause of morbidity and mortality, maternal sepsis is the third leading cause of maternal deaths contributing to 10.7% of preventable maternal mortality cases in low-income countries(9). The United Nations (UN) report estimated 287,000 maternal deaths globally in 2020, with 70% of the maternal deaths occurring in sub-Saharan Africa(10). Uganda is one of the sub-Saharan countries with the highest maternal mortality ratio estimated at 336 per 100,000 live births(11). According to the annual maternal perinatal surveillance and response report of 2018/19, maternal sepsis is the second leading cause of maternal deaths in Uganda contributing to 13% of the deaths(5).
Uganda has implemented several interventions to avert maternal sepsis and deaths. One key such intervention is the Maternal and Perinatal Death Surveillance and Response (MPDSR), which is aimed at identifying, notifying, auditing, and learning from each maternal death to prevent future deaths. Other interventions implemented to combat maternal sepsis in Uganda include: improving Water, sanitation, and hygiene (WaSH) in health facilities, increasing antenatal care coverage, improving the proportion of births attended to by a skilled birth attendant, and training health workers in Basic Emergency Obstetric and Newborn care, as well as Comprehensive Emergency Obstetric Newborn care(12)(13)
Despite these interventions, the annual maternal sepsis admission in Uganda increased between 2013 and 2017 from 28/10000 live births to 50/10000 live births (14). There was little information on the current national level incidence of maternal sepsis in Uganda despite the fact that health facilities and districts generate and report data in the District Health Information System (DHIS2) every month. We assessed the trends and distribution of maternal sepsis incidence, maternal deaths attributable to sepsis, and maternal sepsis case-fatality rate, Uganda, 2018-2022, to inform programming.
Methods
Study design, setting, and data source
We conducted a descriptive analysis of pregnancy related maternal sepsis surveillance data generated from the entire country through the DHIS2. According to the Uganda Bureau of Statistics, 24.6% of the Ugandan 41,584,000 population were women of childbearing age(15). Maternal sepsis services are offered at the level of National Referral Hospitals, Regional Referral Hospitals, General Hospitals, Health Centre IVs, and Health Centre IIIs.(16)
Uganda is divided into 15 health regions, namely; Bugisu, Ankole, Kigezi, South Central, North Central, Tooro, Teso, West Nile, Bunyoro, Bukedi, Lango, Karamoja, Kampala, Busoga, and Acholi regions (17).
Study variables, data abstraction, and analysis
We abstracted data on sepsis-related to pregnancy (cases and deaths), maternal deaths, and deliveries in a health unit (live births) from the aggregate data of HMIS 108. We considered HMIS 108 (in-patient) data because the computation of maternal sepsis incidence would be more accurate since the denominator of live births was more readily available for health facility deliveries. We also obtained data on the national reporting rates on maternal sepsis for the years 2018 to 2022 from DHIS2 to determine the relationship between reporting rates and maternal sepsis incidence.
The data extracted from the DHIS2 was exported to Microsoft Excel and then into Stata 14.0 for analysis. To obtain maternal sepsis incidence, we used a proxy indicator of maternal sepsis admissions at the health units. We therefore, divided maternal sepsis cases by the total number of live births at the units and then multiplied by 10,000 per year from 2018 to 2022 at the district, regional, and national levels. The Maternal deaths attributable to sepsis was calculated by dividing the maternal sepsis deaths by total maternal deaths and multiplied by 100. We also calculated the maternal sepsis case fatality rate, by dividing maternal sepsis deaths by the total number of maternal sepsis cases and multiplied by 100. We demonstrated the regional and national trends for maternal sepsis incidence, maternal deaths attributable to sepsis, and case-fatality rate using line graphs. We performed the Mann-Kendall test to determine the existence of change in the trend of maternal sepsis incidence, maternal deaths attributable to sepsis, and case-fatality rate, and to evaluate the significance of linear trends. We also drew choropleths maps using QGIS 3.22.3 to show geographical distribution of maternal sepsis rates by district of Uganda.
Ethical considerations
We conducted a descriptive analysis study using aggregated maternal sepsis surveillance data from all the health facilities across the country that report through the District Health Information System version 2 (DHIS2). The Ugandan MoH authorized us to conduct the study. This activity was also reviewed by the US CDC and was conducted consistent with applicable federal law and CDC policy. § §See e.g., 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq. The office of the Center for Global Health, US Center for Disease Control and Prevention determined that this activity was not human subject research and with its primary intent being for public health practice or disease control.
Data collected did not contain any individual personal identifiers and information was stored in password-protected computers, which were inaccessible by anyone outside the investigation.
Results
Trend of maternal sepsis incidence at health facilities, Uganda, 2018-2022
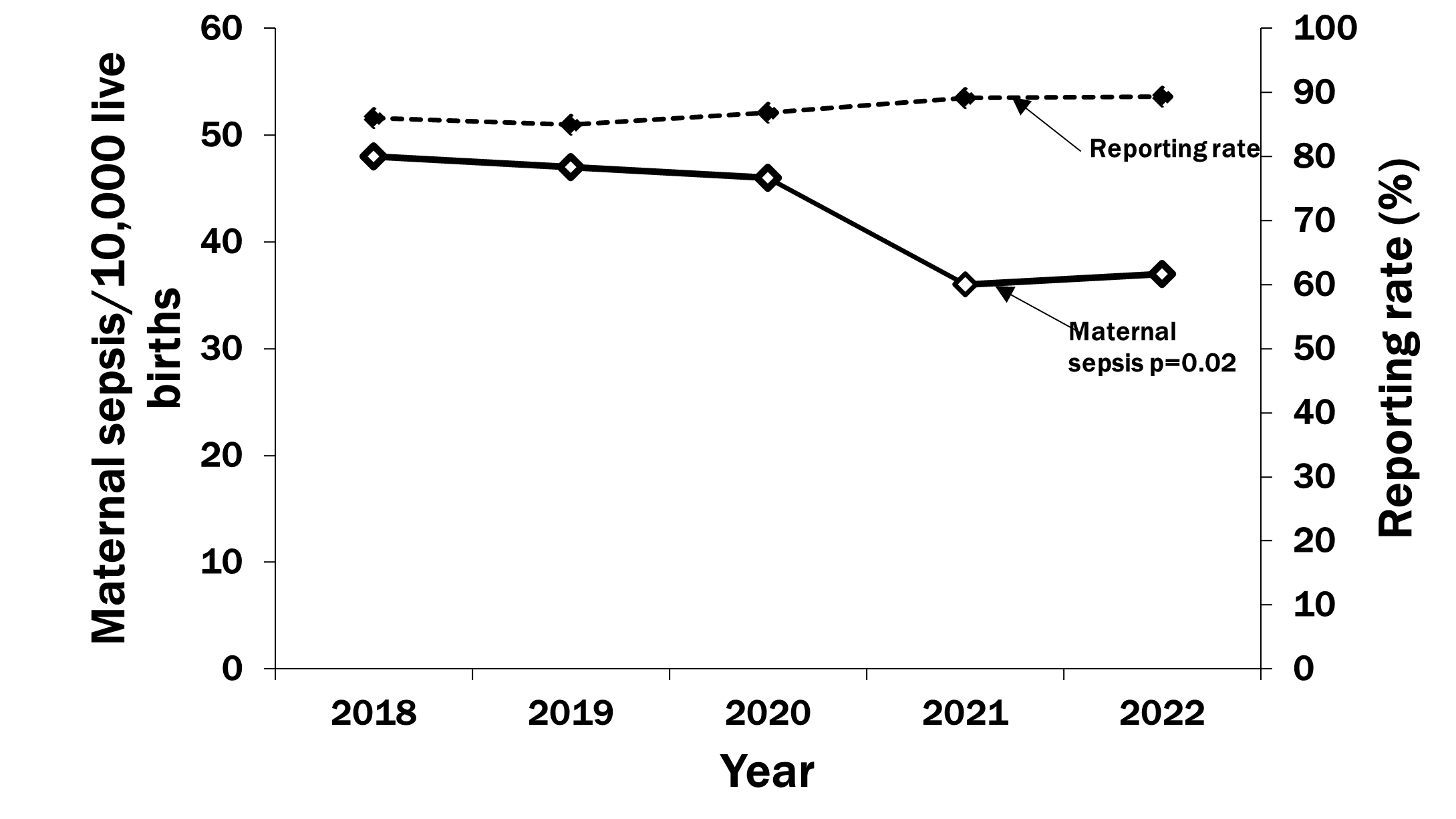
There were 24,285 new cases of maternal sepsis reported from 2018–2022. The maternal sepsis incidence rates in Uganda declined from 48 cases per 10,000 live births in 2018 to 37 cases per 10,000 live births in 2022 (p=0.02), with the highest decline reported between 2020 and 2021(Figure 1). The reporting rates were consistently high between 85 and 89% throughout the study period.
Distribution of maternal sepsis incidence at health facilities by region, Uganda, 2018-2022
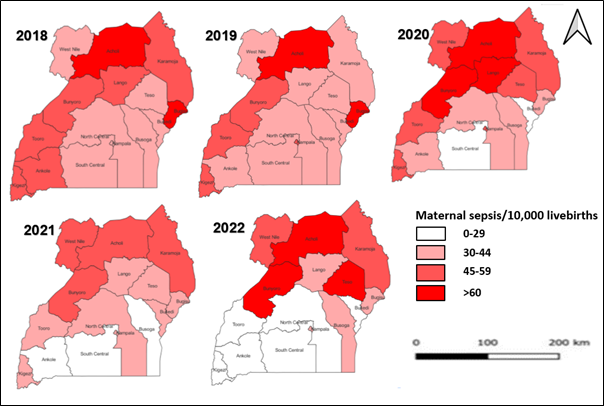
All the 15 regions in Uganda reported maternal sepsis cases and 6 of them showed a significant decrease in maternal sepsis incidence from January 2018 to December 2022. Teso Region, was the only region with a significant increase in maternal sepsis incidence from 39 maternal sepsis cases per 10,000 live births to 64 maternal sepsis cases per 10,000 live births (p=0.049) (Figure 2).
Distribution of maternal sepsis incidence at health facilities by districts, Uganda, 2018–2022
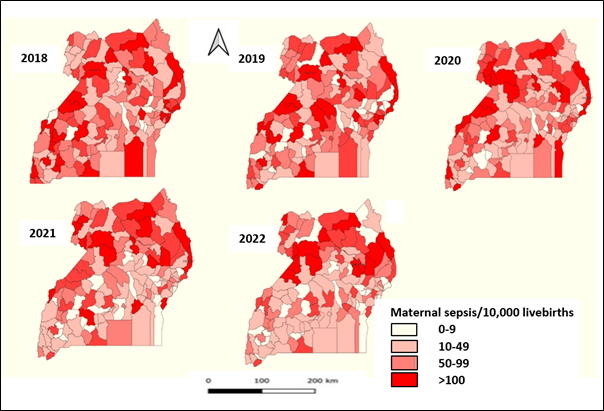
Nwoya District had the highest maternal sepsis incidence in both 2018 (139/10,000 live births) and 2019 (341/10,000 live births), Amudat District had the highest incidence in 2020 (244/10,000 live births) and 2021 (201/10,000 live births, and Amuria District had the highest incidence in 2022 (273/10,000 live births) (Figure 3). Nwoya District was the most affected throughout study with an average maternal sepsis incidence of 198/10,000 live births. This was followed by Moroto 136/10,000 live births, Amudat 125/10,000 live births, Kitgum 112/10,000 live births, and Hoima 95/10,000 live births.
Trend of maternal deaths attributable to sepsis in Uganda, 2018–2022
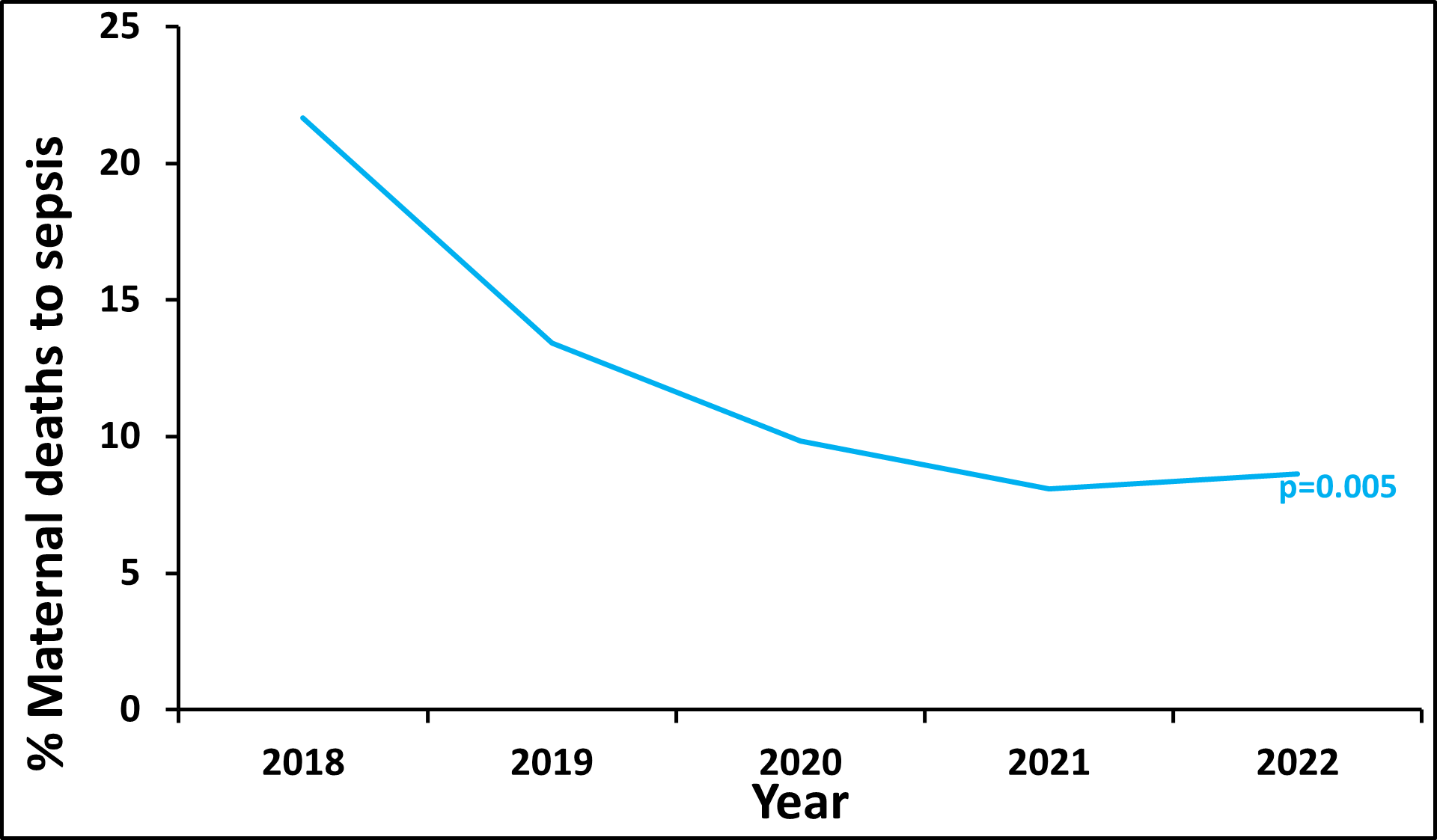
There were 479 maternal deaths due to maternal sepsis reported from 2018-2022. The proportion of maternal deaths that were due to sepsis was 21% in 2018. There was a decline in maternal deaths due to sepsis from 21 % in 2018 to 9 % in 2022 (Figure 4). Lango and Acholi regions had the highest average maternal deaths attributable to sepsis at 13 % through 2018-2022, while Bukedi was least affected at 3%.
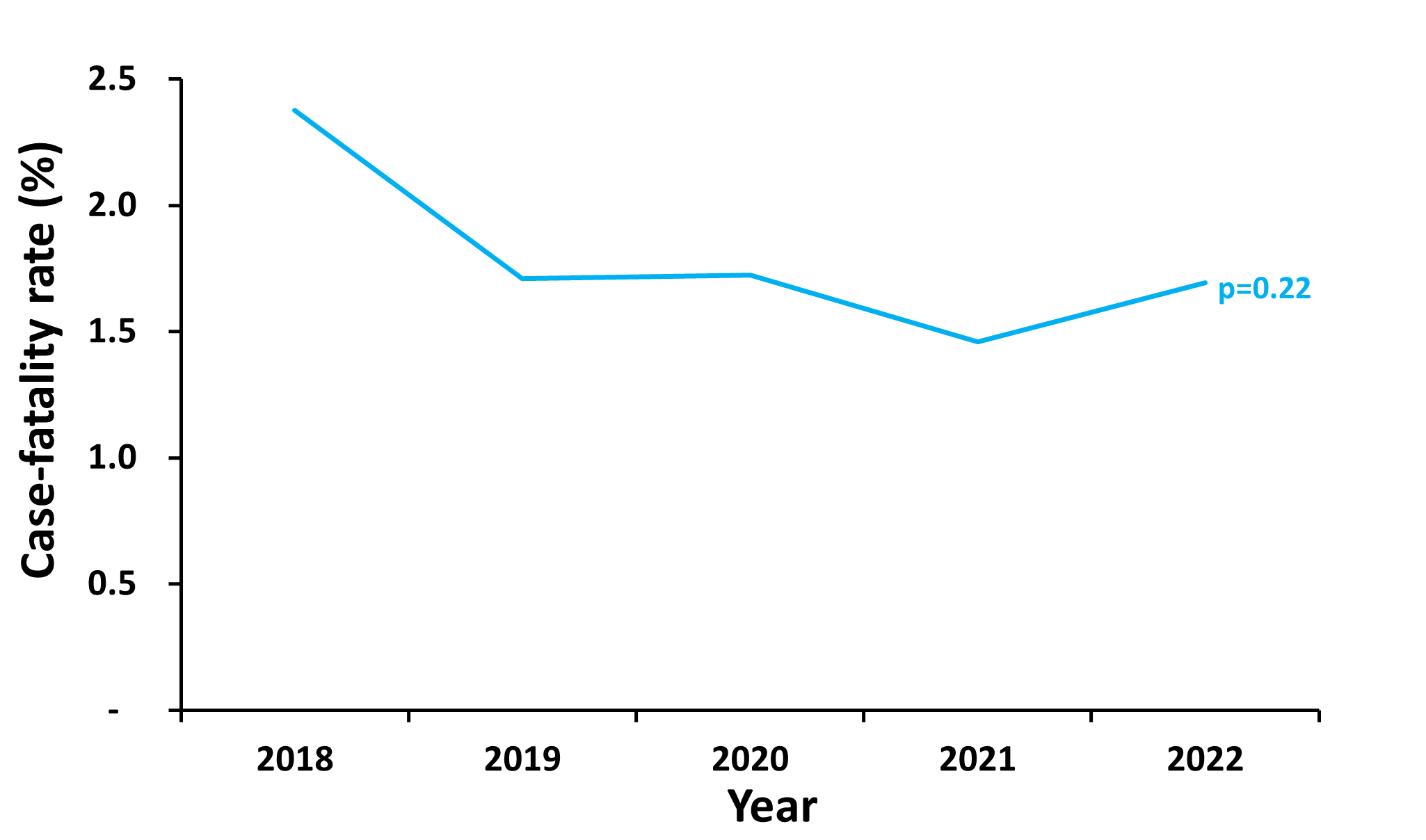
The trend of maternal sepsis case-fatality rate, Uganda, 2018–2022
There was no significant change in the maternal sepsis case-fatality rate (p=0.2207) through 2018-2022 (Figure 5). The maternal sepsis case fatality rate slightly changed from 2.4% in 2018 to 1.7% in 2022. The national average maternal sepsis case fatality rate was 1.8% from 2018-2022. Ankole (2.7%), North Central (2.5%), and Bugisu (2.3%) had the highest average maternal sepsis case fatality rates during the period of study, while Bukedi had the least CFR at 0.5%.
Discussion
We studied the trends and distribution of maternal sepsis in Uganda from 2018 to 2022. The maternal sepsis rates at health facilities in Uganda declined through the study period. The southern region of the country saw reductions in maternal sepsis rates, while the northern area of the country remained unchanged. Teso region was the only region with a significant increase in maternal sepsis rates. Maternal deaths attributable to sepsis declined and the case-fatality rate did not change.
The maternal sepsis incidence of 37 cases per 10,000 live births in 2022 in Uganda was low compared to a study conducted in Ethiopia on the incidence and predictors of puerperal sepsis among postpartum women that found maternal sepsis incidence at 70 cases per 10,000 live births(18). Another study conducted in 52 countries estimated sepsis to affect 109 cases per 10,000 live births. Women from low-income countries like Uganda had the highest sepsis rates at 151 cases per 10,000 live births (19). The decline in maternal sepsis incidence could be due to improved antenatal care coverage with up to 95% of pregnant women attending at least one antenatal care visit from skilled health personnel in the country as reported by the 2022 Uganda Demographic Health Survey (UDHS) (20). According to the WHO Global Maternal Sepsis Study on the aetiology and use of antibiotics in pregnancy-related infections, genital infections and urinary tract infections were the most frequent risk factors for maternal sepsis and these can be identified and managed during quality antenatal care (5).
The increased proportion of pregnant women giving birth in health facilities under the care of skilled birth providers could further explain the decline in the maternal sepsis incidence in the country since most of the risk factors related to developing maternal sepsis are assessed, identified and managed during skilled birth attendance (21). The decline in maternal sepsis incidence is a significant progress towards improving maternal and child health services and a key step to the achievement of both target 3.1 (maternal mortality reduction) and target 3.2 (neonatal mortality reduction) of the Sustainable Development Goals(22).
Maternal sepsis incidence was high in the northern area of the country. The findings were in agreement with the findings of a study that was conducted to assess the trend and distribution of puerperal sepsis in Uganda that indicated northern region was one of the most affected regions with sepsis contributing up to 24% of the maternal deaths (23). The high maternal sepsis incidence in northern region could be due to the low coverage of skilled birth attendance of 50% (15).The low skilled birth attendance is likely associated with mothers seeking for care at later stages with complications that could predispose them to sepsis (24). According to Urendi (2023) in a study on traditional birth attendants and associated factors among pregnant mothers in selected communities in northern Uganda, traditional birth attendance was reported at 58%(25). The low skilled birth attendance could be due to this high traditional birth attendance in the region with participants citing long distances to health facilities, family influence, and low socioeconomic status as significant factors associated with traditional birth attendance.
The decline in maternal deaths attributable to sepsis was consistent with the results of the systematic review of studies on causes of maternal mortality in Sub-Saharan Africa that revealed maternal sepsis contributed 11% of the maternal deaths (26). However, the maternal sepsis contribution of 8.6% to maternal deaths was low compared to the 16.5% of a study done in 2020 at a regional referral hospital in south western Uganda, that focussed on the factors associated with severe maternal outcomes (27). This is probably due to the regional variations observed in this study as the southern region saw reductions in maternal sepsis rates, the northern area remained unchanged, and Teso region a significant increase in maternal sepsis incidence. Given that Teso region had a good skilled birth attendance at 74%, the increase in maternal sepsis could have been due to poor infection, prevention and control measures at health facilities(11). Maternal sepsis is the second largest cause of preventable maternal deaths in Uganda (8),thus the decline in maternal sepsis incidence significantly reduces maternal mortality. This was evidenced by the coincidental reduction of the maternal mortality ratio in Uganda from 336/100,000 live births in 2016 to 189/100,000 live births in 2022 (20).
Study limitations
This analysis was based on the quality of data reported by the health facilities into the DHIS 2, the cases reported in DHIS2 only include those that have reached health facilities, leading to an underestimation of the overall burden of maternal sepsis due to healthcare access bias. In addition, the average reporting rate through the period of study was 87%. This likely led to underestimates of total cases in the study period; however, since we were comparing rates, it may or may not have affected the interpretation of results. We also verified the accuracy of the reported data by reviewing the regular data quality assessment reports(28). Furthermore, maternal sepsis diagnosis in resource-limited settings like Uganda does not have to be laboratory-confirmed. This may have led to over diagnosis.
Conclusion
Uganda registered a significant decline in maternal sepsis incidence and maternal deaths attributable to sepsis from 2018–2022, with the target of <8% of maternal deaths due to sepsis by 2024; nearly achieved in 2022. The decline in maternal deaths attributable to sepsis was due to a reduction of Maternal Sepsis incidence, but not case-fatality rates. We recommended that the Ministry of Health and its partners focus on intensified infection prevention and control practices at health facilities, and sensitization of health care providers and mothers on the presentation, cause, prevention, and management of maternal sepsis as this may further reduce both the incidence and case-fatality rates.
A study to understand the high Maternal Sepsis incidence in the northern area may support interventions to continue to reduce Maternal Sepsis in Uganda.
Conflict of interests
The authors declare that they have no competing interests.
Author’s contribution
LT, RM, and RM participated in the conception, design, analysis, interpretation of the study, and wrote the bulletin; BK, RM, DK, RM, RM, IN, and ARA reviewed the drafts of the bulletin for intellectual content and made multiple edits to the draft bulletin. All authors contributed to the final draft of the bulletin. All the authors read and approved the final bulletin.
Acknowledgments
We thank the staff of the Public Health Fellowship Program for the technical support and guidance offered during this study. We thank the Ministry of Health Reproductive Health Division for granting permission and overall guidance to the team.
Copy right and licensing
All materials in the Uganda Public Health Bulletin are in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med. 2014;370(23):2211–8.
- Escobar MF, Echavarría MP, Zambrano MA, Ramos I, Kusanovic JP. Maternal sepsis. Am J Obstet Gynecol MFM. 2020;2(3):100149.
- van Dillen J, Zwart J, Schutte J, van Roosmalen J. Maternal sepsis: epidemiology, etiology and outcome. Curr Opin Infect Dis. 2010;23(3):249–54.
- Greer O, Shah NM, Sriskandan S, Johnson MR. Sepsis: precision-based medicine for pregnancy and the puerperium. Int J Mol Sci. 2019;20(21):5388.
- Ribeiro-do-Valle CC, Bonet M, Brizuela V, Abalos E, Baguiya A, Bellissimo-Rodrigues F, et al. Aetiology and use of antibiotics in pregnancy-related infections: results of the WHO Global Maternal Sepsis Study (GLOSS), 1-week inception cohort. Ann Clin Microbiol Antimicrob. 2024;23(1):1–12.
- Hussein J, Walker L. Puerperal sepsis in low and middle income settings: past, present and future. Matern infant deaths Chas Millenn Dev goals. 2010;4:131–47.
- WHO. Improving the prevention, diagnosis and clinical management of sepsis- Report by the Secretariat. WHO Publ [Internet]. 2017;executive(January):1–6. Available from: https://apps.who.int/iris/bitstream/handle/10665/273181/B140_12-en.pdf?sequence=1&isAllowed=y
- Black RE, Levin C, Walker N, Chou D, Liu L, Temmerman M. Reproductive, maternal, newborn, and child health: key messages from disease control priorities 3rd edition. Lancet. 2016;388(10061):2811–24.
- Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Heal. 2014;2(6):e323–33.
- Zarocostas J. Global maternal mortality rates stagnating. Lancet. 2023;401(10377):632.
- UBOS and Rockville, Kampala, Uganda and Maryland U. Uganda Demographic and Health Survey 2016: Key Indicators Report, Maternal mortality. Uganda Bureau of Statistcs (Ubos). 2017.
- UBOS. the Republic of Uganda Uganda Demographic and Health Survey (Udhs) 2022 Key Findings. Work Dissem Dist Kampala [Internet]. 2023;(September). Available from: www.ubos.org
- MOH. NEWBORN AND CHILD HEALTH SHARPENED PLAN FOR UGANDA November 2013. 2013;(November). Available from: http://www.usaid.gov/sites/default/files/documents/1860/Reproductive_Maternal_Newborn_and_Child_Health_Sharpened_Plan_for_Uganda-Final_Version_Nov2013.pdf
- KAMPALA IIN. MINISTRY OF HEALTH UGANDA. 2018;
- UBOS. Uganda Demographic and Health Survey 2016. Kampala; 2018.
- Health M of. National Health Facility Master List 2018. A Complet List all Heal Facil Uganda. 2018;
- MOH. National Health Data Repository [Internet]. DHIS II. 2023. Available from: https://hmis-repo.health.go.ug/repo/dhis-web-dashboard/#/
- Bishaw KA, Sharew Y, Beka E, Aynalem BY, Zeleke LB, Desta M, et al. Incidence and predictors of puerperal sepsis among postpartum women at Debre Markos comprehensive specialized hospital, northwest Ethiopia: A prospective cohort study. Front Glob Women’s Heal. 2023;4:966942.
- Bonet M, Brizuela V, Abalos E, Cuesta C, Baguiya A, Chamillard M, et al. Frequency and management of maternal infection in health facilities in 52 countries (GLOSS): a 1-week inception cohort study. Lancet Glob Heal. 2020;8(5):e661–71.
- UDHS. Uganda Demographic and Health Survey ( UDHS ) 2022 Extension. Key Findings. Sherat Hotel Kampala Dist 8th Sept 2023. 2023;(September).
- Plante LA, Pacheco LD, Louis JM, (SMFM S for M-FM. SMFM Consult Series# 47: Sepsis during pregnancy and the puerperium. Am J Obstet Gynecol. 2019;220(4):B2–10.
- Hudson I, PM G. The Impact of Birth Preparedness on Pregnancy Outcome: Findings from Lurambi Sub County, Kakamega County, Kenya. J Pregnancy Child Heal. 2016;3(4).
- Alobo G, Reverzani C, Sarno L, Giordani B, Greco L. Estimating the Risk of Maternal Death at Admission: A Predictive Model from a 5-Year Case Reference Study in Northern Uganda. Appiah-Denkyira E, editor. Obstet Gynecol Int [Internet]. 2022;2022:4419722. Available from: https://doi.org/10.1155/2022/4419722
- Brizuela V, Cuesta C, Bartolelli G, Abdosh AA, Abou Malham S, Assarag B, et al. Availability of facility resources and services and infection-related maternal outcomes in the WHO Global Maternal Sepsis Study: a cross-sectional study. Lancet Glob Heal. 2021;9(9):e1252–61.
- Urendi. Traditional Birth attendants and Associated Factors among Pregnant Mothers in Selected Communities of Arua District in Northern Uganda : A Case Study of NEWPORT INTERNATIONAL JOURNAL OF PUBLIC HEALTH AND PHARMACY ( NIJPP ) Traditional Birth attendants and. Tradit Birth Attend Assoc Factors among Pregnant Mothers Sel Communities Arua Dist North Uganda. 2023;(October).
- Musarandega R, Nyakura M, Machekano R, Pattinson R, Munjanja SP. Causes of maternal mortality in Sub-Saharan Africa: a systematic review of studies published from 2015 to 2020. J Glob Health. 2021;11.
- Dale M, Kajabwangu R, Mayengo H, Munyanderu B, Baluku A, Manyang A, et al. Factors Associated With Severe Maternal Outcomes at a Regional Referral Hospital in South-Western Uganda: A Case-Control Study. 2020;
- Agiraembabazi G, Ogwal J, Tashobya C, Kananura RM, Boerma T, Waiswa P. Can routine health facility data be used to monitor subnational coverage of maternal, newborn and child health services in Uganda? BMC Health Serv Res. 2021;21:1–10.


Comments are closed.