Contact Tracing and Community-Based Surveillance for COVID-19 Using Health Assistants, Masindi District, Uganda
Quarterly Epidemiological Bulletin: October– December, 2020: Volume 5 / Issue 4/Article No. 1 Authors: Bob O. Amodan*, 1, Immaculate Akusekera1, Geoffrey Amanya1, Josephine Namayanja1, Daniel Kadobera1, Alfred Driwale2, Alex R. Ario1, 2, Julie Harris3
Summary
On 1st May 2020, the first case of COVID-19 in Masindi District, Uganda, was identified. The case-patient, a policeman, who had more than 750 contacts. Previously, central-level healthcare workers from the Ministry of Health had been deployed to conduct contact tracing in districts, which was highly resource-intensive. We set out to build capacity of health Assistants in Masindi to strengthen district COVID-19 surveillance response capacity, and compared costs of deploying central-level vs local-level responders using this case as a model.
We spent May 2-16, 2020 in Masindi District, working with the District Task Force to identify 31 environmental health workers (Health Assistants [HAs]) and train them for 2 days in COVID-19 contact tracing and community-based surveillance (CBS). We tracked the proportion of all contacts followed up by HAs each day and supported HAs to establish a CBS system comprising community leaders and village health teams. We calculated and compared response costs between use of 31 HAs and 10 central-level epidemiologists for this work.
HAs identified 729 contacts, and visited or telephoned 20-25 contacts daily for 14 days after their last exposure to the case-patient. Of the 729 contacts, 725 (99.5%) were followed for 14 days and four were lost to follow-up. All contacts tested negative for SARS-CoV-2 at Day 14. From 5-16 May, the new CBS system received and investigated 531 separate community alerts for suspected cases unlinked to the index case.
Using HAs vs central-level epidemiologists reduced the 14-day response costs by 70% ($8,300 to $2,500). District-level training in COVID-19 contact tracing and CBS from the central level enabled a less costly and a more effective approach to alert response and contact tracing at the local level. Decentralized use of the HAs to conduct contact tracing and CBS can increase community and District ownership of COVID-19 response.
Introduction
On 1 May 2020, the first community transmission case of COVID-19 was identified in Masindi District, western Uganda during a rapid assessment survey among high-risk persons on the prevalence of the COVID-19 in communities. The case-patient was a 29-year-old, police officer who worked at homicide department of Masindi District as a criminal investigator. This case-patient was the first known case that had no travel history and link to truck drivers, who had contributed to bulk of confirmed cases in Uganda at the time.
On 2 May 2020, the Public Health Emergency Operations Centre, Ministry of Health notified the Incident Management Team, and a team of four field epidemiology fellows from the Uganda Public Health Fellowship Program were sent to Masindi District to establish an epidemiologic linkage, and support the district in response.
At that time, Masindi District lacked the capacity to do an effective COVID-19 response. This included contact tracing, which involves contact identification and listing, and then follow-up to detect any contacts who become ill. This critical component of the COVID-19 response is facilitated by local structures and knowledge that the central level team might have a difficult time providing. In addition, Masindi did not have a community-based surveillance structure. This was critical for ensuring the presence of an alerts system, which can detect any suspected cases through reporting.
Contact tracing is the identification, listing, and follow-up of all exposed persons to determine whether they could have contracted the disease from their contact with the infected person. It is also one of the single most important activity that breaks the chain of transmission of COVID-19 [5]. As opposed to active surveillance, use of community-based surveillance systems to control spread of COVID-19, is an attractive alternative design and operation is recommended. Effective community-based contact tracing surveillance program requires constant community engagement
[6] and use of Health Assistants. We supported the district contain the spread of the virus by building capacity of Health Assistants to strengthen surveillance, and compared costs of deploying central-level vs local-level responders (Health Assistants) using this case as a model.
Methods
Identification and training of Health Assistants
We worked with the COVID-19 District task force on 2 May, 2020 to identify 31 Health Assistants who were trained from 3- 4 May 2020 on how to conduct contact tracing using WHO guidelines [6]. All contacts were listed from 20 April to 2 May, 2020 when the case was isolated for management. The start contact date of 20 April 2020 was chosen because the case-patient had reported history of cough and flu-like symptoms from 22 to 25 April, 2020.
We further trained the Health Assistants on community-based surveillance. In so doing, key issues such as: benefits of a functional community-based surveillance system, community case definition for COVID-19, and how-to set-up and manage community COVID-19 alerts was shared with Health Assistants.
Contact identification and Listing during COVID-19 outbreak, Masindi District, Uganda, May 2020
On 2nd May, 2020, we conducted a telephone interview with the case-patient to understand the list of people who had contact with him during the specific timeframe mentioned above.
Furthermore, we interviewed the officer in-charge of the local police station to further understand the duties the case-patient was doing, and authorize release of the police documents for our perusal. We reviewed police records to identify the people who had interacted with the case-patient during execution of his duties.
With support from the district health office, the Health Assistants called upon all contacts of the case-patient through radio talk shows and announcements to volunteer themselves to the health authorities regardless of any punitive, security, and immigration issues they were facing.
In addition, Health Assistants made phone calls to the identified contacts and further conducted home visits to collect contact details and linked them to the quarantine management team.
Contacts were given phone calls (if having phones) and visited by the Health Assistants in the afternoons after the training to ascertain the level of contact with the confirmed case-patient. During listing, demographic, residence, exposure history, clinical and relationship with the case information was collected. Health Assistants also counselled contacts, and emphasized on precautions and rationale for contact tracing. A total of 729 contacts were listed; of which, 323 were listed on 2 May, 2020 and later geographically quarantined. On 3 May, 2020, another 125 contacts were listed and later taken to institutional quarantine centers for monitoring. The other, 281 contacts were listed on 4 May, 2020 and asked to stay at home on self-quarantine.
Confidentiality of the contacts’ information was maintained and well managed by the Health Assistants. Efforts were made to have the contacts’ lives protected, and stigma arising from community members was also confronted using risk communication messages aired by Health Assistants or Health educators on radios.
Follow-up of contacts during COVID-19 outbreak in Masindi District, Uganda, May 2020
The Health Assistants opted to follow-up all the contacts for 14 days from the date the case was taken for isolation (2 May, 2020). This was so, first, because most of the contacts could not remember their exact dates of last contact with the index case-patient. Secondly, because majority of the contacts had closely mixed with each other at quarantine centers and police stations.
Each Health Assistant was assigned 20 to 25 contacts to follow-up on daily basis using the Ministry of Health’s COVID-19 follow-up form. The team either home visited or telephoned the contacts to understand whether they had developed signs and symptoms in each of the 14 days of observation. Only 11 Health Assistants were given infra-red thermo scans for taking temperature readings, and other 20 took self-reported fever since the thermometers were not enough.
Health Assistants reported to the District Surveillance Focal person on daily basis, specifically highlighting number of contacts followed-up, lost to follow-up, and those who developed signs and symptoms related to COVID-19. Contacts who developed COVID-19 related signs and symptoms were isolated and immediately tested for COVID-19.
We entered data in excel spreadsheets, analyzed on daily basis into descriptive statistics, and shared with the COVID-19 District rapid response team and District task force for decision making.
Activating community-based surveillance during COVID-19 outbreak, Masindi District, Uganda, May 2020
Health Assistants set-up a functional community-based surveillance system from 5 to 16 May 2020. They reached out to the village health teams and local council one leaders to educate them
on the urgent need to control COVID-19 by opening channels for reporting of any suspected cases to the district health authorities.
Additionally, Health Assistants also shared COVID-19 community case definition with the local leaders so that they knew what to look for, and left their phone numbers with them for reporting of any persons who met the community case definition.
Costing the response during COVID-19 outbreak, Masindi District, Uganda, May 2020
We also roughly calculated the costs of all the activities we carried out using the Health Assistants, and compared them to what the costs would have been if we had only used central- level health workers. These costs included Safari day allowances for HAs or per diem for central level health workers and fuel.
Results
Contacts traced during COVID-19 outbreak, Masindi District, Uganda, May 2020
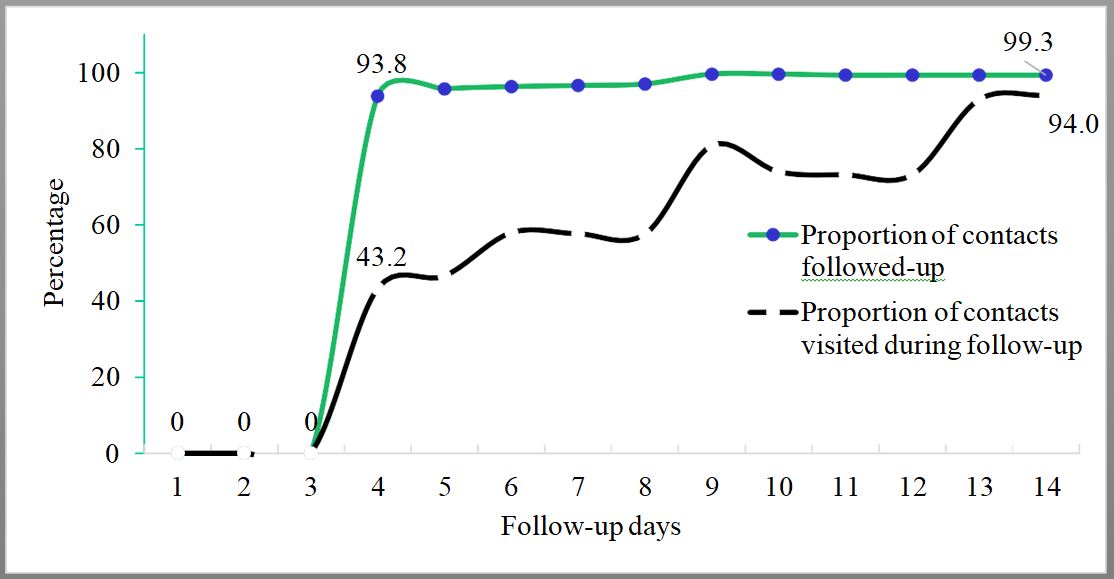
A total of 729 contacts were listed and followed-up for 14 days. The first 3 days in figure 1 showed zero performance in terms of follow-up. The proportions of contacts followed-up by either home visit or phone call increased from day 4 at 94% to day 14 at almost 100%. The proportion of contacts followed-up by only home visit also gradually increased from 43% to 94% (Figure 1).
In addition, during 14-days follow-up, no contact turned positive for COVID-19 even when 3.8% (28/729) contacts developed signs and symptoms related to COVID-19. Only 0.55% (4/729) contacts were lost to follow-up in between day 9 and 13.
Activating community-based surveillance during COVID-19 outbreak in Masindi District, Uganda in May 2020
Health Assistants also managed to set up a functional community-based surveillance system. As compared to before, when there were no formal COVID-19 alert management and linkage systems, 531 non-index case-linked community alerts were collected and investigated in between 5-16 May, 2020.
Response costs that were incurred during COVID-19 outbreak in Masindi District, Uganda in May 2020
The cost doing contact tracing and community-based surveillance when central-level team is used would be over $8,300 and that of Health Assistants would be 2,500 US dollars (Table 2).
The difference between separate costs of central-level team and Health Assistants response would be over USD 5,800, which is a 70% reduction of costs if we used only health assistants.
Table 1: COVID-19 Response costs of using central-level versus Health Assistants during COVID-19 outbreak, Masindi, Uganda, May 2020
| Item | Qty | Unit cost | Freq | Total Cost (UgX) | Total Cost (USD)** |
| Allowance (per | 5 | 160,000 | 15 | 12,000,000 | 3,158 |
| Fuel | 2 | 60,000 | 15 | 1,800,000 | 474 |
| Driver allowance | 2 | 160,000 | 15 | 4,800,000 | 1,263 |
| Allowance (per | 5 | 150,000 | 15 | 11,250,000 | 2,961 |
| Driver allowance | 1 | 75,000 | 15 | 1,125,000 | 296 |
| Fuel | 1 | 60,000 | 15 | 900,000 | 237 |
| Subtotal -1 | 31,875,000 | 8,388 | |||
| Use of Health assistants (costing) | |||||
| Allowance (SDA) | 31 | 12,000 | 14 | 5,208,000 | 1,371 |
| Fuel | 31 | 10,000 | 14 | 4,340,000 | 1,142 |
| Subtotal-2 | 9,548,000 | 2,513 | |||
** USD 1.0 = 3,800 UgX
Discussion
This activity built the capacity of Health Assistants in contact tracing and community-based surveillance. In addition, costs of deploying central-level vs local-level responders (HAs) using this case as a model were estimated. The Health Assistants have a broad spectrum and all- encompassing range of skills that makes them unique and easily understand a lot of disciplines within prevention and control of outbreaks [7]. The capacity of Health Assistants was greatly built with less costs, and turned to be a more effective approach for implementing contact tracing and community-based surveillance.
This case-patient generated the highest number of documented contacts in Uganda. This could be partly due to the nature, high mobility and busy schedule of the case-patient. High mobility patterns or habits have been linked to high COVID-19 transmission [8, 9].
The contacts were not followed-up as expected in the first three days because the Health Assistants were being mobilized and trained on the essentials of contact tracing and community- based surveillance. In the subsequent days (from day 4 to 14 of follow-up), the Health Assistants were deployed under our supervision. Overall follow-up by either home visit or phone call was well done as exhibited by the high daily proportion of contacts followed-up from the first to the last day. This could be because Health Assistants were familiar, well known, and respected health workers, and thus did not have to grapple with local mis-trust, language barrier, terrain, and culture of Masindi District. Whereas daily contact follow-up was not 100% as expected [6, 10], this achievement was way too high when we consider Uganda’s possible past challenges in contact follow-up such as, non-cooperation of contacts, poor geographical and settlement patterns.
To note, there was progress in terms of proportion of contacts home visited during follow-up even when the team did not make it to the recommended 100% coverage on each day. This was attributed to wide dispersion between homes of self-quarantined contacts in the rural areas, and that there was inability to trace contacts in the urban areas in the maiden days of follow-up. In addition, inaccurate and miss leading residence data was collected by the local untrained health workers who had partly done contact listing.
Even when the institutional quarantine centre had registered a run way, a loss to follow-up of any contact was not constituted because, by the help of the police, community members and media houses, the escapee was apprehended and returned to the centre within 1 day. This escape happened because; first, the parameter wall was too low, so one could easily jump over, and secondly, the security personnel were not many enough. Later, the security at the quarantine centre was beefed up by the army as recommended by the country’s quarantine guidelines [11], and that explained why we did not have any other escapees during the follow-up days. At self- quarantine homes, there was a loss to follow-up that could be attributed to indiscipline (not to staying home) among contacts or feeling of stigma because of health-worker home visit follow- up. In addition, some of the contacts were bodaboda motorcycle riders who wanted to fend for themselves and families. Even when efforts were made to involve the local leadership to make sure that all contacts adhered to the self-quarantine regulations, those lost to follow-up went to stay somewhere else unknown until the 14 days follow-up was over. Escapes and loss to follow-up could cause spread of COVID-19 among other groups of people. Use of digitalized contact tracing could reduce possible stigma due to face-to-face contact interactions with the contact tracing team [12].
No single contact, even those who developed signs and symptoms related to COVD-19 turned positive. This could partly be because the case was not exposed to the contacts during his most infectious stage of the infection since he developed COVID-19 related signs and symptoms after he was isolated. The risk of transmission of COVID-19 is higher when the case is symptomatic [13, 14].
Community-based surveillance systems were established and kept functional during the response to the outbreak. This is partly due to the fact that Health Assistants have a sound technical training, respect from the local leaders, since they often work together in many other health programs at community level.
Conclusion and Recommendations
In conclusion, building capacity of Health Assistants enabled proper contact listing and follow- up. Use of Health Assistants to conduct contact tracing and Community based surveillance activities can increase community and district ownership of COVID-19 response. In addition, Use of HAs was a less costly and a more effective approach to alert management and contact- tracing.
Since the outbreak was likely to take long or even have other waves, we recommended that the Ministry of Health, Uganda adopts using Health Assistants to accomplish the demands of COVID-19 contact tracing and community-based surveillance. In adopting the use of health assistants, there need to: Build their capacity, support digital innovations of contact tracing, fund the tasks and monitor performance.
References
- Naming the coronavirus disease (COVID-19) and the virus that causes it [https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical- guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it]
- MoH: Uganda confirms 1st case of COVID-19. Saturday 21 March 2020. In.: Ministry of Health, Uganda;
- Liu J, Liao, X., Qian, S., Yuan, J., Wang, F., Liu, Y., … Zhang, Z.: Community transmission of severe acute respiratory syndrome coronavirus 2. Emergency Infectious Diseases 2020, 26(6).
- Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, Marimuthu K: Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA 2020, 323(16):1610-1612.
- World Health Organization: Critical preparedness, readiness and response actions for COVID- 19: interim guidance, 22 March 2020. In. Geneva: World Health Organization;
- World Health Organization: Contact tracing in the context of COVID-19: interim guidance, 10 May 2020. In.;
- Morse T, Chidziwisano K, Musoke D, Beattie TK, Mudaly S: Environmental health practitioners: a key cadre in the control of COVID-19 in sub-Saharan Africa. BMJ Global Health 2020, 5(7):e003314.
- Badr H, Du H, Marshall M, Dong E, Squire M, Gardner L: Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. The Lancet Infectious Diseases
- Cartenì A, Di Francesco L, Martino M: How mobility habits influenced the spread of the COVID- 19 pandemic: Results from the Italian case study. Science of The Total Environment 2020, 741:140489.
- Africa Centres for Disease Control and Prevention: Guidance on Contact Tracing for COVID-19 Pandemic. In.;
- Ministry of Health: Guidelines on Quarantine of Individuals in the Context of Containment of Coronavirus Disease (COVID-19) in Uganda. In. Kampala;
- Owusu PN: Digital technology applications for contact tracing: the new promise for COVID-19 and beyond? Global Health Research and Policy 2020, 5(1):36.
- Cheng H-Y, Jian S-W, Liu D-P, Ng T-C, Huang W-T, Lin H-H, Team ftTC-OI: Contact Tracing Assessment of COVID-19 Transmission Dynamics in Taiwan and Risk at Different Exposure Periods Before and After Symptom Onset. JAMA Internal Medicine 2020, 180(9):1156-1163.
- Lipsitch M, Cohen T, Cooper B, Robins JM, Ma S, James L, Gopalakrishna G, Chew SK, Tan CC, Samore MH et al: Transmission Dynamics and Control of Severe Acute Respiratory Syndrome. Science 2003, 300(5627):1966.
Reference this page as below
Bob O. Amodan*, 1, Immaculate Akusekera1, Geoffrey Amanya1, Josephine Namayanja1, Daniel Kadobera1, Alfred Driwale2, Alex R. Ario1, 2, Julie Harris3, Contact Tracing and Community-Based Surveillance for COVID-19 Using Health Assistants in Masindi District. Kampala, Uganda National Institute of Public Health. 2020 Deecember 26th. Available from:https://uniph.go.ug/wp-content/uploads/2021/05/1-Vol-1-Issue-4-Article-No-1-LB18Jan2021-Contact-Tracing-and-Community-Based-Surveillance-for-COVID-19-Using-Health-Assistants-Masindi-District.pdf


Comments are closed.