Trends and Distribution of Severe Malaria Cases, Uganda, 2017–2021: Analysis of Health Management Information System Data
Authors: Marie Gorreti Zalwango1, Lilian Bulage1, Jane F. Zalwango1, Richard Migisha1, Bosco B. Agaba2, Daniel Kadobera1, Benon Kwesiga1, Jimmy Opigo2, Alex Riolexus Ario1 Institutional affiliations: 1Uganda Public Health Fellowship Program-Uganda National Institute of Public Health, Kampala, Uganda, 2National Malaria Control Division, Ministry of Health, Kampala, Uganda. *Correspondence: Email: mzalwango@musph.ac.ug, Tel: +256752610802
Summary
Background: Malaria remains the largest contributor to morbidity and mortality among children <5 years in Uganda. We evaluated the trends and distribution of severe malaria from 2017–2021 to inform progress on current interventions to reduce malaria morbidity and mortality in the country.
Methods: We used secondary data from monthly malaria surveillance reports from the District Health Information System (DHIS2) for 2017–2021. As per DHIS2, severe malaria was defined as any admission with confirmed malaria (by microscopy or rapid diagnostic test (RDT)). We calculated proportions of malaria cases that progressed to severe malaria for each year using severe malaria cases as the numerator and total outpatient malaria cases as the denominator. We used logistic regression to evaluate trends by administrative levels and by health facility type.
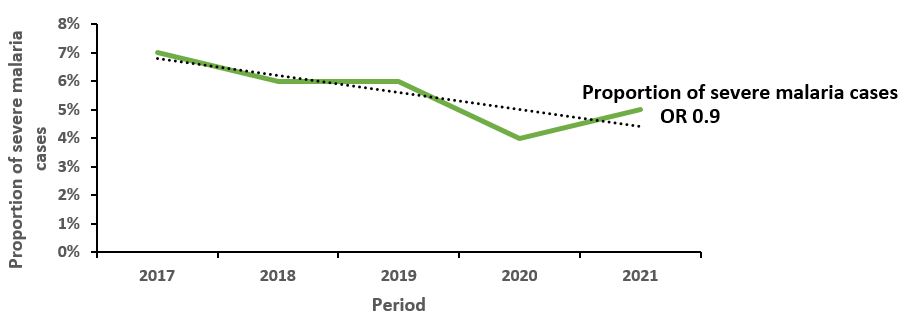
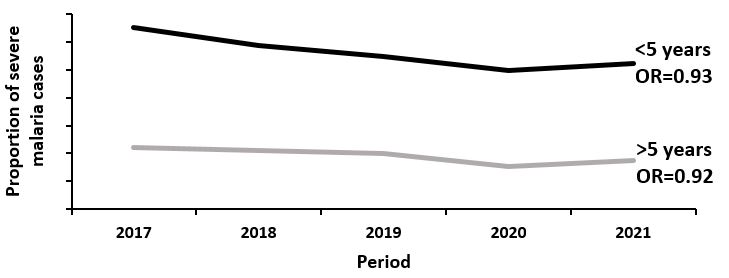
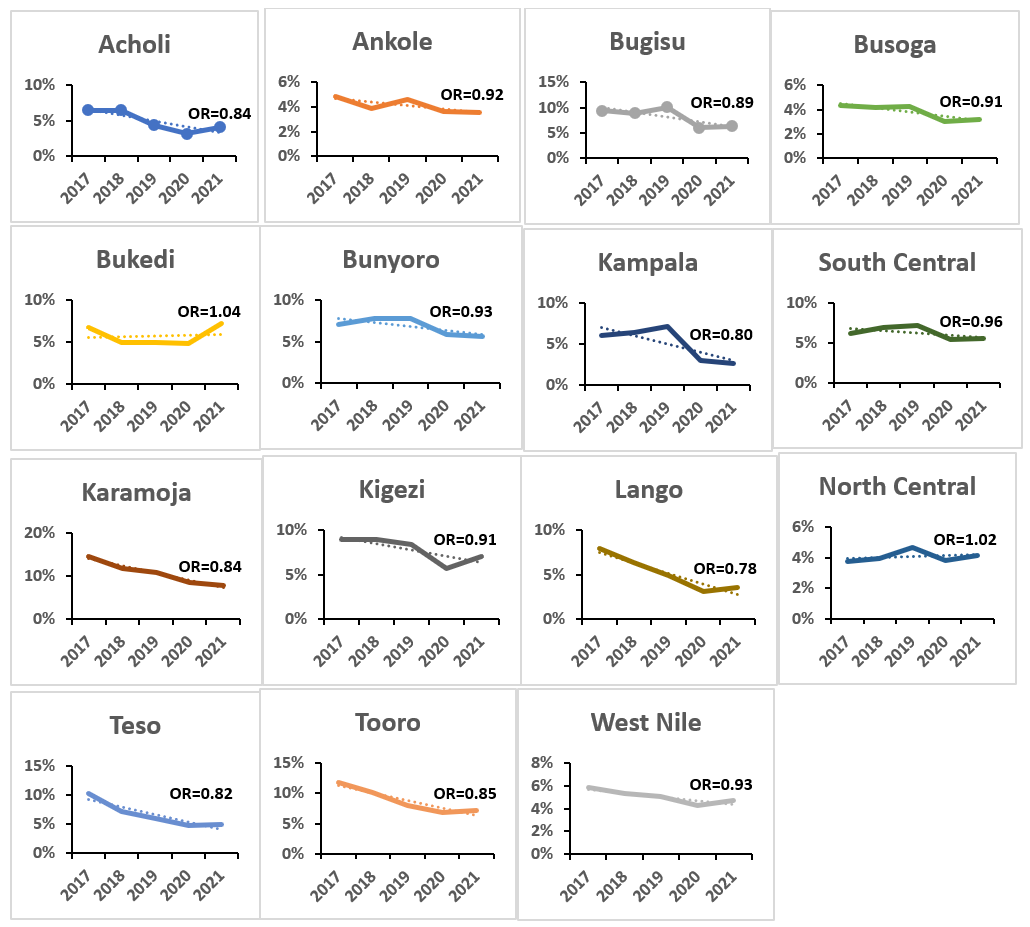
Results: Overall, 2,957,672 severe malaria cases were reported. Severe malaria cases as a proportion of all malaria cases decreased by 10% annually from 7.0% (679,328/ 10,263,374) in 2017 to 5.0% (539,995/ 11,029,320) in 2021 (OR=0.90; p<0.001). The proportion among children <5 years reduced from 13% in 2017 to 10% in 2021 while that for >5 years reduced from 4.4% to 3.5%. The proportion among females reduced from 6.1% in 2017 to 4.6% in 2021; among males it reduced from 7.2% in 2017 to 6.0% in 2021 (OR=0.93; p<0.001). Among the 15 regions, only Bukedi Region (OR=1.04; p<0.001) and Northern Central Region (OR=1.02; p<0.001) had increases in severe malaria cases as a proportion of all malaria. Severe malaria cases increased at regional referral hospitals (OR 1.15; p<0.001) and private clinics (OR 1.04; p<0.001), all other health facility levels had significant reductions. Both private (OR 1.09; p<0.001) and public health facilities (OR 1.13; p<0.001) had increases.
Conclusion: The proportion of severe malaria cases consistently declined over the review period suggesting progress in the control and management of uncomplicated malaria. However, Bukedi and North Central regions experienced increases. The burden of severe malaria cases was much higher at regional referral hospitals and private clinics. Additional efforts to improve management of uncomplicated malaria in Bukedi and North Central regions and other high malaria transmission regions could reduce severe malaria in Uganda.
Introduction
Globally, the scale-up of malaria prevention and control measures has made a significant contribution to the fight against malaria, with notable gains between 2000 and 2020 resulting in a 36% reduction in mortality. Despite this decrease, the number of malaria cases that progress to severe causing malaria-related deaths remains high; In 2021, malaria caused an estimated 247 million clinical episodes and 619,000 deaths[1]. Severe malaria typically occurs due to delayed treatment of uncomplicated malaria[2]. It is multi-syndromic and often manifests as cerebral malaria, severe malaria anaemia, and respiratory distress with severe anaemia being the most common complication[3]. The distribution of severe malaria syndromes varies by age across transmission intensities, influenced mainly by changes in community-level immunity patterns with a high mortality in the absence of timely appropriate treatment[2, 3]. Severe malaria is usually concentrated in children aged under 5 years, with the number of cases increasing with transmission intensity[3].
In Uganda, severe malaria is responsible for 15–20% of hospital admissions and is the leading cause of mortality among children under 5 years[4]. Uganda ranks 8th to the global malaria mortality burden and this number is due to poor treatment outcomes of severe malaria[1]. The country has embraced a number of interventions over the years all aimed at malaria mortality reduction and elimination to near zero (<1 death per 100,000 population) by 2030[5]. These include but are not limited to: strengthening the test and treat policy and intensified malaria case management nationally. Other interventions targeting high malaria transmission areas include: integrated community case management of childhood illnesses like malaria, Indoor residual spraying for high malaria transmission districts, malaria chemoprevention for high transmission areas, and with hope of receiving malaria vaccine for the children in the near future[5].
Despite these interventions, malaria remains the largest contributor to morbidity and mortality in the country with approximately 19,600 deaths annually[1]. Determining describing and trends of severe malaria could help in the identification of regions and districts with a high risk of malaria deaths and the population groups at risk. This will support better allocation of resources and quantification of drugs and other supplies required in severe malaria case management all aimed at prevention of malaria mortality. We evaluated the trends and distribution of severe malaria cases to inform progress on current interventions.
Methods
Study setting
Uganda is divided into 15 health regions including: Acholi, Ankole, Bugisu, Bukedi, Bunyoro, Busoga, Kampala, Karamoja, Kigezi, Lango, North Central, South Central, Teso, Tooro, and West Nile. Malaria is highly endemic in 96% of Uganda. Regions of West Nile and Acholi have very high transmission intensity with malaria incidence above 450 cases/1000 population. Lango, Karamoja, Teso, Bukedi, and Busoga regions have medium transmission intensity (malaria incidence between 251–450 cases/1000 population). Low transmission intensity regions with malaria incidence between 101–250 cases/1000 population include: South central, North central, Kampala, Ankole, Tooro and Bunyoro regions. Kigezi region has a very low malaria transmission intensity with malaria incidence between 0–100 cases/1000 population.
Uganda applies a free healthcare system in public health facilities where drugs are provided free of charge[6]. Health facilities are categorized into levels based on the number of services they offer; Health center IIs are the lowest level and are not mandated to treat severe malaria, Health Center IIIs can treat severe malaria, however majority do not have hospitalization services which leave most of the severe malaria management to health center IV level, hospitals, and regional referral hospitals. These facilities are challenged by frequent stock outs of drugs required for the management of
severe malaria and supportive treatment like blood products and medical oxygen[7-9]. Management of severe malaria is also done at private low-level clinics.
Study design and data source
We conducted a descriptive analysis of facility-based severe malaria data from 2017 to 2021 in Uganda using the District Health Information System ver.2(DHIS2). As per the DHIS2, severe malaria is defined as a confirmed (by microscopy or rapid diagnostic tests) malaria admission at a health facility OR a malaria illness serious enough to be an immediate threat to the life of a patient with a positive blood film or RDT and any of the following cerebral malaria (impairment of consciousness), severe anaemia, hemoglobinuria, acute respiratory distress syndrome, abnormalities in blood coagulation, low blood pressure caused by cardiovascular collapse, acute kidney injury, hyper-parasitemia, and metabolic acidosis[2, 10].
The facility-based severe malaria data are routinely generated at health facilities. This data is captured in the inpatient registers. They are then aggregated into a health facility monthly report (paper form) capturing the entire severe malaria management cascade of confirmed malaria cases admitted and the malaria mortality cases. The data are then entered into a web-based reporting system (DHIS2) which can be accessed by the Ministry of Health (MoH) and other stakeholders. DHIS2 captures information for all the districts in the fifteen health Regions. The system is reviewed every 5 years to include any added administrative units and revised indicators. This explains the difference in the number of districts reviewed for the various years (from 2017–2019; 136 districts and from 2020–2021; 146 districts).
Study variables, data abstraction, and analysis
We used pivot tables to filter secondary data on selected indicators: inpatient malaria cases and total confirmed outpatient malaria cases from monthly disease surveillance reports (105 and 108) from 2017–2021 available in DHIS2. Data was extracted using Microsoft Excel for each year disaggregated into national and regional and district level data. We further obtained district population data from Uganda bureau of statistics (UBOS) for calculation of district severe malaria incidence. The proportions of severe malaria cases of the total confirmed malaria cases were then calculated for each year using severe malaria inpatient department (IPD) cases (numerator) and total outpatient department (OPD) cases (denominator).
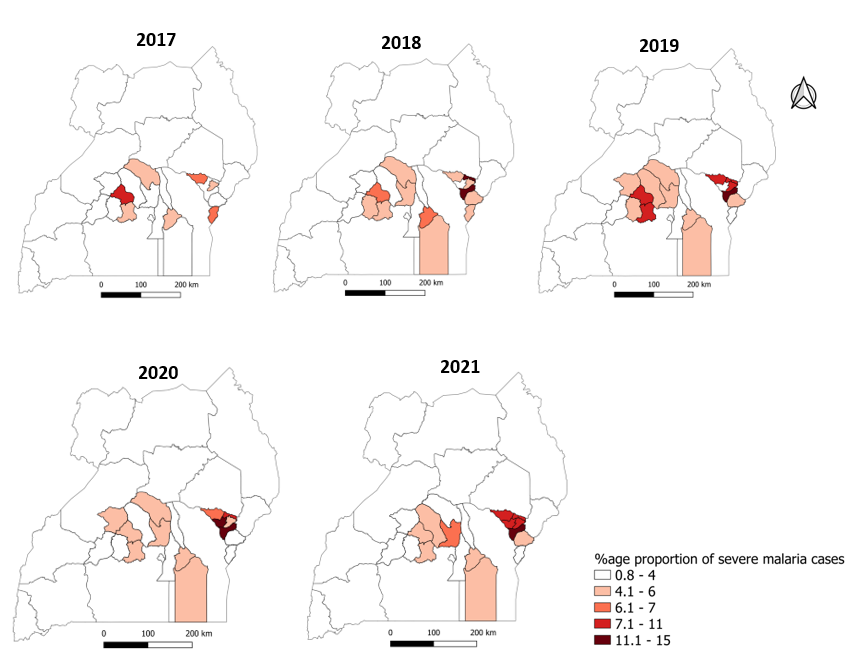
The trend was stratified by region, age, sex, health facility level, and health facility type. Trends in severe malaria proportions were tested for significance using logistic regression in Epi Info 7 software and level of significance was considered at a p–value <0.05. Choropleth maps for the regional severe malaria proportions and severe malaria incidence for the period from 2017 to 2021 were generated using Quantum Geographic Information System (QGIS). For the proportions map since we could not get an acceptable proportion, we based on data to make appropriate ranges with 1–4% being the least and 11.1–15% being the highest range. Similar assumptions were made for the ranges of severe malaria incidence on the choropleth maps.
Results
Trends in severe malaria as a proportion of all malaria cases, Uganda, 2017–2021 Overall, 2,957,672 severe malaria cases were reported in the 5year period reviewed. Severe malaria cases as a proportion of all malaria cases decreased by 10% annually from 7.0% (679,328/10,263,374) in 2017 to 5.0% (539,995/11,029,320) in 2021 (OR=0.90; 95% CI 0.90–0.91) (Figure 2).
The proportion among children <5 years reduced from 13% in 2017 to 10% in 2021 (OR=0.93; 95% CI 0.93–0.93) while that for >5 years reduced from 4.4% to 3.5% (OR=0.92; 95% CI 0.91–0.92) (Figure 3). Similarly, the proportion for females reduced from 6.1% in 2017 to 4.6% in 2021 (OR=0.91; 95% CI 0.91–0.91) while males reduced from 7.2% in 2017 to 6.0% in 2021 (OR=0.93; 95% CI 0.93–0.93) (Figure 4).
Severe malaria as a proportion of all malaria cases by health region, Uganda, 2017–2021
At regional level, Bukedi region and Northern Central regions had a significant increasing trend of severe malaria cases while all the rest had a reducing trend just like the national picture. Bukedi Region had a 4% increase in severe malaria cases for every increase in years (OR 1.04; 95% CI, 1.03–1.04) while Northern central regions had a 2% increase in severe malaria cases for every increase in years (OR 1.02, 95% CI, 1.01–1.02) (Figure 4). Lango region had the highest reduction in severe malaria cases of 22% for every increase in years (OR 0.78; 95% CI, 0.78–0.78) followed by Kampala region with a 20% reduction in severe malaria cases for every increase in years (OR 0.8; 95% CI; 0.79–0.81) (Figure 4).
Severe malaria as a proportion of all malaria cases by district level, Uganda, 2017–2021
To determine which specific districts contributing to the increasing trend in severe malaria cases for the Bukedi and North central regions, we analyzed trends for the districts in these regions. Budaka and Pallisa districts were contributing to the regional increase in severe malaria cases for Bukedi region. For North central region, Buvuma, Kyankwanzi, Luwero, Mukono and Nakaseke contributed to the increase in the trend of severe malaria cases in this region. The rest of the districts had a reducing trend in severe malaria cases over the years.
For Bukedi region, Budaka District had an 8% (OR 1.08; 95% CI 1.07–1.09) reduction in severe malaria cases for every increase in years. Similarly, Pallisa District had an 8% (OR 1.08; 95% CI 1.06–1.09) reduction in severe malaria cases for every increase in years. Additionally, for North central region, Luwero District had the highest increase in severe malaria trends with a 19% (OR 1.19; 95% CI 1.18–1.21) increase in trend for every increase in years. This was followed by Mukono District with a 17% (OR 1.17; 95% CI 1.15–1.18) increase, Buvuma District with 13% (OR 1.13; 95% CI 1.11–1.12) increase, Kyankwanzi District with 8% (OR 1.08; 95% CI 1.07–1.12) increase, Nakaseke District with 6% (OR 1.06; 95% CI 1.05–1.08) and Mityana District with 4% (OR 1.04; 95% CI 1.03–1.04) increase for every increase in years (Table 1).
Table 1: Significant odds ratios for the trend of severe malaria cases for Bukedi and North central regions of Uganda, 2017–2021 (OR; Odds ratio, CI: Confidence Interval)
| District | OR | CI | P-value | |
| Bukedi | Budaka | 1.08 | 1.07-1.09 | <0.001 |
| Busia | 0.76 | 0.76-0.77 | <0.001 | |
| Butaleja | 0.98 | 0.96-0.98 | <0.001 | |
| Butebo | 0.87 | 0.86-0.88 | <0.001 | |
| Kibuku | 0.86 | 0.84-0.86 | <0.001 | |
| Pallisa | 1.08 | 1.06-1.09 | <0.001 | |
| Tororo | 1.02 | 1.00-1.02 | <0.001 | |
| North Central | Buikwe | 0.97 | 0.96-0.97 | <0.001 |
| Buvuma | 1.13 | 1.11-1.15 | <0.001 | |
| Kassanda | 0.93 | 0.92-0.94 | <0.001 | |
| Kayunga | 0.93 | 0.92-0.94 | <0.001 | |
| Kiboga | 0.92 | 0.90-0.92 | <0.001 | |
| Kyankwanzi | 1.08 | 1.07-1.12 | <0.001 | |
| Luwero | 1.19 | 1.18-1.21 | <0.001 | |
| Mityana | 1.04 | 1.03-1.04 | <0.001 | |
| Mubende | 0.89 | 0.88-0.90 | <0.001 | |
| Mukono | 1.17 | 1.15-1.18 | <0.001 | |
| Nakaseke | 1.06 | 1.05-1.08 | <0.001 | |
| Nakasongola | 0.91 | 0.89-0.92 | <0.001 |
Spatial distribution of severe malaria as a proportion of all malaria cases by health region, Uganda, 2017–2021
During spatial analysis, a reduction in severe malaria proportions of the total confirmed malaria cases was evident for all regions over the years. However, an increasing trend in severe malaria proportions was observed for Bukedi and Northern central regions (Figure 2). Although North central showed a 2% increase in severe malaria proportions, this increase was too small to be evident on the regional map over time. Kigezi region showed a 9% overall decrease in severe malaria proportions, however, spatial distribution shows an increase in proportion from 4.1-6% in 2020 to 7.1–11% in 2021 (Figure 5).
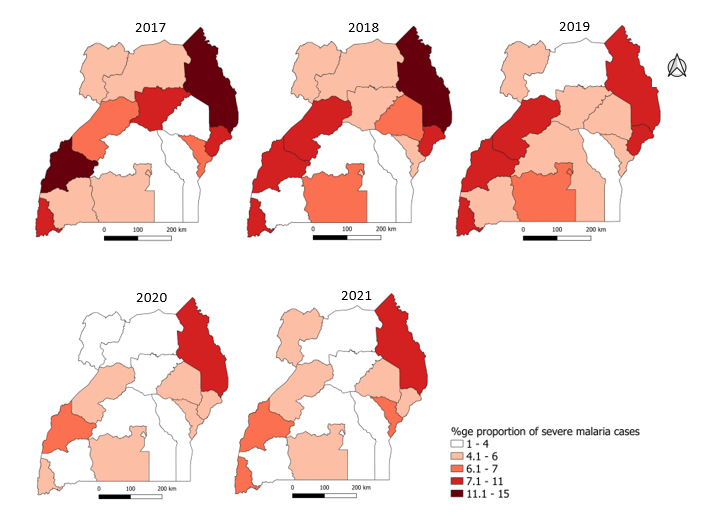
Specific districts contributed to the increasing severe malaria trend in North Central and Bukedi regions. The increase in trend was evident for Luwero District in North central region and for districts within Bukedi Region (Figure 5).
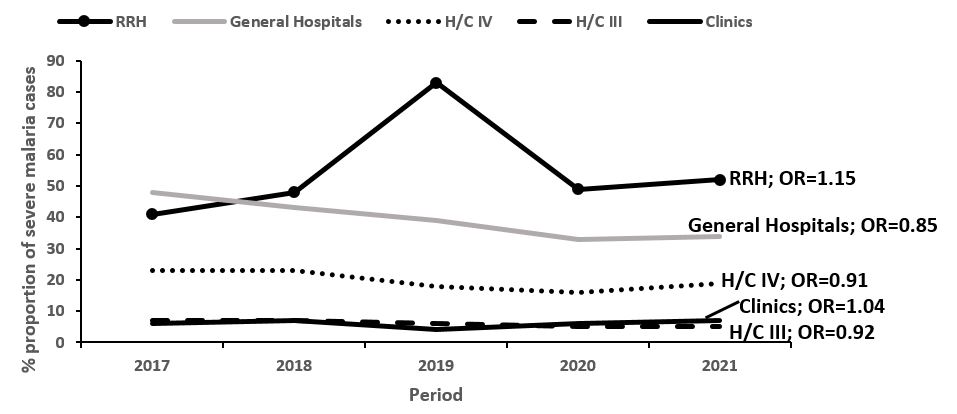
Trends of severe malaria as a proportion of all malaria cases by health facility level, Uganda, 2017–2021
The proportion of severe malaria cases increased significantly among regional referral hospitals with a 15% increase for every increase in years and private clinics with a 4% increase for every increase in years. Among the other health facility levels (General hospitals, Health center IV and Health center IIIs), severe malaria proportions significantly reduced (Figure 6).
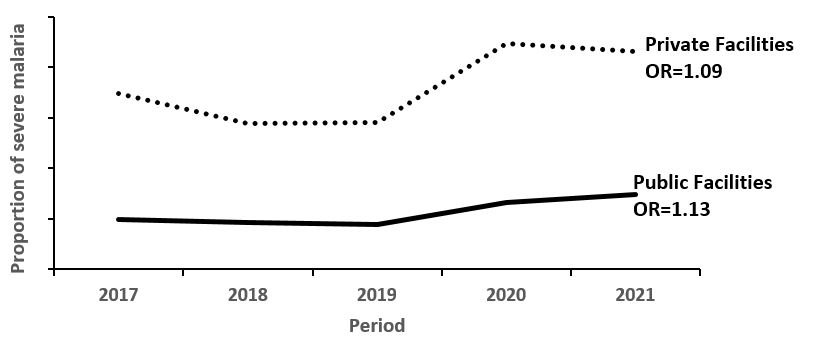
Trends of severe malaria as a proportion of all malaria cases by health facility ownership, Uganda, 2017–2021
Discussion
We highlight a general reduction in the proportion of malaria cases that progress to severe over the years nationally and for most of the regions. A similar trend was observed in all age categories most especially children below 5 years and in sex groups. For regions with an increasing severe malaria trend, specific districts were driving this trend. Looking at health facility type, only regional referral hospitals and private clinics had an increasing trend. With regard to health facility ownership, both private and public health facilities registered an increasing trend in severe malaria cases. Public health facilities had a higher annual increase of 13% compared to 9% annual increase in private facilities.
Our findings revealed an overall national decreasing trend in the proportion of malaria cases that progress to severe malaria, this trend was similar in 87% of the regions. The decrease in the proportion of malaria cases progressing to severe malaria suggests a general improvement in the quality of case management. This could be as a result of the on-gong integrated malaria management (IMM) trainings and onsite mentorships that target health workers at health facilities[10]. Further possible explanation for the observed trend could be related to increased coverage to social behavioral change communication (SBCC) networks and population exposure to malaria messages that has been previously associated with early health seeking behavior and timely referral of cases to facility for care[11]. Additional strategies implemented include integrated community case management (iCCM) of childhood illnesses including malaria that targets children <5 years, and relies entirely on village health teams[12].
This intervention ensures timely malaria treatment for the most burdened age group[3]. According to the Global Fund Mid-term Assessment, iCCM is operating in 78 districts of Uganda and has helped strengthen health and community systems. Additionally, regions receiving long-lasting insecticide treated nets (LLINs) and indoor residual spraying (IRS) have received an over 20% reduction in malaria burden among the <15year children[13]. A decrease in malaria burden could explain the decrease in severe malaria proportion since 15.9% of cases have been found to progress to severe disease[14]. Furthermore, the decreasing proportions could also be due to improved malaria treatment at health facilities as per a study to review adherence to malaria management guidelines by health care workers in the Busoga sub-region, eastern Uganda. This study revealed that adherence to malaria case management guidelines were good, but with gaps noted mainly in the private sector[15].
Regional referral hospitals and private clinics were found to have a significant increase in the trend of the proportion of severe malaria cases among other health facility levels with a 15% and 4% increase respectively. This could be due to the referral system in Uganda where complicated cases are referred to high level health facilities[16]. Those unable to reach the high-level health facilities due to transport challenges access low level private clinics near them. The reducing trend at low level health facilities could be due to frequent stock outs of required treatment options hence the need for referral to regional referrals and private clinics assured of antimalarial commodity stock and other related services for the management of severe malaria complications[17-19]. Equipping low level health facilities with adequate severe malaria treatment commodities could help decongest regional referral hospitals and private clinics.
Our findings revealed a higher increase in proportion of severe malaria in government health facilities (13%) compared to 9% in private health facilities. Private health facilities offer an important service in filling the gaps in healthcare delivery in Uganda with over 50% of sick children being first treated by primary level private health facilities[20, 21]. However, in cases of severe disease, patients seek care from government health facilities due to the perceived presence of healthcare providers and their high level of experience[21, 22]. Furthermore, a study conducted on utilization of public or private health providers after removal of user fee services revealed that the average expenditure for hospitalization is USD 7.6 per child[23]. And because a higher burden of disease has been noted among the poor with less access to healthcare services, this could explain the higher increase in proportion of severe malaria in public health facilities that offer free medical services [24]. Equipping the government health facilities with adequate quantities of severe malaria management supplies is critical in ensuring the proper management of patients and reduced mortality.
Although severe malaria generally showed a decreasing trend, an increasing trend was observed for Bukedi and North Central regions plus a few districts in Tooro, Kigezi and South-central regions. This could be explained by the waning immunity within the population due to reduced exposure to infective mosquito bites as a result of prolonged protection provided by IRS for Bukedi region. The Observed trend for north central and other districts in low and very low malaria transmission can be explained by the low malaria endemicity in this area that creates a low immune population that is more prone to severe form of disease[1, 3, 5]. The Malaria Indicator Survey (MIS) 2019 reported low parasite prevalence in north central Uganda suggesting a zone of low transmission intensity[25]. Low immune populations are characterized by malaria epidemics, complications and increased risk of deaths[2]. Scale up iCCM, IRS and SBCC interventions to regions with low malaria burden could reduce severe malaria proportions in these regions with reduced immunity to malaria.
Study limitations
The study used secondary data and as such analysis and exploration of other variables related to the severe malaria was not done. There are reporting challenges to this data which might affect the representativeness of these findings. (1) A few districts have suboptimal reporting rates below 80%, (2) a number of low-level private clinics that support in the treatment of severe malaria are not registered to report on this system or are registered but not reporting promptly. This highlights the possible underestimation of the severe malaria burden in the country.
Conclusion
The proportion of severe malaria cases consistently declined over the review period suggesting progress in the control and management of uncomplicated cases. However, Bukedi and North Central regions are still experiencing increases in severe malaria. The burden in treatment of severe malaria cases appears to be shifting from lower-level health facilities to regional referral hospitals and private clinics. We recommend additional efforts to improve the management of uncomplicated malaria in Bukedi and North Central regions and strengthening malaria case management generally most especially among children <5 years to reduce severe malaria in Uganda. A further recommend an investigation to determine factors associated with the increasing severe malaria cases for affected districts and for the high reduction in others.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
The authors appreciate the Ministry of Health for providing access to DHIS2 data that was used for this analysis. We further appreciate the National Malaria Control Division and other national malaria stakeholders for raising the questions that initiated this analysis.
Copyright and licensing
All material in the Uganda Public Health Bulletin is in the public domain and may be used and reprinted without permission. However, citation as to source is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
Acknowledgements
The authors appreciate the Ministry of Health for providing access to DHIS2 data that was used for this analysis. We further appreciate the National Malaria Control Division and other national malaria stakeholders for raising the questions that initiated this analysis.
References
- Organisation WH. World Malaria Report 2022. Geneva: 2022.
- Health CG. Division of Parasitic Diseases and Malaria 2022. Available from: https://www.cdc.gov/malaria/about/.
- WHO. World Malaria Report 2021.
- Malaria T. Uganda Malaria Facts, Target Malaria. Severe Malaria Observatory2022 1/11/2022]. Available from: https://www.severemalaria.org/countries/uganda.
- National Malaria Control Program MoHU. Uganda National Malaria Control Policy. . 2011. [Pg 8].
- Twikirize JM, O’Brien C. Why Ugandan rural households are opting to pay community health insurance rather than use the free healthcare services. International Journal of Social Welfare. 2012;21(1):66-78.
- Moffitt CA, Olupot-Olupot P, Onen JW, O’Brien N. Adherence to severe malaria treatment guidelines in children at a Ugandan regional hospital: a baseline assessment for a malaria treatment quality improvement project. Malaria Journal. 2023;22(1):1-8.
- Ippolito MM, Kamavu LK, Kabuya J-B, Tente C, Chileshe E, Wapachole M, et al. Risk factors for mortality in children hospitalized with severe malaria in northern Zambia: a retrospective case-control study. The American Journal of Tropical Medicine and Hygiene. 2018;98(6):1699.
- Kapesa A, Kweka EJ, Atieli H, Afrane YA, Kamugisha E, Lee M-C, et al. The current malaria morbidity and mortality in different transmission settings in Western Kenya. PloS one. 2018;13(8):e0202031.
- Health Mo. Integrated Management of Malaria Training Manual. 3rd Edition ed. Kampala, Uganda2019 November, 2019. 198 p.
- National Malaria Control Program MoHU. National Communication Strategy for Malaria Control in Uganda. Kampala, Uganda2015 December 2015. 41 p.
- Fund TG. Breaking Down Barriers-Uganda mid-term assessment. Geneva, Switzeland: 2021.
- Kigozi SP, Kigozi RN, Epstein A, Mpimbaza A, Sserwanga A, Yeka A, et al. Rapid shifts in the age-specific burden of malaria following successful control interventions in four regions of Uganda. Malaria journal. 2020;19(1):1-12.
- McDonald CR, Weckman AM, Richardson E, Hawkes MT, Leligdowicz A, Namasopo S, et al. Sex as a determinant of disease severity and clinical outcome in febrile children under five presenting to a regional referral hospital in Uganda. Plos one. 2022;17(10):e0276234.
- Mpimbaza A, Babikako H, Rutazanna D, Karamagi C, Ndeezi G, Katahoire A, et al. Adherence to malaria management guidelines by health care workers in the Busoga sub-region, eastern Uganda. Malaria Journal. 2022;21(1):1-15.
- Mbonye AK, Buregyeya E, Rutebemberwa E, Clarke SE, Lal S, Hansen KS, et al. Referral of children seeking care at private health facilities in Uganda. Malaria journal. 2017;16(1):1-11.
- Sundararajan R, Mwanga-Amumpaire J, Adrama H, Tumuhairwe J, Mbabazi S, Mworozi K, et al. Sociocultural and structural factors contributing to delays in treatment for children with severe malaria: a qualitative study in southwestern Uganda. The American journal of tropical medicine and hygiene. 2015;92(5):933.
- Zalwango GM. Risk factors for death among children with severe malaria in Namutumba District, Uganda, September 2021-February 2022. 2022.
- Rahimi A, Kassam R, Dang Z, Sekiwunga R. Challenges with accessing health care for young children presumed to have malaria in the rural district of Butaleja, Uganda: a qualitative study. Pharmacy Practice (Granada). 2019;17(4).
- Maitland K. Management of severe paediatric malaria in resource-limited settings. BMC Med. 2015;13(42).
- Rutebemberwa E, Pariyo G, Peterson S, Tomson G, Kallander K. Utilization of public or private health care providers by febrile children after user fee removal in Uganda. Malaria journal. 2009;8(1):1-9.
- Mwanga-Amumpaire J, Ndeezi G, Källander K, Obua C, Migisha R, Nkeramahame J, et al. Capacity to provide care for common childhood infections at low-level private health facilities in Western, Uganda. PloS one. 2021;16(10):e0257851.
- Nabyonga Orem J, Mugisha F, Okui AP, Musango L, Kirigia JM. Health care seeking patterns and determinants of out-of-pocket expenditure for malaria for the children under-five in Uganda. Malaria journal. 2013;12(1):1-11.
- Kiwanuka S, Ekirapa E, Peterson S, Okui O, Rahman MH, Peters D, et al. Access to and utilisation of health services for the poor in Uganda: a systematic review of available evidence. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2008;102(11):1067-74.
- National Malaria Control Program MoHU. Malaria Indicator Survey Kampala, Uganda: Uganda Bureau of Statistics; 2018-2019 March 2020. 190 p


Comments are closed.