Trends and spatial distribution of pneumonia admissions and deaths among children under five years in Uganda, 2013-2021
Authors: Mercy Wendy Wanyana1*, Patrick King1, Richard Migisha1, Institutional affiliations: 1Uganda Public Health Fellowship Program, Uganda National Institute of Public Health, Kampala, Uganda *Correspondence: Email: mwanyana@uniph.go.ug, Tel: +256779207928
Summary Background: Pneumonia is the second leading cause of hospital admissions and deaths among children <5 years in Uganda. While the pneumococcal conjugate vaccine was introduced to the routine immunisation schedule in 2013, little is known about the country’s progress in reducing pneumonia admissions and deaths since then. We described the trends and spatial distribution of pneumonia hospital admissions and mortality among children <5 years in Uganda during 2013–2021. Methods: We analysed aggregate secondary data on pneumonia admissions and deaths from the District Health Information System 2, 2013–2021. Pneumonia admissions and mortality rates were calculated per 100,000 children <5 years at national, regional, and district levels. Logistic regression was used to assess the significance of the trend. To contextualize the findings, we also collected data on reporting rates, defined as the percentage of complete submitted monthly reports over the study period divided by the number of expected reports. Results: There were 753,978 pneumonia admissions and 13,632 deaths during 2013–2021 among children <5 years. Reporting rates for admissions and death during this period increased from 78% to 92%. Annual admissions decreased by 4% (OR=0.96, 95% CI: 0.96-0.96) from 2013 to 2021. Northern Region had the smallest decline (OR=0.99, 95% CI: 0.99-0.99) while Central Region had the largest (OR=0.92, 95% CI: 0.92-0.92). Admission rates were highest (1,900 to 14,209 /100,000) in Kotido and Gulu districts over all 9 years. Annual mortality rates decreased by 6% (OR=0.94, 95% CI: 0.93-0.95) over the study period, with the smallest decline in Eastern Region (OR=0.95, 95% CI: 0.94-0.96) and the largest in Central Region (OR=0.93, 95% CI: 0.92-0.94). Gulu District had the highest mortality rates (40 to 110/100,000) over all 9 years. Conclusion: Both hospital admissions and mortality from pneumonia among children <5 years declined during 2013-2021 in Uganda despite increases in reporting. Existing interventions should be intensified to further accelerate the declines.
Background
Pneumonia, a largely preventable disease persists as a major public health problem among children <5 years of age. By 2019, pneumonia was the leading infectious cause of death among children <5 years accounting for 14% of all deaths with one child dying of pneumonia every 39 seconds(1). Fifty percent of the pneumonia cases and deaths are reported in Sub-Saharan Africa with an annual incidence of 10,493 and mortality of 253 per 100,000 children <5 years of age(2).
Even with marked reductions in pneumonia globally (from 178 to 138 million cases annually), reductions in Sub-Saharan Africa have been much slower(2,3). By 2020, the prevalence of pneumonia among children <5 years in Eastern Africa was 34,000 per 100,000 children <5 years of age(4). Furthermore, although pneumonia incidence and mortality reduced, there was a three-fold increase in pneumonia admissions in Sub-Saharan Africa in this age group(3).
Particulary in Uganda pneumonia remains the second leading cause of all hospital admissions among children <5 years of age(5). This places a substantial burden on the health system as pneumonia accounts for a significant proportion of paediatric admissions. An economic burden is also placed on the already impoverished families. On average Ugandan households spend 62 US dollars per hospitalised episode of pneumonia(6).
To avert this burden, Uganda joined the rest of the world in 2013 to implement various global initiatives such as the integrated Global Action Plan for the Prevention and Control of Pneumonia and Diarrhoea (GAPPD)(7). This initiative led to the introduction of pneumococcal conjugate vaccine introduced to the routine immunisation schedule.
This was to be complimented by other low-cost interventions including exclusive breastfeeding for the first six months and continued breastfeeding with appropriate complementary feeding thereafter, use of simple, standardized guidelines for the identification and treatment of pneumonia in the community through integrated community case management of childhood illnesses and reduction of household air pollution with improved stoves.
With these interventions, Uganda like the rest of the world targeted to reduce the incidence of pneumonia requiring admission by 75% in children <5 years of age compared to 2010 levels and reduce mortality from pneumonia in children <5 years of age to fewer than 3 per 1000 live births by 2025(7).
Little is documented on Uganda’s progress towards these goals.
Previous studies(8,9) conducted in Uganda assessed prevalence of pneumonia at specific time points hence less informative about the progress over time. Additionally, these studies were conducted in particular regions and may not be generalisable to the entire country or show any spatial differences if any exist. We assessed the trends and spatial distribution of pneumonia admissions and mortality rate among children <5 Uganda, 2013-2021.
Methods
We conducted a secondary analysis of pneumonia surveillance data generated from the entire Uganda and stored in the District Health Information System 2 (DHIS-2). Uganda is a low-income country located in Eastern Africa with 20% of its population aged <5 years.
The DHIS-2 system collects data on priority diseases, conditions, and events of public health importance like pneumonia based on the Integrated Disease Surveillance and response guidelines(10). We specifically abstracted aggregate data of both pneumonia admissions and deaths from the inpatient monthly reports (Health Management Information System forms (HMIS) 108) from 2013 to 2021 into excel and imported into Epi info 7 software for analysis.
Using the aggregate data on pneumonia admissions and deaths we calculated the annual incidence of pneumonia admissions and mortality rate using population data from the Uganda Bureau of Statistics as a denominator. Facility based mortality rates were calculated as the proportion of pneumonia cases who died following admission. Pneumonia admissions were defined as hospital stay due to pneumonia based on the ICD-10 framework as a primary diagnosis. Pneumonia deaths were defined as in-patient deaths with pneumonia as the main cause of death.
We calculated annual incidence of pneumonia admissions, overall mortality, and facility-based mortality rates at national, regional, and facility levels. We used line graphs to describe national and regional trends. Additionally, logistic regression analysis was conducted to evaluate the overall trend using Epi info 7 software. Choropleth maps drawn using QGIS software were used to show the spatial distribution of pneumonia admissions and mortality in the country. To further contextualize the findings, we also abstracted data on reporting rates, calculated as the percentage of complete submitted monthly reports over the study period divided by the number of expected reports.
Our study utilized routinely generated aggregated surveillance data with no personal identifiers in health facility in-patient monthly reports, Ministry of Health (MoH) through the DHIS-2. The MoH of Uganda through the office of the Director General Health Services gave approval to access data for pneumonia admissions and death from the DHIS-2. We stored the abstracted data set in a password-protected computer and only shared it with the investigation team.
In addition, The Office of the Associate Director for Science, U.S. Centers for Disease Control and Prevention, determined that this study was not a human subjects research with the primary intent of improving use of surveillance data to guide public health planning and practice.
Results
National incidence of pneumonia admissions among children under 5 years, Uganda, 2013-2021
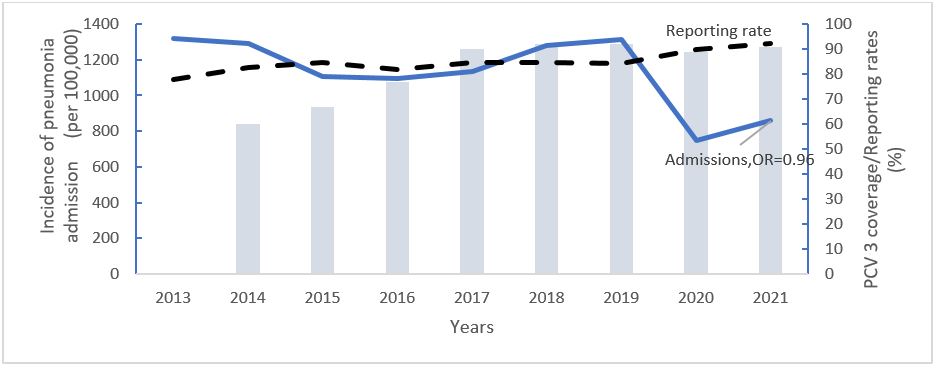
Over the study period, there was a total of 753,978 admitted pneumonia cases. The PCV vaccine coverage increased from 60% to 92% (Figure 1).
The national average incidence of pneumonia admissions was 1,127 (Range:750 to 1,319) admitted cases per 100,000 children <5 years, with the highest in 2019 (1,319 cases per 100,000). Overall, there was a 4% decline in the incidence of pneumonia admissions among children <5 years (OR= 0.96,95% CI: 0.956-0.957), p=<0.001 (Figure 1).
Overall trends in the overall pneumonia mortality, among children under 5 years, Uganda, 2013-2021
During the study period, there were 13,632 deaths occurred among children <5 years admitted with pneumonia. The PCV vaccine coverage increased from 60% to 92% (Figure 1).
The national average overall pneumonia mortality rate was 21 (Range: 26 to 14) deaths per 100,000 children <5 years with the highest in 2013(26). Overall, there was a 6% decline in the overall pneumonia mortality among children <5 years (OR= 0.93,95% CI: 0.93-0.95), p=<0.001(Figure 2).

Pneumonia facility-based mortality rate among children under 5 years, Uganda, 2013-2021
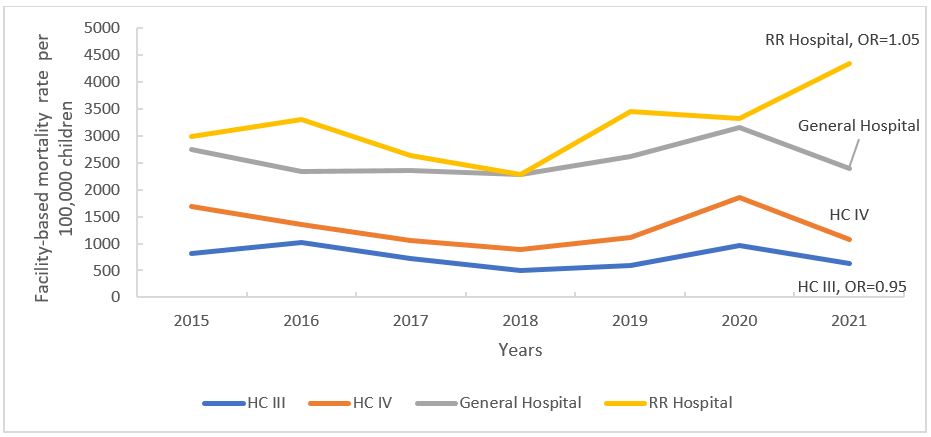
The average national pneumonia facility-based mortality rate was 1,805 (Range: (Range:1, 612 to 2,097) per 100,000 children <5 years, with the highest in 2020 (2,097 per 100,000 children).
Overall, the pneumonia facility-based mortality rate declined by 2% (OR:0.98,95% CI:0.97-0.99). Changes in pneumonia facility-based mortality rate varied with no changes observed at health centre IV (OR:0.97,95% CI:0.95-1.00), p=0.058 and general hospital level (OR:1.00,95% CI:0.99-1.02), p=0.288. At health centre III level, pneumonia facility-based mortality rate declined (OR:0.95,95% CI:0.93-0.99), while it increased at the regional referral level (OR:1.05,95% CI:1.02-1.08) (Figure 3).
Regional trends of incidence of pneumonia admissions, overall mortality rate, and facility-based mortality rate among children under 5 years, Uganda, 2013-2021
Pneumonia admissions significantly declined across all regions (Table 1).
The greatest decline in the incidence of pneumonia admissions was in the central region (OR:0.92, CI: 0.920-0.924, P<0.001) while the smallest decline was in the northern region (OR:0.99,95% CI:0.99-0.99, P<0.001). Unlike pneumonia admissions, facility-based mortality rate only declined in the northern region, 7% (0R=0.93,95% CI:0.919-0.943).
Overall, pneumonia mortality significantly declined across all regions. The greatest decline in pneumonia mortality was in the central region (OR:0.92, CI: 0.912-0.943, P<0.001) while the smallest decline was in the eastern region (OR:0.95,95% CI:0.936-0.963, P<0.001) (Table 1).
Table 1: Regional trends of incidence pneumonia admissions, overall mortality rate, and facility-based mortality, among children under 5 years, Uganda, 2013-2021
| Incidence of pneumonia admissions | Facility based mortality rate | Overall mortality | |||||||
| Region | OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value |
| Central | 0.92 | 0.92 – 0.92 | <0.001 | 1.00 | 0.99-1.020 | 0.332 | 0.93 | 0.91-0.94 | <0.001 |
| Eastern | 0.95 | 0.94-0.95 | <0.001 | 1.00 | 0.99-1.019 | 0.603 | 0.95 | 0.94-0.96 | <0.001 |
| Northern | 0.99 | 0.99-0.99 | <0.001 | 0.93 | 0.92-0.94 | <0.001 | 0.93 | 0.92-0.94 | <0.001 |
| Western | 0.95 | 0.95-0.95 | <0.001 | 0.99 | 0.98-1.00 | 0.264 | 0.94 | 0.93-0.96 | <0.001 |
Spatial distribution of incidence of pneumonia admissions and overall mortality among children under 5 years, Uganda, 2013-2021
Incidence of pneumonia admissions among children < 5 years were highest (1,900 to 14,209 /100,000) in Kotido and Gulu districts over all 9 years (Figure 4).
Gulu district had the highest mortality rates (40 to 110/100,000) over all 9 years. Kasese district had consistently high incidence of pneumonia admissions and overall mortality rates.
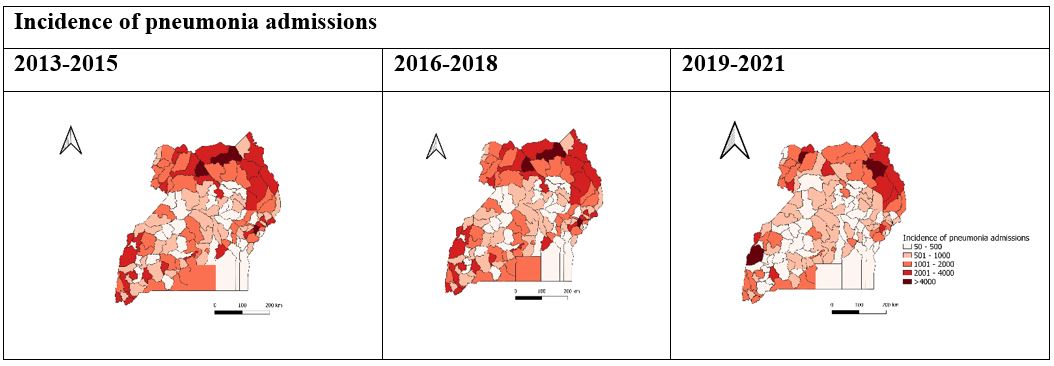
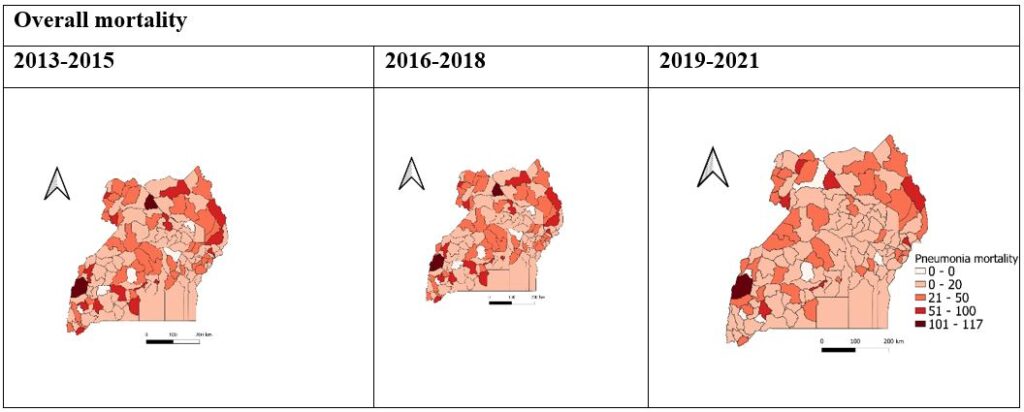
Figure 4: Spatial distribution of incidence of pneumonia admissions and overall mortality among children <5 years, Uganda, 2013-2021
Discussion
We described the trends and spatial distribution of pneumonia hospital admissions and mortality among children <5 years in Uganda during 2013–2021.Our findings indicate declines (<10%) in the incidence of pneumonia admissions, overall mortality, and facility-based mortality rates over the 9-year period.
These declines differed across region, with the lowest decline in the incidence of pneumonia admissions and mortality observed in the northern region and eastern regions respectively. Declines in the pneumonia facility-based mortality rate were only observed at the health centre III level and in northern region. Pneumonia facility-based mortality rate increased at regional referral hospital level. Like the global trend, our findings indicate a reduction in pneumonia admissions over the 9-year period(3).
However, declines in the incidence in pneumonia admissions reported in this study were below those previously observed in other studies in African Countries where the Pneumococcal Vaccine(PCV) vaccine was introduced(11,12). A study in Burkina Faso(12) indicated 34% reduction in pneumonia admissions among children <5, five years following the introduction of PCV.
In another study in Zambia(11) pneumonia admissions declined by 37.8% and 28.8% among children aged <1 year and 1–4 years, respectively. Previous studies conducted among children<5 years with severe pneumonia(13,14) indicated the presence of other pneumonia-causing organisms that the PCV vaccine does not protect against such as the Klebsiella species and other viral pneumonia-causing organisms.
These could contribute to slower declines in pneumonia admissions despite the high PCV coverage. Additionally, the observed declines in pneumonia admissions in 2020 could be attributed to the limited access to healthcare during the COVID-19 lockdown leading to fewer documented pneumonia admissions and not actual declines in pneumonia requiring admission(15).
Pneumonia mortality declines in both overall and facility-based mortality reported in this study were below those observed in other studies in Africa where the pneumonia vaccine was introduced. A study in South Africa(16) indicated a 33% and 26% reduction in pneumonia mortality among children aged 1 to 11 months and 1 to 4 years respectively.
Anticipated gains in reduction of hospital pneumonia mortality could be prevented by the presence of overlapping risk factors previously documented in Uganda. These include undernutrition, delayed health care seeking, co-morbidities such as HIV, limited access to oxygen, and stock out of essential treatments(17–21). Additionally, declines in pneumonia mortality may vary across countries due to differences in coding of the cause of death(22).
Notably, the decline in the facility-based mortality rate were far below (less than half) the decline in the overall mortality rate. This indicates a slower progress in the health care system’s capacity to reduce pneumonia mortality among children <5 years(23).
Existing gaps in timely seeking of appropriate treatment and access to parenteral antibiotics and oxygen (where necessary) and treatment failure resulting from anti-microbial resistance in developing countries like Uganda may contribute to slower declines in the facility-based mortality rate(24).
In Uganda, critical children are more likely to complete the referral process,(25) it is therefore not surprising that the facility based mortality rate at regional referral hospital level increased overtime.
Regional differences in the trend of incidence of pneumonia admissions, pneumonia overall mortality, and facility-based mortality rate were observed. The lowest declines in the incidence of pneumonia incidence and mortality were observed in the northern and eastern regions. These regions are characterised with poverty and poor housing, all of which are associated with an increased likelihood of pneumonia requiring admission and mortality(26,27).
Limitations
Our findings should be interpreted with the following limitation. We used in-patient data which could lead to underestimation of the true pneumonia mortality due to the exclusion of community deaths. Secondly, we used aggregate secondary data which lacked key variables to further explore trends across sub categories within this age group.
Conclusion
We highlight declines in the incidence of pneumonia admissions, overall mortality rate, and facility-based rate over the nine years following the introduction of the PCV vaccine in Uganda. Existing interventions should be intensified to further accelerate the decline in order to achieve set targets.
Conflict of interest
The authors declare that they had no conflict of interest.
Acknowledgments
We would like to thank the Ministry of Health for providing access to DHIS2 data that was used for this analysis. We appreciate the technical support provided by the Division of Surveillance, Information and Knowledge Management. Finally, we thank the US-CDC for supporting the activities of the Uganda Public Health Fellowship Program (UPHFP).
Copyright and licensing
All materials in the Uganda National Institute of Public Health Quarterly Epidemiological Bulletin is in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form
References 1. Perin J, Mulick A, Yeung D, Villavicencio F, Lopez G, Strong KL, et al. Global, regional, and national causes of under-5 mortality in 2000-19: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet Child Adolesc Heal. 2022 Feb;6(2):106–15. 2. Troeger CE, Khalil IA, Blacker BF, Biehl MH, Albertson SB, Zimsen SRM, et al. Quantifying risks and interventions that have affected the burden of lower respiratory infections among children younger than 5 years: an analysis for the Global Burden of Disease Study 2017. Lancet Infect Dis [Internet]. 2020 Jan 1;20(1):60–79. Available from: https://doi.org/10.1016/S1473-3099(19)30410-4 3. McAllister DA, Liu L, Shi T, Chu Y, Reed C, Burrows J, et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Glob Heal. 2019 Jan;7(1):e47–57. 4. Beletew B, Bimerew M, Mengesha A, Wudu M, Azmeraw M. Prevalence of pneumonia and its associated factors among under-five children in East Africa: a systematic review and meta-analysis. BMC Pediatr. 2020 May;20(1):254. 5. MoH M of HU. Ministry of Health Annual Sector Performance Report 2020/2021 [Internet]. Kampala, Uganda; 2021. Available from: http://library.health.go.ug/publications/performance-management/ annual-health-sector-performance-report-financial-year-202021 6. Ekirapa-Kiracho E, De Broucker G, Ssebagereka A, Mutebi A, Apolot RR, Patenaude B, et al. The economic burden of pneumonia in children under five in Uganda. Vaccine X. 2021 Aug;8:100095. 7. WHO (World Health Organisation). Ending preventable child deaths from pneumonia and diarrhoea by 2025: the integrated global action plan for pneumonia and diarrhoea (GAPPD). 2013; 8. Kiconco G, Turyasiima M, Ndamira A, Yamile OA, Egesa WI, Ndiwimana M, et al. Prevalence and associated factors of pneumonia among under-fives with acute respiratory symptoms: a cross sectional study at a Teaching Hospital in Bushenyi District, Western Uganda. Afr Health Sci. 2021 Dec;21(4):1701–10. 9. Ma C, Gunaratnam LC, Ericson A, Conroy AL, Namasopo S, Opoka RO, et al. Handheld Point-of-Care Lactate Measurement at Admission Predicts Mortality in Ugandan Children Hospitalized with Pneumonia: A Prospective Cohort Study. Am J Trop Med Hyg. 2019 Jan;100(1) :37–42. 10. MoH (Minstry of Health Uganda). National Technical Guidelines for Integrated Disease Surveillance and Response Third Edition [Internet]. 2021. Available from: https://www.afro. who.int/sites/default/files/2021-09/2_Uganda_3rd_IDSR_Tech_Guideline_PrintVersion_10Sep2021.pdf 11. Mpabalwani EM, Lukwesa-Musyani C, Imamba A, Nakazwe R, Matapo B, Muzongwe CM, et al. Declines in Pneumonia and Meningitis Hospitalizations in Children Under 5 Years of Age After Introduction of 10-Valent Pneumococcal Conjugate Vaccine in Zambia, 2010–2016. Clin Infect Dis [Internet]. 2019 Sep 5;69(Supplement_2):S58–65. Available from: https://doi.org/10.1093/cid/ciz456 12. Kaboré L, Ouattara S, Sawadogo F, Gervaix A, Galetto-Lacour A, Karama R, et al. Impact of 13-valent pneumococcal conjugate vaccine on the incidence of hospitalizations for all-cause pneumonia among children aged less than 5 years in Burkina Faso: An interrupted time-series analysis. Int J Infect Dis [Internet]. 2020 Jul 1;96:31–8. Available from: https://doi.org/10.1016/j.ijid.2020.03.051 13. Nantanda R, Hildenwall H, Peterson S, Kaddu-Mulindwa D, Kalyesubula I, Tumwine JK. Bacterial aetiology and outcome in children with severe pneumonia in Uganda. Ann Trop Paediatr. 2008 Dec;28(4):253–60. 14. Nantanda R, Tumwine JK, Ndeezi G, Ostergaard MS. Asthma and Pneumonia among Children Less Than Five Years with Acute Respiratory Symptoms in Mulago Hospital, Uganda: Evidence of Under-Diagnosis of Asthma. PLoS One [Internet]. 2013 Nov 29;8(11):e81562. Available from: https://doi.org/10.1371/journal.pone.0081562 15. Burt JF, Ouma J, Lubyayi L, Amone A, Aol L, Sekikubo M, et al. Indirect effects of COVID-19 on maternal, neonatal, child, sexual and reproductive health services in Kampala, Uganda. BMJ Glob Heal [Internet]. 2021;6(8). Available from: https://gh.bmj.com/content/6/8/e006102 16. Kleynhans J, Tempia S, Shioda K, von Gottberg A, Weinberger DM, Cohen C. Estimated impact of the pneumococcal conjugate vaccine on pneumonia mortality in South Africa, 1999 through 2016: An ecological modelling study. PLOS Med [Internet]. 2021 Feb 16;18(2):e1003537. Available from: https://doi.org/10.1371/journal.pmed.1003537 17. Iroh Tam P-Y, Wiens MO, Kabakyenga J, Kiwanuka J, Kumbakumba E, Moschovis PP. Pneumonia in HIV-exposed and Infected Children and Association With Malnutrition. Pediatr Infect Dis J [Internet]. 2018;37(10):1011–3. Available from: http://europepmc.org/abstract/MED/29505479 18. Banga D, Baren M, Ssonko NV, Sikakulya FK, Tibamwenda Y, Banga C, et al. Comorbidities and Factors Associated with Mortality among Children under Five Years Admitted with Severe Acute Malnutrition in the Nutritional Unit of Jinja Regional Referral Hospital, Eastern Uganda. Int J Pediatr. 2020;2020:7809412. 19. Källander K, Hildenwall H, Waiswa P, Galiwango E, Peterson S, Pariyo G. Delayed care seeking for fatal pneumonia in children aged under five years in Uganda: a case-series study. Bull World Health Organ. 2008 May;86(5):332–8. 20. Nabwire J, Namasopo S, Hawkes M. Oxygen Availability and Nursing Capacity for Oxygen Therapy in Ugandan Paediatric Wards. J Trop Pediatr [Internet]. 2018 Apr 1;64(2):97–103. Available from: https://doi.org/10.1093/tropej/fmx033 21. Masters SH, Burstein R, DeCenso B, Moore K, Haakenstad A, Ikilezi G, et al. Pharmaceutical Availability across Levels of Care: Evidence from Facility Surveys in Ghana, Kenya, and Uganda. PLoS One [Internet]. 2014 Dec 11;9(12):e114762. Available from: https://doi.org/10.1371/journal.pone.0114762 22. de Oliveira LH, Shioda K, Valenzuela MT, Janusz CB, Rearte A, Sbarra AN, et al. Declines in Pneumonia Mortality Following the Introduction of Pneumococcal Conjugate Vaccines in Latin American and Caribbean Countries. Clin Infect Dis an Off Publ Infect Dis Soc Am. 2021 Jul;73(2):306–13. 23. Souris M, Gonzalez J-P. COVID-19: Spatial analysis of hospital case-fatality rate in France. PLoS One [Internet]. 2020 Dec 15;15(12):e0243606. Available from: https://doi.org/10.1371/journal.pone.0243606 24. Graham SM, English M, Hazir T, Enarson P, Duke T. Challenges to improving case management of childhood pneumonia at health facilities in resource-limited settings. Bull World Health Organ. 2008 May;86(5):349–55. 25. Nanyonjo A, Bagorogoza B, Kasteng F, Ayebale G, Makumbi F, Tomson G, et al. Estimating the cost of referral and willingness to pay for referral to higher-level health facilities: a case series study from an integrated community case management programme in Uganda. BMC Health Serv Res [Internet]. 2015;15(1):347. Available from: https://doi.org/10.1186/s12913-015-1019-5 26. Atamanov A, Malasquez Carbonel EA, Masaki T, Myers CA, Granguillhome Ochoa R, Sinha N. Uganda Poverty Assessment: Strengthening Resilience to Accelerate Poverty Reduction. 2022. 27. Azab SFAH, Sherief LM, Saleh SH, Elsaeed WF, Elshafie MA, Abdelsalam SM. Impact of the socioeconomic status on the severity and outcome of community-acquired pneumonia among Egyptian children: a cohort study. Infect Dis Poverty [Internet]. 2014;3(1):14. Available from: https://doi.org/10.1186/2049-9957-3-14


Comments are closed.